a POCT, point-of-care testing.
Smaller sample volume allows POCT use in neonatal and pediatric population and is preferred for those undersized patients requiring frequent testing. The overall cost of patient care is arguably smaller due to improved patient workflows. Testing near the patient requires fewer steps than transporting a specimen to the laboratory, processing, aliquoting, testing, and communicating results back to clinical staff, all of which may reduce preanalytical and postanalytical laboratory-related errors. Portability of POCT allows for increased access to testing in a wider variety of sites, for example, rural areas, accident sites, areas with limited infrastructure and personnel, and locations with underserved populations. One example of the latter is the use of a portable POCT to test for tuberculosis in the risk populations in low-income countries.6
Although POCT offers many advantages, there are some negative aspects of POCT (Table 10.1). On a cost per test basis, POCT is more expensive than the cost of central laboratory testing as a result of the higher disposable and reagent costs of the POCT analyzers. End users may be able to counterbalance these increased costs by gaining efficiencies in improved patient workflows and increased patient satisfaction. Additionally, quality of results is a concern because POCT is usually performed by nonlaboratory personnel who may include nurses, physicians, emergency medical technicians, pharmacists, medics, patients, and medical office assistants. End users with multiple responsibilities and limited laboratory training may not appreciate the value of laboratory quality control (QC) in ensuring quality test results.
LABORATORY REGULATIONS
Accreditation
In the United States, laboratory testing for patient care (with limited exceptions) requires a Clinical Laboratory Improvement Amendments (CLIA) certificate. CLIA was enacted by Congress and established quality standards for all laboratory testing, thereby ensuring the accuracy, reliability, and timeliness of patient test results regardless of where the test was performed.7 The requirements are based on the complexity of the test and not the type of laboratory where the testing is performed (POC or central laboratory). All laboratories performing POCT must be certified under one of the five types of CLIA certificates listed in Table 10.2. The CLIA certificate must be appropriate for the testing that is performed in the laboratory (i.e., appropriate complexity). In addition to the federal program, state departments of public health or public organizations may apply for “deemed” status, which allows these organizations to perform laboratory accreditation and inspections.
TABLE 10.2 Types of CLIA Certificatesa
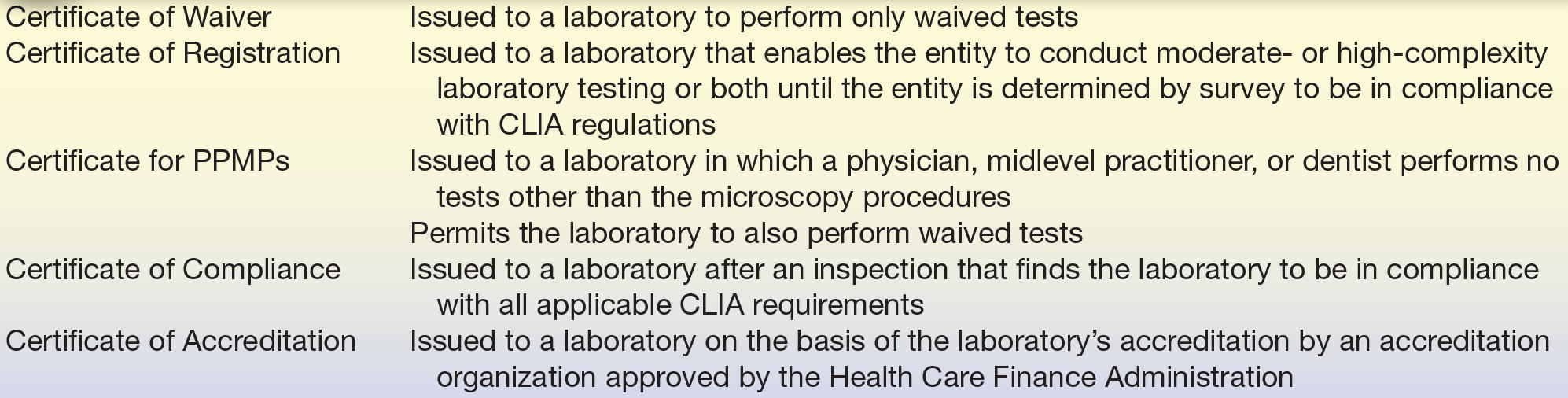
CLIA, Clinical Laboratory Improvement Amendments; POCT, point-of-care testing; PPMP, provider-performed microscopy procedure.
a Clinical Laboratory Improvement Act. How to Obtain a CLIA Certificate of Waiver, http://www.cms.gov/Regulations-and-Guidance/Legislation/CLIA/downloads//howobtaincertificateofwaiver.pdf
POCT Complexity
Tests are classified based on their complexity. The Food and Drug Administration (FDA) uses several criteria to assign complexity to any test, and the three categories are “waived” tests, moderate-complexity tests, and high-complexity tests. Waived tests are a category of tests defined by CLIA, such as dipstick tests, urine pregnancy tests, and blood glucose monitoring devices, which are subject to the lowest level of regulation and are cleared by the FDA for home uses. They employ methodologies that are so simple and accurate as to render the likelihood of erroneous results negligible and pose almost no risk of harm to the patient if the test is performed incorrectly. A full list of currently waived tests can be found on the FDA website (http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfClia/testswaived.cfm). Laboratories performing nonwaived tests (moderate-complexity tests and high-complexity tests) must fulfill all the requirements for personnel qualifications, proficiency testing and inspections, quality assurance and QCs, and patient test management.
The fourth category of POCT is provider-performed microscopy procedures, or PPMPs, which is a subcategory of moderate-complexity testing. These tests involve the use of a microscope, limited to bright-field or phase-contrast microscopy. Generally, the specimens are labile and cannot survive transport to a clinical laboratory. Only licensed physicians, dentists, and midlevel practitioners may perform PPMP. There are usually no QC materials available for PPMP; however, the individual performing PPMP endures the certification process and participates in proficiency testing.
To determine to which category POC test or procedure belongs, refer to the following searchable and continuously renewable FDA-approved test menu: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfClia/search.cfm.
IMPLEMENTATION
Establishing Need
When establishing a POCT site, the approach and steps in the implementation will be different in nearly every case insofar as organizational culture, and the financial situation of any given institution may vary greatly. However, there are some common guidelines to implementation that apply to nearly every case. Support of the organization must be present to evaluate the requests for POCT. Typically, a multidisciplinary committee consisting of laboratory staff, physicians, nursing representatives, and hospital/laboratory administration is formed to create a structure for receiving and establishing criteria for approving requests for POCT. Before implementing a POCT service, an interdisciplinary committee should address the questions similar to those listed in Box 10.1. The decision to establish POCT program is made after justifying the clinical need, cost comparisons, and the analytic performance requirements. Other factors should also be considered, including space, any previous track record of regulatory compliance, personnel who will be performing the testing, and metrics to determine if the POCT implementation is successful.
 BOX 10.1 Questions to Ask When Implementing POCT
BOX 10.1 Questions to Ask When Implementing POCT
- Which test is required and in which specific area? How is the service currently provided, and is this a means to resolve a problem?
- What is the expected annual test volume?
- What clinical question is being asked when requesting this test?
- What clinical decision is likely to be made and action to be taken upon receipt of the result?
- How will POCT increase patient satisfaction?
- Are personnel competent to perform the POCT? Are facilities available to perform the test and store equipment, reagents, and documentation?
- Will a change in practice be required?
- Can central laboratory deliver the required service? How do POCT cost, reference ranges, accuracy, and precision compare to similar tests in a laboratory?
- Are available POCT analyzers user friendly? Can POCT analyzers interface with an LIS and a patient electronic medical record?
- Are both internal and external QC materials available?
- Does the company providing POCT analyzers and reagents offer a reliable support service?
POCT Implementation Protocol
After making the decision to implement POCT, the responsible party selects the method of choice and begins validation. Desirable characteristics of POCT analyzers include ease of use, method accuracy and comparability to the main laboratory method, portability, durability, low maintenance, simple QC, QC lockout features, simple sample handling requirements, bar code patient and operator identification capabilities, and the ability to interface with a laboratory information system (LIS). The manufacturer should aid in providing minimum acceptability requirements, instrument manuals, package inserts for reagents and QCs, materials safety data sheet, and training materials. The manufacture also typically assists with instrumentation setup and validation studies. Method validation should confirm the manufacturer’s specifications, and a procedure/policy should be written for each test. This should not be simply a collection of materials obtained from a manufacturer; rather, these documents should aid in the development of an easy-to-follow, simple, and concise procedure. The procedure should include information on the principle of the method; personnel qualifications; specimen, reagents, supplies, and equipment requirements; QC and calibrations; patient-testing procedure; reference ranges; reporting limits; and interfering substances if applicable. All required regulatory or certifying standards should be in place prior to initiating patient testing (Box 10.2).
 BOX 10.2 Point-of-Care Checklist
BOX 10.2 Point-of-Care Checklist
1. Quality management
The POC program has a written QM program as well as organizational system setting forth levels of authority, responsibility, and accountability. There is a documented system to address unusual patient results or instrument troubleshooting. There is a written procedure for each POCT.
2. Specimen handling
There is a documented procedure describing methods for patient identification and preparation, as well as for specimen collection, accessioning, and preservation before testing. There is a procedure for entering POCT results into the permanent medical record of a patient. Reference intervals should be established.
3. Reagents
All reagents should be stored and labeled as recommended by the manufacturer.
4. Instruments and equipment
Equipment must be evaluated and scheduled for a regular maintenance, as required by the manufacturer.
5. Personnel
The director of the POCT program is a physician or a doctoral scientist. The testing personnel have adequate, specific training to ensure competence, and this must be documented.
6. Quality Control and Calibration
Calibrations and quality controls are run at regular intervals (at least daily). Acceptable limits are defined for control procedures, and there are documented corrective actions when control results exceed defined acceptability limits. Upper and lower limits of the analytical measurement range (AMR) for each analyte are defined.
7. Safety
There is a program to assure that the safety of patients and health care personnel is not compromised by POCT.
Adapted from the College of American Pathologists Point-of-Care-Testing Checklist 01.04.2012 (http://www.cap.org).
Personnel Requirements
For a POC program with moderate-complexity tests, unlike for those POC programs with Certificate of Waiver or certificate for PPMP, institutions are required to have a certain organizational and administrative structure where staff has established qualifications, competency, and experience. The director of laboratory is usually a Ph.D. scientist, or a physician with at least 1 year of experience directing a laboratory with 20 continuing medical education credits,8 or a person with a bachelor’s degree with 2 years’ laboratory experience plus 2 years of supervising experience. Responsibilities of a director are very broad and include policy making, ensuring compliance with regulatory standards, and administrative duties. Importantly, the director is responsible for the analytic performance of all tests. The director must make technical decisions based on a constant monitoring of ongoing proficiency, accuracy, and precision. Such individuals should be a liaison between the clinicians, hospital administration, and laboratory personnel.
Each laboratory performing moderate-complexity tests must have a technical and a clinical consultant. The technical consultant is responsible for scientific oversight of the POCT, while the clinical consultant is required to provide clinical and medical advice. The director of a POCT program, the technical consultant, and the clinical consultant may be the same person.
Even though the implementation of the POCT program may be done differently depending on an institution, the entity responsible for quality management of the POCT program is always the laboratory. It is useful, therefore, for a laboratory to have a person supervising the POCT program, so a POCT coordinator (POCC) fulfills this role. The POCC monitors day-to-day activities of testing personnel, and it is the responsibility of the POCC to coordinate POC patient testing and facilitate compliance with procedures and policies and regulatory requirements. The POCC develops a training program for testing personnel and ensures documentation of competency training. The POCC also oversees completion of proficiency testing programs, performs on-site review of patient testing, QC, and maintenance logs and reports problems and regulatory noncompliance to appropriate management personnel.
Even though the laboratory is responsible for the POCT policies and procedures, it is the clinical staff that does the actual testing. Fostering a partnership between the operators and laboratory will help solve problems that may arise during the testing process. In this decentralized testing model, the specifics of how training is performed, how competency records are maintained, and how reagents are ordered may be different for each institution. The laboratory should monitor POC areas and ensure consistent feedback is provided regarding compliance with any applicable regulations. However, before any testing is initiated, clarifying individual roles and expectations is key to the success of the program.
QUALITY MANAGEMENT
Accuracy Requirements
Understanding how accurate the results need to be in the context of how the test will be used clinically is important before any patient testing is initiated. Ideally, a POC test will provide equivalent results with those from the central laboratory. If this were the case, depending on a clinical situation, physicians would have an option to choose either test and achieve the same clinical outcome. Unfortunately, despite the ongoing harmonization and standardization efforts, currently, there are still accuracy and imprecision concerns with some POCT. One example is the ongoing accuracy and precision problems with glucose meters. Authors of one study applied simulation modeling to relate performance characteristics of glucose analyzers to error rates in insulin dosage.9 Interestingly, glucose meters that met existing POCT quality specifications allowed a large fraction of administrated insulin doses to differ from the intended doses. In addition, two landmark studies on tight glycemic controls gave completely different outcomes.10,11 While one study showed that tight glycemic controls and the following intensive insulin therapy reduce morbidity and mortality among critically ill patients in the surgical ICU,10 authors of another study found that intensive glucose control increased mortality among adults in the ICU.11 There has been a considerable debate in the laboratory medicine literature that the difference in these two studies’ outcome was due to the test method.12, 13, 14 Due to complaints about glucose meter inaccuracy, the FDA is currently developing new standards for glucose meter accuracy.
QC and Proficiency Testing
The purpose of a quality management program is to ensure quality test results. A thorough validation should verify the analytical performance and any applicable limitations with the assay. Ongoing daily QC will alert the operator to any reagent or instrument issues. Some devices have both internal and external QC, both of which have distinctly different roles. Internal QC, which is also referred to as onboard QC, internal checks, electronic QC, or intelligent QC,15 is performed at specific time intervals or at least daily. Internal QC ensures the electronics of the device are performing as expected or, if a manual test, the integrity of the specific test system. Some instruments automate QC and/or calibration, which is helpful for regulatory compliance. This also ensures the instrument is ready to perform quality testing at all times. Another important feature is to tie QC performance requirements to test availability. If QC has not been performed as required and is unsatisfactory, the instrument does not allow patient testing until corrective action has taken place. This is known as QC lockout.
The entire testing process should be checked periodically according to the manufacturer and regulatory requirements by running an external QC. Here, a control sample is introduced to the test system in the same manner as a patient sample. Another form of external QC is proficiency testing, where blind samples are sent to participating laboratories to perform testing. In the United States, results from one laboratory are compared with the results from the laboratories using the same method (peer group).
Quality management programs also need to ensure that the operators are competent to perform testing. After initial training, ongoing assessment of their performance is required. This is commonly called the recertification process. Careful control of personnel records is an important part of the quality management program and may be managed at the POCT site or directly by the laboratory. Some POCT programs will allow “super users” (supervisors, managers, or POCC) to track training renewal dates and to lockout operators whose training has expired.
The greatest source of error in POCT is the preanalytical error. While the above features are necessary for any POCT program, it is more difficult to identify errors arising from poor specimen, for example, sample contamination, dilution, circulating interference (lipemia, icterus, and hemolysis), and proper specimen source (arterial, venous, and fingerstick). For this reason, careful assessment of an area’s compliance in proper specimen collection and handling is needed prior to implementing testing.
Preventing postanalytic errors in reporting can be achieved more reliably with connectivity. With the aid of bar codes, modern technology has improved patient identification and decreased transcription errors in many health care applications. However, linear bar code identification methods are not fail-safe.16 Hospitals should work with laboratories, pharmacy, radiology, and admissions to standardize scanning and printing specifications across a system. Careful control and tight specifications of bar code scanning and printing equipment will minimize the misidentification threat to patient safety.
Total-system POCT quality assurance is thus the combination of several QC mechanisms:
- A mechanism to perform a thorough systems validation
- Reliable, user-friendly POCT device
- Training of POCT operators
- Competency assessment of all individuals involved in POCT
- QC testing and monitoring
- Proficiency testing
- Connectivity and bar-coding technologies
POC APPLICATIONS
POCT makes up nearly 30% of the total in vitro diagnostics market in the United States.17 A wide variety of POCT devices can be loosely classified into a single-use system, handheld device, benchtop device, or the wearable device (Box 10.3). POCT devices are designed with a consideration for the operators who may have little to no laboratory training. Handheld devices are getting smaller and more ergonomic with every generation. A variety of analytical principles used in a laboratory have also been implemented in POCT devices, including the following:
- Reflectance
- Electrochemistry, electrical impedance
- Light scattering/optical motion
- Immunoturbidimetry
- Lateral flow, flow-through, or solid phase immunoassays
- Spectrophotometry, multiwavelength spectrophotometry
- Fluorescence, time-resolved fluorescence
- Polymerase chain reaction
 BOX 10.3 Types of POCT Analyzers
BOX 10.3 Types of POCT Analyzers
1. Single-use, qualitative, or semiquantitative cartridge/strip tests
- Urine and blood chemistry
- Infectious disease agents, cardiac markers, hCG
2. Single-use quantitative cartridge/strip tests with a reader device
- Glucose
- Blood chemistry
- Coagulation
- Cardiac markers, drugs, C-reactive protein (CRP), allergy, fertility tests
- Chlamydia
- HbA1c, urine albumin
- Blood chemistry
- pH, blood gases, electrolytes, metabolites
3. Multiple-use quantitative cartridge/benchtop devices
- Hemoglobin species, bilirubin
- pH, blood gases, electrolytes, metabolites
- Cardiac markers, drugs, CRP
- Complete blood count
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


