Progressive Transformation of Germinal Centers
Pei Lin, MD
Key Facts
Terminology
Progressive transformation of germinal centers (PTGC)
Clinical Issues
Young adults most commonly affected
Asymptomatic localized lymphadenopathy in most patients
Cervical lymph nodes in ˜ 50%
Generalized lymphadenopathy occurs in subset of patients
Can be incidental finding in patients with lymphoma
NLPHL most common
PTGC usually resolves spontaneously
Can recur
PTGC not associated with HIV
Microscopic Pathology
Scattered large follicles in otherwise reactive lymph node with follicular hyperplasia
Mantle zone cells migrate into and disrupt hyperplastic germinal centers
Each affected follicle at different stage of PTGC (asynchronous)
Top Differential Diagnoses
Nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL)
Lymphocyte-rich classical Hodgkin lymphoma, nodular variant
Follicular lymphoma, floral variant
HIV-associated lymphadenopathy
TERMINOLOGY
Abbreviations
Progressive transformation of germinal centers (PTGC)
Synonyms
Progressively transformed germinal centers
Progressively transformed follicular centers
Definitions
Reactive hyperplasia of follicles characterized by
Large follicles with hyperplastic germinal centers
Disruption of germinal centers due to infiltration by mantle zone B cells
Affected follicles typically are at different stages of dissolution
ETIOLOGY/PATHOGENESIS
Unknown
Viral cause suspected
CLINICAL ISSUES
Presentation
PTGC can occur at any age but is common in young adults
Median age: 28 years
˜ 20% of cases occur in children
Men are more often affected than women
PTGC usually involves peripheral lymph nodes
Cervical lymph nodes are most commonly involved (50% of cases)
Axillary and inguinal lymph nodes less common
PTGC can be the predominant change in lymph nodes prompting biopsy
Patients with PTGC can present with or without symptoms
Most frequent presentation is asymptomatic and localized lymphadenopathy
Generalized lymphadenopathy can occur in subset of patients
Adolescents who present with viral-like illness
Patients with autoimmune diseases
PTGC can be incidental finding in patients with lymphoma
PTGC can be detected at initial diagnosis or after therapy
Interval between PTGC and lymphoma can be > 10 years
PTGC also rarely can precede diagnosis of lymphoma
PTGC usually spontaneously resolves but can recur
Same or different lymph nodes
Recurrence occurs more often in children than adults
PTGC is not associated with human immunodeficiency virus infection
Treatment
Observation
Prognosis
Excellent
IMAGE FINDINGS
Radiographic Findings
Lymphadenopathy in subset of patients
MICROSCOPIC PATHOLOGY
Histologic Features
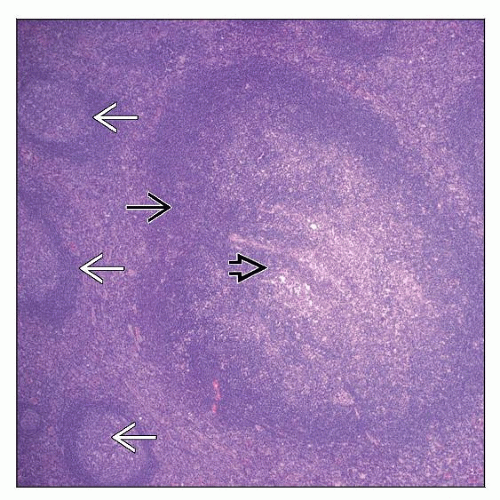
Follicles with PTGC are usually large
4-5x the size of normal reactive secondary follicles
PTGC is usually focal; involves only a few follicles in lymph node
Process of PTGC appears to proceed in stages
Initially germinal centers become hyperplastic
“Starry sky” pattern can occur but unusual
2-3 germinal centers per follicle fuse together
Mantle zone B cells infiltrate and disrupt germinal centers
Eventually germinal centers disappear
Centroblasts and follicular dendritic cells are scattered among small mantle zone B cells
Follicles involved by PTGC appear to be at different stages (i.e., asynchronous)
PTGC is almost always accompanied by follicular hyperplasia
Interfollicular hyperplasia often present
PTGC follicles can show Castleman-like changes; uncommon
Clusters of epithelioid cells can surround PTGC follicles
More common in pediatric cases
PTGC can coexist with Hodgkin or non-Hodgkin lymphoma
Nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) most common
No data to support PTGC as precursor of NLPHL
Other lymphoma types uncommonly associated with PTGC
Classical Hodgkin lymphoma (nodular sclerosis or mixed cellularity)
Plasma cell myeloma
PTGC may involve same lymph node involved by lymphoma or different lymph node
In generalized cases of PTGC, histologic findings are more florid
Rarely associated with lymphoma
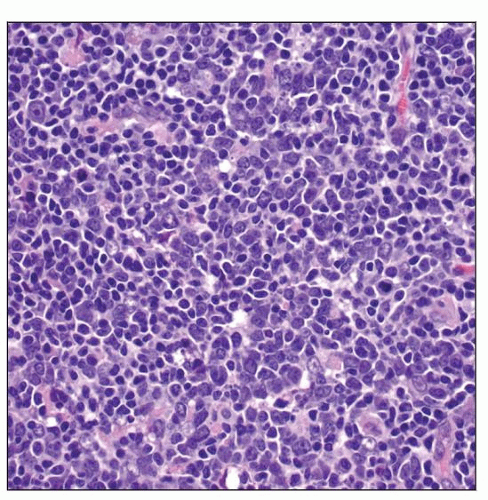
Cytologic Features
Mixed population of small and large lymphocytes
Small round lymphocytes are mantle zone B cells and reactive T cells
Germinal center centrocytes and centroblasts
No LP cells; no Hodgkin or Reed-Sternberg (HRS) cells
No plasma cells, neutrophils, or eosinophils
ANCILLARY TESTS
Immunohistochemistry
Preserved B-cell and T-cell compartments of lymph node
Prominent follicular pattern
In PTGC follicles
Germinal centers
B-cell antigens(+), T-cell antigens(-)
CD10(+), Bcl-6(+), Bcl-2(-)
Disruption of follicular dendritic cells that are CD21(+), CD23(+)
Mantle zones
B-cell antigens(+), T-cell antigens(-)
IgD(+), Bcl-2(+)
CD10(-), Bcl-6(-)
T cells are relatively few in PTGC follicles
Flow Cytometry
No evidence of monoclonal B-cell population
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree