Pseudosarcomatous Fibroblastic Proliferations
Elizabeth A. Montgomery, MD
Key Facts
Terminology
Nodular fasciitis: Rapidly growing myofibroblastic proliferation that is often cellular and mitotically active, but behaves in a benign fashion
Intravascular fasciitis: Rare variant of nodular fasciitis arising in association with small- and medium-sized vessels
Cranial fasciitis: Variant of nodular fasciitis involving soft tissues of scalp and underlying skull in infants
Proliferative fasciitis/myositis: Subcutaneous (fasciitis) or intramuscular (myositis) proliferation of ganglion-like cells in a background of myofibroblasts similar to those seen in nodular fasciitis
Ischemic fasciitis: Proliferation composed of zones of fat and fibrinoid necrosis with ingrowth of capillaries, fibroblasts, and myofibroblasts
Clinical Issues
Excellent prognosis: All these lesions are benign and typically do not recur even after incomplete excision
Recurrence should prompt re-review of prior sample to ensure initial diagnosis was correct
Microscopic Pathology
Myofibroblastic differentiation results in expression of “smooth muscle” immunohistochemical markers
Top Differential Diagnoses
Fibrous histiocytoma (dermatofibroma)
Neurofibroma
Fibromatosis
Malignant fibrous histiocytoma (undifferentiated pleomorphic sarcoma)
Leiomyosarcoma
TERMINOLOGY
Abbreviations
Nodular fasciitis (NF)
Synonyms
Pseudosarcomatous fasciitis (nodular fasciitis)
Subcutaneous pseudosarcomatous fibromatosis (nodular fasciitis)
Atypical decubital fibroplasia (ischemic fasciitis)
Definitions
Nodular fasciitis: Rapidly growing myofibroblastic mass-forming proliferation that is often cellular and mitotically active, but behaves in a benign fashion
Intravascular fasciitis: Rare variant of nodular fasciitis arising in association with small- and medium-sized vessels
Cranial fasciitis: Variant of nodular fasciitis involving soft tissues of scalp and underlying skull in infants
Proliferative fasciitis/myositis: Tumefactive subcutaneous (fasciitis) or intramuscular (myositis) proliferation featuring ganglion-like fibroblasts in a background of myofibroblasts similar to those seen in nodular fasciitis
Ischemic fasciitis: Pseudosarcomatous proliferation composed of zones of fat and fibrinoid necrosis with zonal ingrowth of capillaries, fibroblasts, and myofibroblasts
Initially described as tumefactive pressure sore arising over bony prominences in debilitated patients, but some examples do not fit this profile
CLINICAL ISSUES
Epidemiology
Incidence
All are uncommon; nodular fasciitis is most common among them
Age
Nodular fasciitis: Most patients are in their 3rd and 4th decades
Intravascular fasciitis: Most patients are in their 3rd and 4th decades
Cranial fasciitis: Infants in peripartum period
Proliferative fasciitis: Middle-aged and older adults; rare in children
Ischemic fasciitis: Elderly patients
Gender
No predilection
Site
Nodular fasciitis: Classic site is forearm
Intravascular fasciitis: Classic sites are distal extremities (especially fingers) and head and neck
Cranial fasciitis: Head
Proliferative fasciitis: Classic site is forearm
Ischemic fasciitis: Classic sites are overlying sacral promontory or greater trochanter
Presentation
All of these pseudosarcomatous processes present as mass lesions, usually painless
Most lesions: 1-3 cm
Ischemic fasciitis lesions can be large
Treatment
Simple excision is curative
Prognosis
Excellent; all of these lesions are benign and typically do not recur
Recurrence should prompt review of prior sample to ensure that initial diagnosis was correct
IMAGE FINDINGS
General Features
Imaging generally shows well-marginated subcutaneous process
Exception: Proliferative fasciitis tracks along connective tissue septa
MACROSCOPIC FEATURES
General Features
Well-marginated but unencapsulated lesions
White to gelatinous cross section
Ischemic fasciitis can feature areas of hemorrhage
Size
Most 2-3 cm (exception is ischemic fasciitis, which can attain large sizes)
MICROSCOPIC PATHOLOGY
Histologic Features
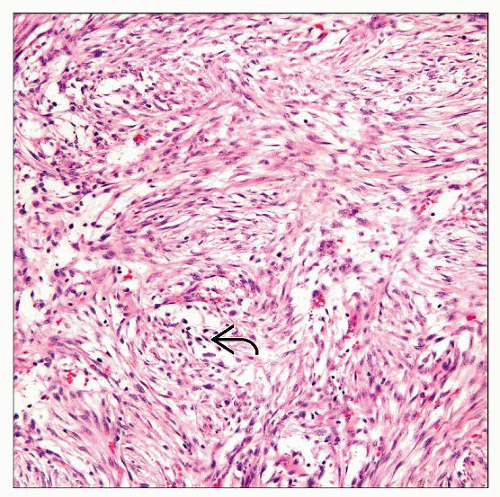
Nodular fasciitis
Loose storiform pattern with tissue culture appearance, variable myxoid stroma, cystic spaces, strands of keloid-like collagen
Osteoclast-like giant cells common (see in most lesions if sought; can be enhanced by CD68 staining)
Scattered lymphocytes but negligible plasma cells
Extravasated erythrocytes unassociated with hemosiderin deposition
3 reported forms: Myxoid, cellular, fibrous
Loose correlation with duration of lesions
Myxoid lesions often have been resected within 10 days of coming to clinical attention
Cellular and fibrous forms more longstanding
Some lesions show mixed patterns
Myofibroblastic differentiation results in expression of “smooth muscle” immunohistochemical markers
Lesions can thus be mistaken for leiomyosarcoma when mitotically active
Intravascular fasciitis
Similar features to nodular fasciitis, except has intravascular component
Often associated extravascular component encountered
Abundant osteoclast-like giant cells
Prominent mitotic activity can result in an incorrect diagnosis of intravascular leiomyosarcoma
Cranial fasciitis
Lesion of infancy sometimes attributed to birth trauma
Similar morphology to that of nodular fasciitis, but more myxoid
Some reported lesions are probably instead fibromatoses
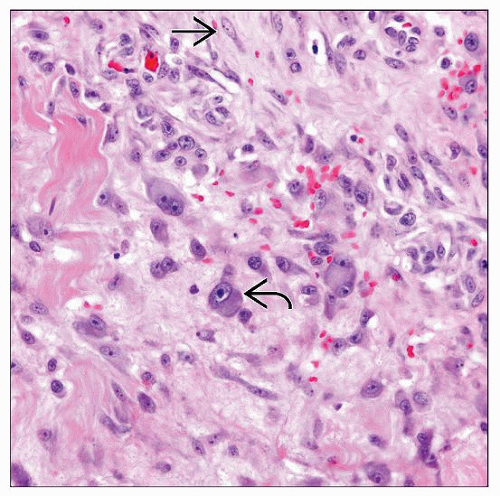
Proliferative fasciitis
Predominantly plump stellate to spindled fibroblasts and myofibroblasts
Extravasated erythrocytes
Background myofibroblasts
Large ganglion-like fibroblasts
Macronucleoli, abundant amphophilic cytoplasm
Not true ganglion cells; no Nissl substance
Pediatric examples
Ganglion-like cells predominate
Exuberant mitotic activity
Mistaken for rhabdomyosarcomas in the past
Lack skeletal muscle markers (MYOD1, myogenin)
Ischemic fasciitis
Ill-defined focally myxoid masses
Lobular configuration
Most centered in deep subcutis
A few extend into skeletal muscle or tendon/aponeurosis
Overlying skin typically intact
Zones of fibrinoid necrosis and myxoid stroma
Necrotic zones rimmed by ingrowing ectatic thin-walled vessels
Atypical enlarged degenerating fibroblasts with abundant basophilic cytoplasm, large hyperchromatic nuclei, prominent nucleoli
Occasional mitoses, including atypical forms
DIFFERENTIAL DIAGNOSIS
Fibrous Histiocytoma (Dermatofibroma)
Mostly in differential diagnosis of nodular fasciitis
Typically small superficial lesions
Storiform pattern
Collagen trapping
Abundant background changes (foamy histiocytes, hemosiderin, plasma cells)
Overlying dermal hyperplasia
Factor VIII reactive; variable actin expression
Tend to recur locally when incompletely excised
Neurofibroma
Small superficial lesions
Serpentine nuclei
Shredded-appearing collagen, nuclei “plastered” against collagen fibrils
Myxoid change, mast cells
S100 protein(+), variable CD34(+)
Benign behavior
Fibromatosis
Large, deep, infiltrative lesions
Shoulder girdle, abdomen (in women in childbearing years), head and neck
Sweeping fascicles of myofibroblasts
Uniform collagen deposition
Prominent vascular pattern
Highly infiltrative
Express actin (myofibroblastic), show nuclear β-catenin labeling
Prone to local recurrences
Kaposi Sarcoma
Immunocompromised patients and elderly patients
In setting of AIDS/HIV, often in skin and mucosal surfaces of upper half of body
In elderly, in distal lower extremity
All examples associated with HHV8
Hyperchromatic spindle cells
Extravasated erythrocytes, hemosiderin, plasma cells, hyaline globules
Immunoreactivity: CD34, CD31, HHV8
Most behave indolently
Quasineoplastic: Can regress if immunosuppression is reduced
Malignant Fibrous Histiocytoma (Undifferentiated Pleomorphic Sarcoma)
Deep lesions in 6th, 7th decade
Storiform pattern
Pleomorphic nuclei
Outcome related to stage; overall 5-year survival about 60%
Embryonal Rhabdomyosarcoma
Mostly in differential diagnosis of proliferative fasciitis in children
Genital region/head and neck of young children
Enhanced cellularity beneath mucous membranes (cambium layer)
Atypical nuclei often without prominent nucleoli
Expresses skeletal muscle markers on immunolabeling
Responds to chemotherapy (70-80% 5-year survival)
Well-Differentiated Liposarcoma
Mostly in differential diagnosis for ischemic fasciitis
Large, deep lesions of proximal extremities and retroperitoneum
Mature-appearing adipose tissue lesion with relatively homogeneous low-power appearance
Lobules of fat separated by fibrous bands containing enlarged hyperchromatic nuclei
Occasional lipoblasts (not required for diagnosis)
Minimal mitotic activity
Low-grade sarcoma
Leiomyosarcoma
Wide range of clinical presentations
Perpendicularly oriented fascicles
Brightly eosinophilic cytoplasm
Hyperchromatic nuclei with blunt ends
Paranuclear vacuoles
Immunolabeling: Actin, desmin, calponin, and caldesmon all reactive
Outcome relates to stage and site
Pleomorphic Rhabdomyosarcoma
In differential diagnosis of proliferative fasciitis in adults
Highly aggressive tumors of deep proximal extremities of older adults
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree