Prostate Carcinoma, General Concepts
Gladell P. Paner, MD
Rafael E. Jimenez, MD
Jesse K. McKenney, MD
TERMINOLOGY
Synonyms
Prostate carcinoma (PCa)
Definitions
Term “prostate cancer/carcinoma” has been used for varying histologic subtypes
Acinar adenocarcinoma and morphologic variants
Ductal adenocarcinoma
Adenosquamous and squamous cell carcinoma
Basaloid and adenoid cystic carcinoma
Small cell carcinoma
Sarcomatoid (spindle cell) carcinoma
However, ≥ 95% of PCas are acinar adenocarcinoma
Some authors use the term microacinar, acinar, or conventional to describe typical PCa
Epidemiologic, pathogenetic, and clinical features of PCas mainly based on those of acinar adenocarcinoma
EPIDEMIOLOGY
Age Range
Common in elderly men; low incidence in < 50 years
Incidence increases dramatically with age; > 75% occur in patients ≥ 65 years
Mortality from prostate cancer also increases with age
3rd and 2nd cause of cancer death in ages 60-79 years and ages 80 years or older, respectively
Not one of top 5 causes of cancer mortality for ages 40-59 years
Incidence
6th most common cancer in the world
Incidence varies in different parts of the world
Attributed to ethnic and environmental factors and detection rates of clinically latent tumors
High incidence areas include USA, Australia, and Scandinavian countries
In USA, prostate cancer is most common malignancy in men; 2nd most lethal after lung cancer
In 2009: 192,280 new cases of prostate cancer were expected in USA, and 27,360 men expected to die from disease
Low incidence areas include Asia and North Africa
Mortality rates
High in North America, North and West Europe, Australia, and Caribbean
Low in Asia and North Africa
Differences in mortality rates less marked than differences in incidence rates in different areas
Ethnicity Relationship
In USA, African-Americans have highest incidence and mortality rates, up to 70% higher than Caucasians
Lower rates in Asian-Americans than Caucasians
Rate differences in ethnic groups also documented in other regions of the world, such as Brazil and Europe
Diet
Strong positive association with diets rich in animal products, particularly red meat
Suggested to be due to heterocyclic amine content
Weak association with obesity
Healthy weight and diet low in total fat associated with lower risk for prostate cancer
Fruits and vegetables may have protective effect
ETIOLOGY/PATHOGENESIS
General Concepts
Migration studies demonstrate that immigrants from low incidence areas acquire intermediate-risk levels after migrating to high-risk areas
Suggests role for environmental and genetic factors
Well-documented familial association
5-11x increased risk among men with 2 or more 1st-degree relatives with prostate cancer
Proposed higher risk with environmental exposures
Cadmium, rubber, textile, chemical, drug, fertilizer, and atomic energy industries
Vitamin D deficiency implicated and may explain geographic differences due to light exposure
Controversial association with xenotropic murine leukemia virus-related virus (XMRV)
CLINICAL IMPLICATIONS
Clinical Presentation
Majority of PCa in USA are clinically diagnosed in asymptomatic patients
Tumor detected due to early detection programs
Main indications for prostate biopsy
Increased serum PSA level
Abnormal digital rectal examination (DRE)
Palpable nodules, firmness, or asymmetry
Majority of prostate cancer (70-75%) arise in posterior zone, which is accessible by palpation
Low sensitivity and positive predictive value
Still considered “gold standard” in clinical staging of prostate cancer
When symptomatic, prostate cancer presents with signs or symptoms of advanced disease
Obstructive bladder symptoms
Transition zone cancers may present earlier
Pelvic pain due to local extension
Bone pain and tenderness, spinal cord compression, or adenopathy due to metastatic disease
Rarely, disseminated intravascular coagulation, nonbacterial thrombotic endocarditis, ascites, or pleural effusion
Paraneoplastic syndrome more common in certain carcinoma subtypes (i.e., small cell carcinoma)
˜ 10% of transurethral resection of prostate (TURP) specimens for lower urinary tract obstruction contain incidental prostate cancer
Laboratory Tests
Prostate specific antigen (PSA)
Synthesized by secretory cells of normal, hyperplastic, or malignant prostatic acini and ducts
Increased diffusion into serum when basement membrane is breached by invasive PCa
Traditional cut off is 4 ng/mL, over which prostate biopsies are recommended
PSA serum level above 4 ng/mL has sensitivity of ~ 20% and specificity of 60-70% for PCa
Sensitivity in cancer detection increases with lower serum PSA cut-off
Modifications of measurement and interpretation used to improve sensitivity and specificity
PSA density
Serum PSA level/prostate gland volume
> 0.15 would prompt prostate biopsy
Age-specific ranges
Higher PSA levels permissible in older age groups (e.g., 2.5 ng/mL for men 40-49 years vs. 6.5 ng/mL for men 70-79 years)
PSA velocity
Relative change in time of PSA value
Increase of > 0.75 ng/mL per year would prompt prostate biopsy
Percentage of free PSA
PSA not bound to serum protease inhibitors
Low levels (< 10%) associated with higher risk of cancer
PSA levels useful in monitoring patients after therapy for prostate cancer
National Comprehensive Cancer Network (NCCN) 2009 guidelines
Perform biopsy for abnormal DRE regardless of serum PSA level
Consider biopsy for PSA 2.6-4 ng/mL or PSA velocity > 0.35 ng/mL/y when PSA ≤ 2.5 ng/mL
Also consider age, comorbidity, percent free PSA, prostate exam/size, family history, African-American race
Prefer biopsy when PSA 4-10 ng/mL or do free PSA when risk of biopsy &/or diagnosis and treatment outweighed by comorbid conditions
Perform biopsy if free PSA ≤ 10%
Perform biopsy when PSA >10 ng/mL
American Urological Association (AUA) 2009 Best Practice Policy
Baseline serum PSA level at 40 years old
No single threshold value for PSA to prompt prostate biopsy is recommended
Decision based primarily on PSA and DRE, but other factors should be considered
Consider multiple factors: Free and total PSA, age, PSA velocity, PSA density, family history, ethnicity, prior biopsy history, and comorbidities
Prostatic acid phosphatase (PAP)
1st serum marker used for prostate cancer
Low sensitivity and specificity limit its role in prostate cancer diagnosis and monitoring
Also elevated in prostatic hyperplasia and inflammation
Prostate specific membrane antigen (PSMA)
Most informative in hormone-resistant states, metastasis, or in tumor recurrence or progression
Molecular diagnostic tests
Currently investigational
Clinical utility in prostate cancer diagnosis and management still to be confirmed
May target PCa-associated proteins, mRNA, or DNA
High throughput gene expression profiling and proteinomics have identified genes and proteins specifically overexpressed in prostate cancer
Candidate biomarkers include
Human kallikrein 2, urokinase-type plasminogen activator receptor, PSMA, early prostate cancer antigen, prostate carcinoma antigen 3, AMACR, GST-κ, TMPRSS2-ERG gene fusions
Performed in tissues, blood, or urine samples
Use varying methods of detection, such as RT-PCR, ELISA, Western blot, or other techniques
RT-PCR extremely sensitive assay, capable of detecting 1 prostate cell in 108 nonprostate cells
Limits clinical utility of this assay due to possible nonspecific positivity
Natural History
PCa is biologically heterogeneous and some present clinically as “latent” or “quiescent” tumors
Latent form PCa extremely common; up to 80% of PCa in 9th decade
Unclear whether latent tumors are intrinsically different from clinically significant tumors
Natural history of nonlatent PCa highly dependent on stage at presentation
Imaging Findings
Radiographic studies
As ancillary tool in diagnosis of primary tumors
More useful for staging and detection of metastases
Bone scan performed for localized disease with PSA > 20 ng/mL, Gleason score (GS) ≥ 8, or symptomatic T3 or T4 disease
Osteoblastic bone metastasis for acinar carcinoma
Pelvic CT or MR performed for T3 or T4 disease or in localized cancer with high nomogram probability for lymph node involvement
In PSA era of lower stage prostate cancers, false-positivity higher in detecting metastases
Staging imaging studies not routinely recommended if GS < 7 or PSA < 20 ng/mL
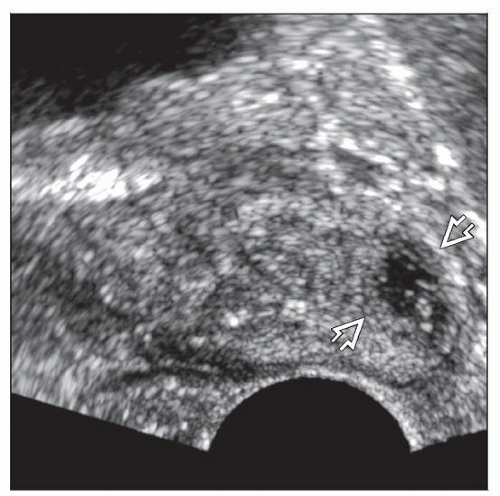
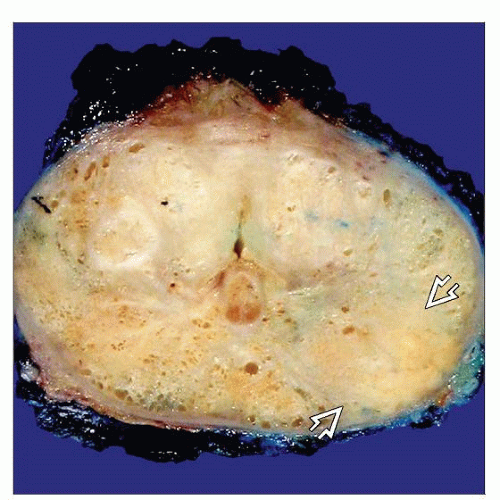
Ultrasonography
Transrectal ultrasound (TRUS) mainly to guide needle core biopsy sampling
Also to measure prostate gland volume and to estimate prostate cancer size
Low sensitivity and specificity
Most prostate cancers are hypoechoic lesions (40%) but can be hyper- (30%) or isoechoic (30%)
Organ-confined prostate cancer isoechoic with prostate parenchyma are difficult to detect
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree