16 Principles and Practice of Secondary Prevention
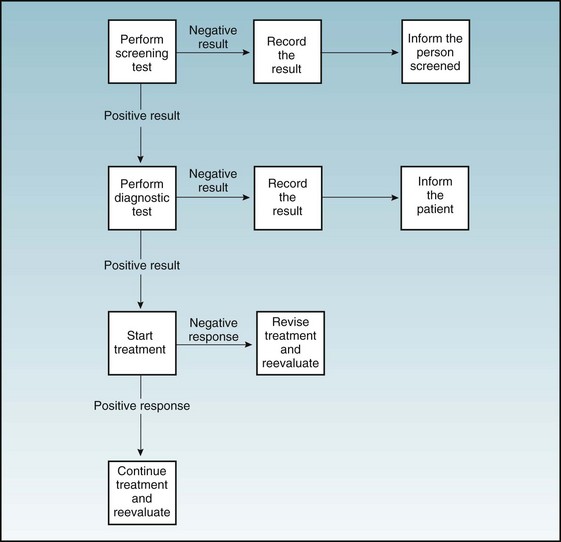
As shown in Figure 16-1, the process of screening is complex and involves a cascade of actions that should follow if each step yields positive results. In this regard, initiating a screening program is similar to boarding a roller coaster; participants must continue until the end of the process is reached. Many members of the public assume that any screening program will automatically be valuable or cost-effective; this explains the popularity of mobile imaging vans that offer full-body computed tomography (CT) and the direct-to-consumer marketing of genomic analysis. In contrast, many preventive medicine specialists demand the same standards of evidence and cost-effectiveness as for therapeutic interventions in patients with known disease. A case may be made for even higher standards. Screening means looking for frouble. It involves, by definition, people with no perception of disease, most of whom are well; therefore great potential exists to do net harm if screening is performed haphazardly.
A program to take annual blood pressure of employees of a business or industry would be considered screening, whereas performing chest radiography for a patient who was just admitted to a hospital for elective surgery would be called “case finding.” The distinction between screening and case finding is frequently ignored in the literature and in practice. Most professional societies do not distinguish between the two in their recommendations regarding screening. We use the two terms interchangeably in this chapter. Chapter 7 discusses some of the quantitative issues involved in assessing the accuracy and performance of screening, including sensitivity, specificity, and predictive value of tests. In this chapter we assume the reader is comfortable with these concepts. The purpose here is to discuss broader public health issues concerning screening and case finding. Chapter 18 provides an extensive discussion of the U.S. Preventive Services Task Force in the clinical encounter.
I Community Screening
A Objectives of Screening
Community screening programs seek to test large numbers of individuals for one or more diseases or risk factors in a community setting (e.g., educational, work, recreational) on a voluntary basis, often with little or no direct financial outlay by the individuals being screened (Table 16-1).
Table 16-1 Objectives of Screening Programs
| Target | Objective | Examples |
|---|---|---|
| Disease | Treatment to reduce mortality | Cancer |
| Treatment to prevent complications | Hypertension | |
| Treatment to eradicate infection and prevent its spread | Gonorrhea, syphilis, tuberculosis | |
| Change in diet and lifestyle | Coronary artery disease, type 2 diabetes mellitus | |
| Risk Factors | ||
| Behavioral | Change in lifestyle | Cigarette smoking, unsafe sexual practices |
| Environmental | Change in occupation | Chronic obstructive pulmonary disease from work in a dusty trade |
| Metabolic | Treatment or change in diet and lifestyle | Elevated serum cholesterol levels |
B Minimum Requirements for Community Screening Programs
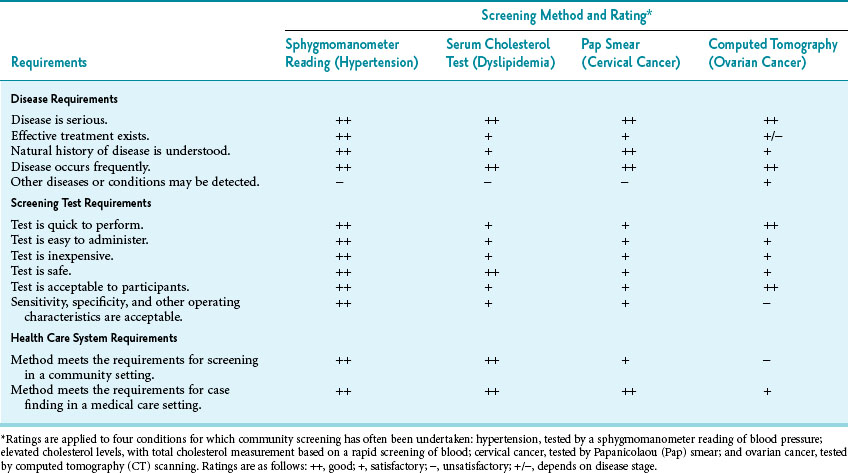
If any of the requirements is not at least partially met, an extensive population-wide screening program may be inappropriate. Table 16-2 outlines these requirements in four common screening programs, for hypertension, high cholesterol, cervical cancer, and ovarian cancer, as further discussed in Application of Minimum Screening Requirements to Specific Programs.
Table 16-2 Requirements for Screening Programs and Ratings of Example Methods to Detect Hypertension, Elevated Cholesterol Levels, Cervical Cancer, and Ovarian Cancer
1 Disease Requirements
1. The disease must be serious (i.e., produce significant morbidity or mortality), or there is no reason to screen in the first place.
2. Even if a disease is serious, there must be an effective therapy for the disease if it is detected. Screening is of no value unless there is a good chance that detecting the disease in the presymptomatic stage would be followed by effective therapy. Furthermore, the benefits of detecting the condition in a few people should outweigh the harms that occur (and accrue) to people with a false-positive test, including unnecessary, invasive workups and treatment. For example, at present, there is no value in screening for pancreatic cancer because the chance of cure by standard medical and surgical methods is extremely small. The controversy around prostate cancer screening is largely about the benefits of treatment versus the possible harm of unnecessary treatment.
3. The natural history of a disease must be understood clearly enough to know that there is a significant window of time during which the disease is detectable, and a cure or at least effective treatment would occur. For example, colon cancer follows an established disease mechanism from small polyps in the colon to colon cancer. Early detection and surgical removal of a polyp in the colon could prevent intestinal obstruction and morbidity, and likely is curative.
4. The disease or condition must not be too rare or too common. Screening for a rare disease usually means that many false-positive test results would be expected for each true finding (see Chapter 7). This increases the cost and difficulties of discovering persons who truly are ill or at high risk, and it causes anxiety and inconvenience for individuals who must undergo more testing because of false-positive results. Unless the benefits from discovering one case are very high, as in treating a newborn who has phenylketonuria or congenital hypothyroidism, it is seldom cost-effective to screen general populations for a rare disease.
2 Screening Test Requirements
1. The screening test must be reasonably quick, easy, and inexpensive, or the costs of large-scale screening in terms of time, effort, and money would be prohibitive.
2. The screening test must be safe and acceptable to the persons being screened and to their clinicians. If the individuals to be screened object to a procedure (as frequently occurs with colonoscopy), they are unlikely to participate.
3. The sensitivity, specificity, positive predictive value, and other operating characteristics of a screening test must be known and acceptable. False-positive and false-negative test results must be considered. An additional difficulty in using screening tests in the general population is that the characteristics of the screening test may be different in the population screened from the population for whom the screening was developed.
3 Health Care System Requirements
1. People with positive test results must have access to follow-up. Because screening only sets apart a high-risk group, persons who have positive results must receive further diagnostic testing to rule in or rule out actual disease. Follow-up testing may be expensive, time-consuming, or painful, with some risk. With many screening programs, most of the efforts and costs are in the follow-up phase, not in the initial screening.
2. Before a screening program for a particular disease is undertaken, treatment already should be available for people known to have that disease. If there are limited resources, it is not ethical or cost-effective to allow persons with symptoms of the disease to go untreated and yet screen for the same disease in apparently well persons.
3. Individuals who are screened and diagnosed as having the disease in question must have access to treatment, or the process is ethically flawed. In addition to being unethical, it makes no medical sense to bring the persons screened to the point of informing them of a positive test result and then abandon them. This is a major problem for community screening efforts because many people who come for screening have little or no medical care coverage. Therefore, the cost for the evaluation of the positive screening tests and the subsequent treatment (if disease is detected) are often borne by a local hospital or other institution.
4. The treatment should be acceptable to the people being screened. Otherwise, individuals who require treatment would not undertake it, and the screening would have accomplished nothing. For example, some men may not want treatment for prostate cancer because of possible incontinence and impotence.
5. The population to be screened should be clearly defined so that the resulting data are epidemiologically useful. Although screening at “health fairs” and in shopping centers provides the opportunity to educate the public about health topics, the data obtained are seldom useful because the population screened is not well defined and tends to be self-selected and highly biased in favor of those concerned about their health.1
6. It should be clear who is responsible for the screening, which cutoff points are to be used for considering a test result “positive,” and how the findings will become part of participants’ medical record at their usual place of care.
4 Application of Minimum Screening Requirements to Specific Programs
Table 16-2 applies the previously described criteria to the following four conditions for which community screening has been undertaken:
 Hypertension, tested by a sphygmomanometer reading of blood pressure
Hypertension, tested by a sphygmomanometer reading of blood pressure
 Elevated cholesterol levels, based on a screening of blood
Elevated cholesterol levels, based on a screening of blood
 Cervical cancer, with Papanicolaou smear
Cervical cancer, with Papanicolaou smear
 Ovarian cancer, for which CT scan screening was considered but rejected
Ovarian cancer, for which CT scan screening was considered but rejected
As shown in Table 16-2, screening for hypertension, hypercholesterolemia, and cervical cancer generally fulfill the minimum requirements for a community screening program. Investigators have agreed that a screening program using CT scans to detect ovarian cancer in the general population fails at two critical points. First, the yield of detection is low. Second, as numerous studies have shown, only a small proportion of cancers can be cured by the time they are detected.2 Because of these problems, community screening for ovarian cancer is not recommended.
For many screening programs, debate surrounds general screening issues such as what age to start the screening, when to stop, how often to repeat the screening, and whether the methods yield accurate results. Screening for breast cancer is an example of a controversial screening program because the benefits seem to be less than originally hoped and risks are associated with screening mammography.3 The age at which to begin screening women for breast cancer is particularly controversial because breast cancer is less common in younger women, but often more aggressive than later in life, and the risks of screening (e.g., false positives) are higher (Box 16-1).
Box 16-1 Screening Controversies
“Are you really saving lives? And how much worry and lost quality of life is one life saved worth?”
Breast cancer and prostate cancer in particular illustrate the challenge in weighing evidence of small changes in mortality against side effects of screening and treatment. Because of the impact of screening biases, only a change in overall mortality in the screened population is considered evidence of an effective screening program. The debate about changes in the U.S. Preventive Services Task Force (USPSTF) recommendations on breast cancer also demonstrate that few issues in preventive medicine have more power to polarize the public, politicians, and health care professionals than screening.30
Breast Cancer
As of 2011, the strongest evidence shows that any difference in overall mortality between populations exposed to screenings and those not screened is small: for every 2000 women invited for screening throughout 10 years, one will have her life prolonged; 10 healthy women who would not have been diagnosed if there had not been screening will be treated unnecessarily, and more than 200 women will experience important psychological distress for many months because of false-positive findings.30
In 2009, USPSTF changed its screening recommendations regarding breast cancer for women age 40 to 49. Previously recommending routine screening in this population, the Task Force now argued that the improvement in mortality in women between age 40 and 49 was small and that possible harms needed to be considered. Instead, USPSTF recommended that physicians discuss the risks and benefits of screening with the women and to proceed according to their risk/benefit preferences. This change led to a significant media backlash. Many people claimed the decision amounted to “care rationing,” and that the USPSTF had overstepped its mandate by weighing mortality benefits against anxiety.31 The Task Force argued that the evidence did not support a “one size fits all” recommendation and that their guidelines empowered patients and their physicians to make rational decisions based on evidence and more respectful of individual values.32 As of 2012, the rating is a “B” for women age 50 to 74 (recommended) and a “C” for women 40 to 49, indicating that USPSTF believes the decision to screen should be individualized, and the net benefit is likely small.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree