Planning management
 . Learn management algorithms for the most common acute scenarios, chronic diseases and symptoms.
. Learn management algorithms for the most common acute scenarios, chronic diseases and symptoms.
 . Use 10 scenarios with worked answers to reinforce these principles.
. Use 10 scenarios with worked answers to reinforce these principles.
Structure of the Section within the PSA
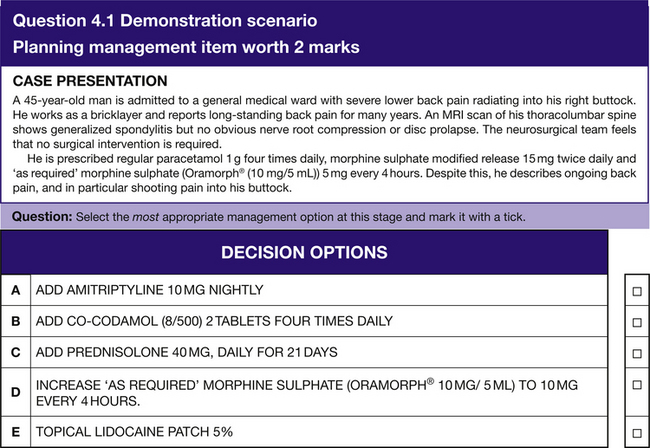
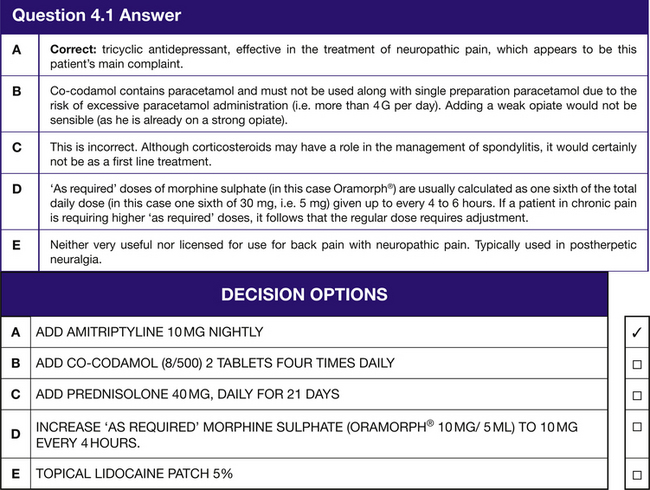
The ‘Planning management’ section will have 8 questions with 2 marks available per question, so a possible total of 16 marks. You will be asked to identify the most appropriate prescription (which may be preventative, curative, symptomatic or palliative) from a list of five for each scenario (see Question 4.1).
Introduction
As with Chapter 2, the practical summaries in each of the three sections incorporate common scenarios in clinical practice and medical examinations, while encompassing those most likely to be seen in the PSA exam.
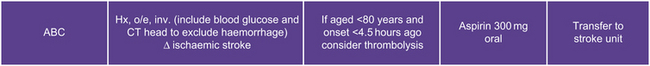
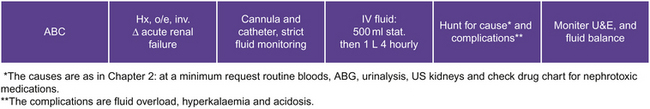
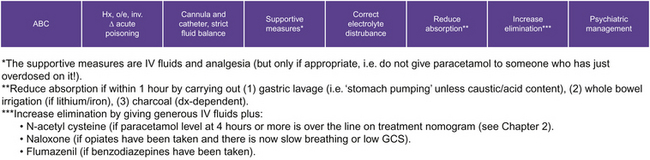
Management of Acute Conditions
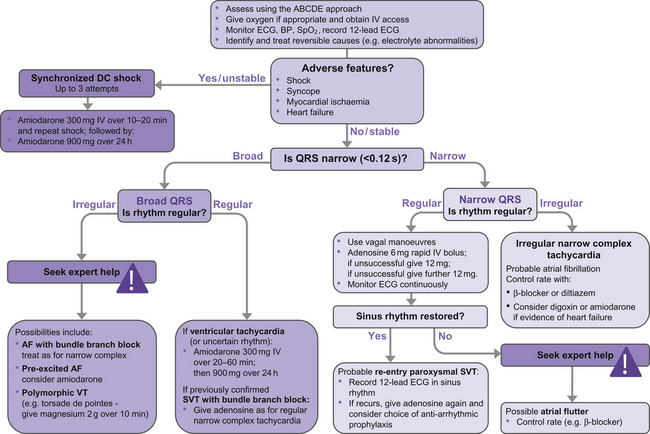
Tachycardia>125 b.p.m.
Remember that many tachycardias>125 b.p.m. will reflect a sick patient with non-cardiac disease (e.g. sinus tachycardia), but always consider the algorithm in Figure 4.2 when not a sinus rhythm.
Respiratory Emergencies
Acute exacerbation of chronic obstructive pulmonary disease (COPD)
Same treatment as asthma (see Fig. 4.4), but add antibiotics if infective exacerbations. Patients are also more likely to have type 2 respiratory failure, so use high-flow oxygen with care. Remember, hypoxia will kill much quicker than hypercapnia. Therefore, in the acute setting, even if a very sick patient has known COPD, apply high-flow oxygen then review it quickly after an arterial blood gas (ABG). This is the same in the PSA: providing the patient is not peri-arrest (in which case high-flow should be applied), 28% oxygen is a safe starter in patients with COPD with ABG 30 min later to assess the effect.
Pneumothorax
 If secondary (i.e. patient has lung disease) then always needs treatment: chest drain if>2 cm or patient SOB or if>50 years old; otherwise aspirate.
If secondary (i.e. patient has lung disease) then always needs treatment: chest drain if>2 cm or patient SOB or if>50 years old; otherwise aspirate.
 If tension pneumothorax (i.e. clinical distinction but often tracheal deviation+/−shock) then emergency aspiration required, but will need chest drain quickly.
If tension pneumothorax (i.e. clinical distinction but often tracheal deviation+/−shock) then emergency aspiration required, but will need chest drain quickly.
 Otherwise (i.e. if primary) determine whether the patient needs treatment:
Otherwise (i.e. if primary) determine whether the patient needs treatment:
Pneumonia
See Figure 4.5 for treatment algorithm. Use mnemonic CURB65 to assess severity of community-acquired pneumonia and hence treatment: Confusion (abbreviated mental test score (AMTS)≤8/10), Urea>7.5 mmol/L, Respiratory rate>30/min, Blood pressure (systolic)<90 mmHg and age≥65 years. For the patient with none or one of these then home treatment is possible; with two or more of these then hospital treatment with oral or IV antibiotics according to policy and severity is required; and with more than three of these then consider ITU admission.
Neurological Emergencies
Bacterial Meningitis
A GP will normally have given the patient 1.2 g benzylpenicillin if there is any suspicion of meningitis (see Fig. 4.8). A computerized tomography (CT) scan of the head is not always required before lumbar puncture (LP); scanning the patient can delay the LP and hence antibiotics.
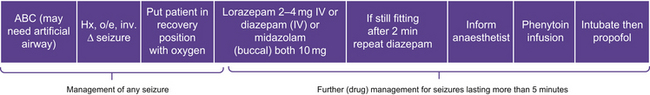
Seizures and status epilepticus
If the patient is having a seizure then (1) ensure the airway is patent, (2) put in recovery position to prevent aspiration if patient vomits and (3) check for provoking factors (e.g. plasma glucose, electrolytes, drugs and sepsis). If the patient is having a seizure for more than 5 minutes, then drugs must be given to stop the seizure as outlined in Figure 4.9. Note that status epilepticus technically means a seizure lasting>30 minutes.
Metabolic Emergencies
Hyperglycaemia (DKA and HONK, Fig. 4.11)
Hyperglycaemic HONK coma
To diagnose hyperglycaemic HONK consider the following:
 Hyperglycaemia (usually>35 mmol/L)
Hyperglycaemia (usually>35 mmol/L)
 HO (hyperosmolar: osmolality over 340 mmol/L (calculated by (x2 Na+x2 K)+urea+glucose)
HO (hyperosmolar: osmolality over 340 mmol/L (calculated by (x2 Na+x2 K)+urea+glucose)
HONK management is the same as DKA management (see Fig. 4.11), except half the rate of fluids is required.
Management of Chronic Conditions
Cardiovascular Conditions
Hypertension
When to treat (see Fig. 4.14)
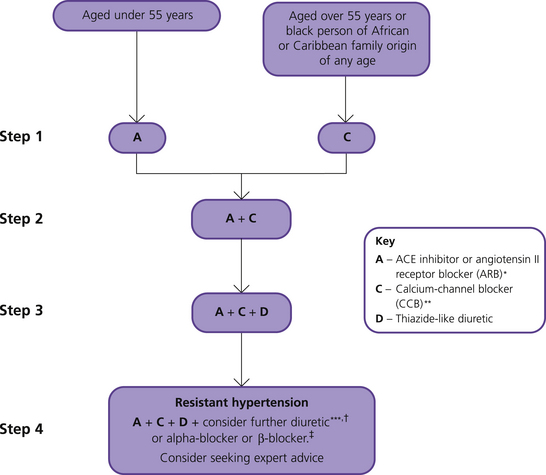
Figure 4.14 Treatment of hypertension (from NICE CG127, 2011, with permission). *Choose a low-cost ARB. **A CCB is preferred but consider a thiazide-like diuretic if a CCB is not tolerated or the person has oedema, evidence of heart failure or a high risk of heart failure. ***Consider a low dose of spironolactone† or higher doses of a thiazide-like diuretic. †At the time of publication (August 2011), spironolactone did not have a UK marketing authorisation for this indication. Informed consent should be obtained and documented. ‡Consider an alpha-blocker or beta-blocker if further diuretic therapy is not tolerated, or is contraindicated or ineffective.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree