Chapter 8 Principles of Toxicology
| Abbreviations | |
|---|---|
| ATP | Adenosine triphosphate |
| CNS | Central nervous system |
| CO | Carbon monoxide |
| DNA | Deoxyribonucleic acid |
| EDTA | Ethylenediamine tetraacetic acid |
| GI | Gastrointestinal |
Therapeutic Overview
Mechanisms of Action
Many toxic substances are known primarily to affect a specific target organ, such as the liver, nervous system, lungs, or kidneys, whereas others target the immune system or may affect normal fetal and cell growth and development. It is important to note, however, that although certain anatomical or functional characteristics may predispose organs to injury, designation of toxicants as “organ specific” (e.g., neurotoxic, cardiotoxic) is somewhat misleading, for several reasons. First, toxic substances may have adverse effects throughout the body, and although a chemical may primarily affect one organ, other organs may also incur less notable injury. Second, a toxic response in one tissue will undoubtedly have serious consequences for other tissues depending on the characteristics of the chemical (physical state, site of exposure, dose, and duration of exposure) and of the patient (general health, nutritional state, age, sex, enzyme induction, immune response, antioxidant concentrations). Thus a minor insult to a compromised organ may cause unexpected injury to that organ and may also affect other organs.
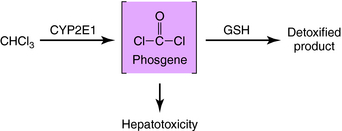
Because of a dual blood supply from the hepatic artery and the portal vein, the liver may be exposed to toxicants entering from the systemic circulation (e.g., via inhalation) or from the splanchnic circulation (absorbed from the gastrointestinal [GI] tract). The leaky capillary system of the hepatic sinusoids promotes the extraction of toxicants from the blood into the liver. The liver contains enzymes that metabolize many endogenous and exogenous chemicals (see Chapter 2). In some cases chemical modification produced by biotransformation results in bioactivation (production of toxic-reactive metabolites). This is exemplified by the bioactivation of chloroform to phosgene (Fig. 8-1). Compounds that enhance the activity of CYP2E1 (enzyme-inducing agents) or reduce the hepatic concentration of glutathione can exacerbate chloroform-induced liver injury. Other compounds that can cause liver injury after metabolism include several solvents (carbon tetrachloride, halogenated benzenes) and carcinogens (aflatoxin B, aromatic amines).
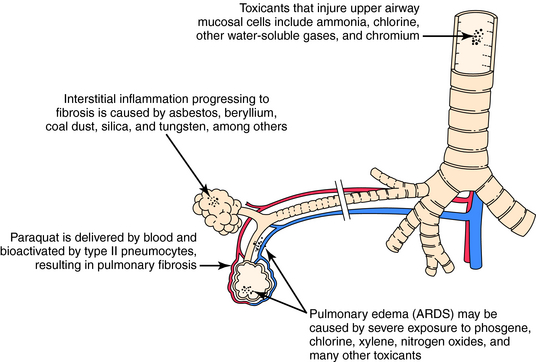
The blood can serve as the route of exposure of the lung in the case of paraquat, a herbicide taken up by type II pneumocytes. Biotransformation in the lung yields a reactive intermediate that undergoes redox cycling, which produces reactive oxygen species that injure the cell. Although exposure to paraquat usually occurs after ingestion or skin contamination, death results from pulmonary injury. Similarly, certain pyrrolidine alkaloids are metabolized in the liver to compounds that circulate in the blood and produce toxicity in the lung. The actions of toxicants on pulmonary tissue are shown in Figure 8-2.
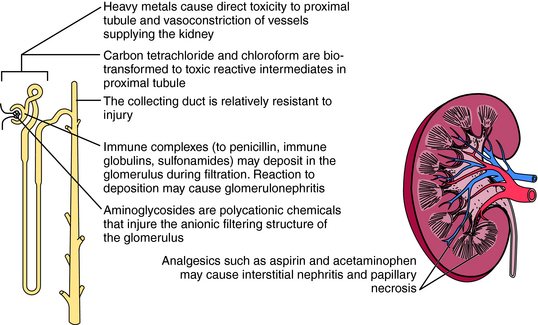
The kidney is also susceptible to toxicants. The mechanisms of renal injury are similar to those in other organs but also include unique mechanisms. Delivery of blood-borne toxicants to the kidney is high, because the kidney receives 25% of cardiac output, and its functions include filtering, concentrating, and eliminating toxicants. As water is reabsorbed, the concentration of chemicals in the tubule can increase to toxic levels. In some cases the concentration may exceed the solubility of a chemical and lead to precipitation and obstruction of the affected area (Fig. 8-3).
The kidney can compensate for excessive chemical exposure because, like many organs, it has a reserve mass. Thus tissue injury equal to one entire kidney must occur before loss of function is clinically apparent. The kidney also replaces lost functional capacity by hypertrophy. In addition, the kidney has developed binding proteins to remove heavy metals. For example, metallothioneins avidly bind cadmium, protecting the kidney and other organs from toxicity. However, renal toxicity will develop if exposure exceeds the binding capacity or if a large amount of the cadmium-metallothionein complex accumulates.
In addition to being a target for chemical-mediated injury, the immune system may mediate injury by producing hypersensitivity reactions—adverse events caused by an immune response to foreign antigens (see Chapter 6). Indeed, cell-mediated hypersensitivity initiated by T lymphocytes may lead to contact dermatitis as a consequence of exposure to nickel and several industrial chemicals.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree