Physiology of the Digestive System
OVERVIEW OF DIGESTIVE FUNCTION
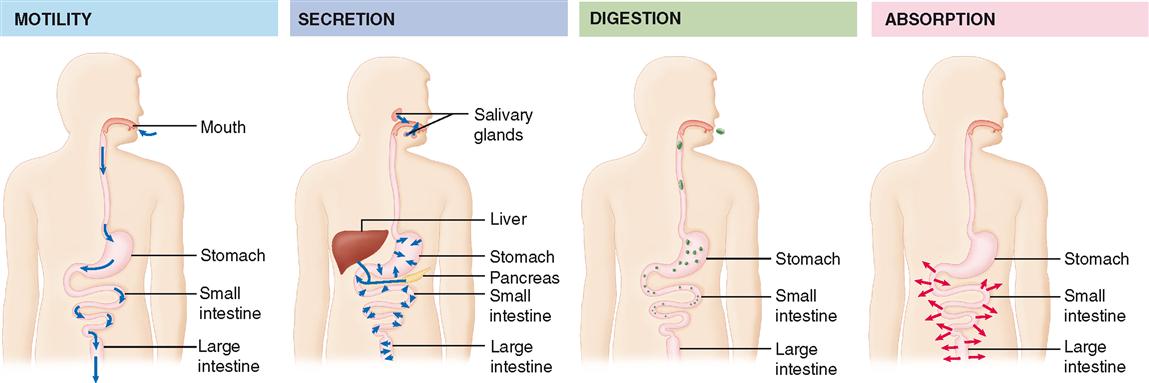
To accomplish the function of making nutrients available to each cell of the body, the digestive system uses various mechanisms (Table 29-1). For example, complex foods must first be taken in—a process called ingestion. Then, complex nutrients are broken down into simpler nutrients in the process that gives this system its name: digestion. To physically break large chunks of food into smaller bits and to move it along the tract, movement (or motility) of the gastrointestinal (GI) wall is required. Chemical digestion—that is, breakdown of large molecules into small molecules—requires secretion of digestive enzymes into the lumen of the GI tract. After being digested, nutrients are ready for the process of absorption, or movement through the GI mucosa into the internal environment. The material that is not absorbed must then be excreted to make room for more material—a process known as elimination. Of course, all these activities must be coordinated, which we have already learned is the process of regulation. Some of the major digestive processes are summarized in Figure 29-1. Digestive regulation is introduced in Box 29-1.
TABLE 29-1
Primary Mechanisms of the Digestive System
| MECHANISM | DESCRIPTION |
| Ingestion | Process of taking food into the mouth, starting it on its journey through the digestive tract |
| Digestion | A group of processes that break complex nutrients into simpler ones, thus facilitating their absorption; mechanical digestion physically breaks large chunks into small bits; chemical digestion breaks molecules apart |
| Motility | Movement by the muscular components of the digestive tube, including processes of mechanical digestion; examples include peristalsis and segmentation |
| Secretion | Release of digestive juices (containing enzymes, acids, bases, mucus, bile, or other products that facilitate digestion); some digestive organs also secrete endocrine hormones that regulate digestion or metabolism of nutrients |
| Absorption | Movement of digested nutrients through the gastrointestinal (GI) mucosa and into the internal environment |
| Elimination | Excretion of the residues of the digestive process (feces) from the rectum, through the anus; defecation |
| Regulation | Coordination of digestive activity (motility, secretion, etc.) |
Note that Figure 29-1 also illustrates that from a functional perspective, the lumen of the alimentary canal is really a tubelike extension of the external environment that goes right through the middle of the body. Thus digested materials are not truly “part of the body” until they’ve been absorbed into the internal environment.
After we have explored the various mechanisms of the digestive process in this chapter, we will be ready for Chapter 30, which discusses the assimilation of nutrients after they have been absorbed.
DIGESTION
After food is ingested (taken into the mouth), the process of digestion begins immediately. Digestion is the overall name for all the processes that chemically and mechanically break complex foods into simpler nutrients that can be easily absorbed. We begin our discussion with a brief overview of mechanical digestion and then move on to a discussion of chemical digestion.
Mechanical Digestion
Mechanical digestion consists of all movement (motility) of the digestive tract that brings about the following:
MASTICATION
Mechanical digestion begins in the mouth when the particle size of ingested food material is reduced by chewing movements, or mastication. The tongue, cheeks, and lips play an important role in keeping food material between the cutting or grinding surfaces of the teeth when a person is biting off or chewing food. In addition to reducing particle size, chewing movements serve to mix food with saliva in preparation for swallowing.
DEGLUTITION
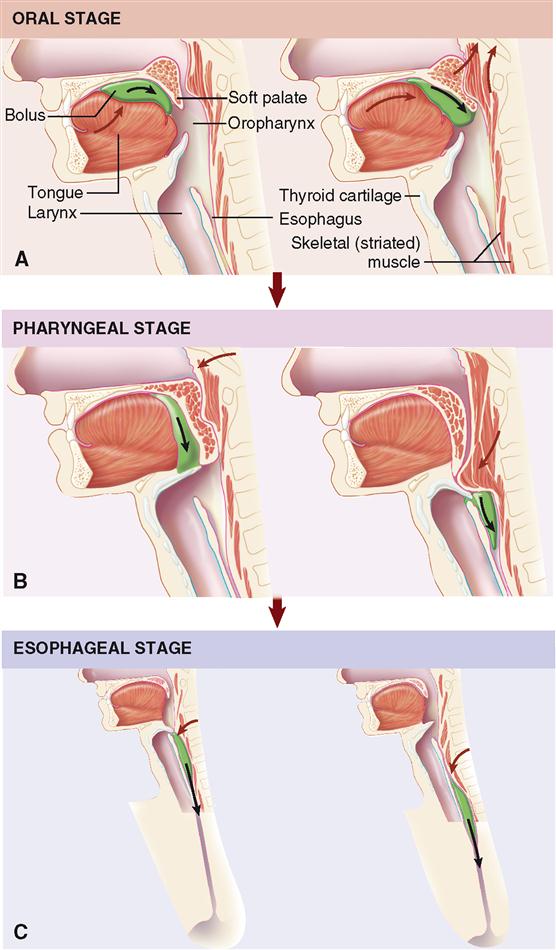
The process of swallowing, or deglutition, involves three main steps, or stages, that may be divided into the formation and then movement of a food bolus from the mouth to the stomach (Figure 29-2):
The first step, which is voluntary and under control of the cerebral cortex, involves the formation of a food bolus that is to be swallowed by means of a depression or groove in the middle of the tongue. During the oral stage, the bolus is pressed against the palate by the tongue and then moved back into the oropharynx. The pharyngeal and esophageal stages, both involuntary, consist of movement of food from the pharynx into the esophagus and, finally, into the stomach.
To propel food from the pharynx into the esophagus, three openings must be blocked: mouth, nasopharynx, and larynx. Continued elevation of the tongue seals off the mouth. The soft palate, including the uvula, is elevated and tensed, causing the nasopharynx to be closed off. Food is prevented from entering the larynx by muscle action that causes the epiglottis to block this opening. The mechanism involves raising of the larynx, a process easily noted by palpation of the thyroid cartilage during swallowing. As a result, the bolus slips over the back of the epiglottis to enter the laryngopharynx. Contractions of the pharynx and esophagus compress the bolus into and through the esophageal tube. These steps are involuntary and under control of the deglutition center in the medulla. The presence of a bolus stimulates sensory receptors in the mouth and pharynx, thus initiating reflex pharyngeal contractions. Consequently, anesthesia of sensory nerves from the mucosa of the mouth and pharynx by a drug such as procaine makes swallowing difficult or impossible.
Swallowing is a complex process requiring the coordination of many muscles and other structures in the head and neck. The process must not only occur smoothly but also take place rapidly because respiration is inhibited for the 1 to 3 seconds required for food to clear the pharynx during each swallowing.
PERISTALSIS AND SEGMENTATION
After food enters the lower portion of the esophagus, smooth muscle tissue in the wall of the GI tract takes on primary responsibility for its movement (Box 29-2). The motility produced by smooth muscle is of two main types: peristalsis and segmentation.
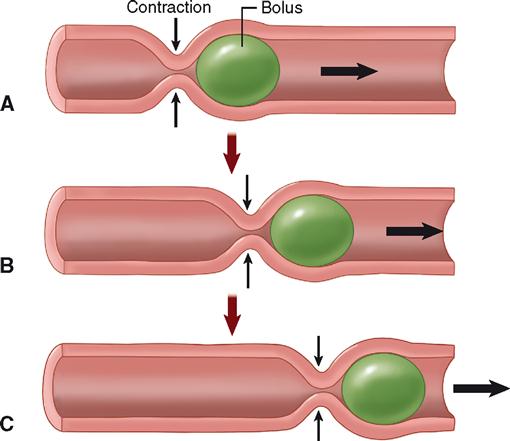
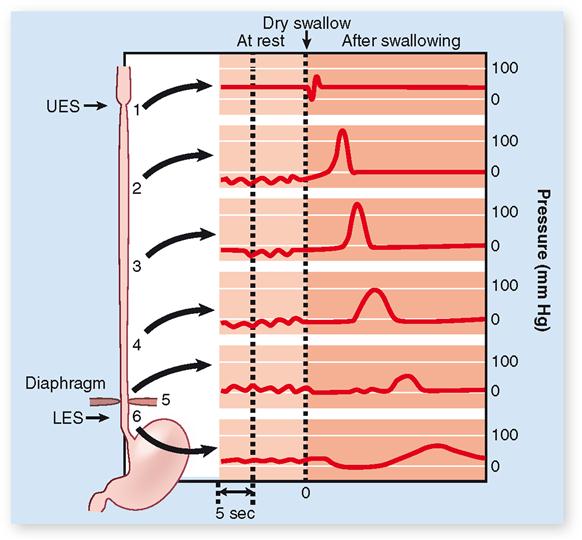
Peristalsis is often described as a wavelike ripple of the muscle layer of a hollow organ. The diagram in Figure 29-3 shows step by step how peristalsis occurs. A bolus stretches the GI wall, triggering a reflex contraction of circular muscle that pushes the bolus forward. This, in turn, triggers a reflex contraction in that location, pushing the bolus even farther. This process continues as long as the stretch reflex is activated by the presence of food. Peristalsis is a progressive kind of motility, that is, a type of motion that produces forward movement of ingested material along the GI tract. Figure 29-4 shows the effects of peristaltic contractions in the esophagus during deglutition.
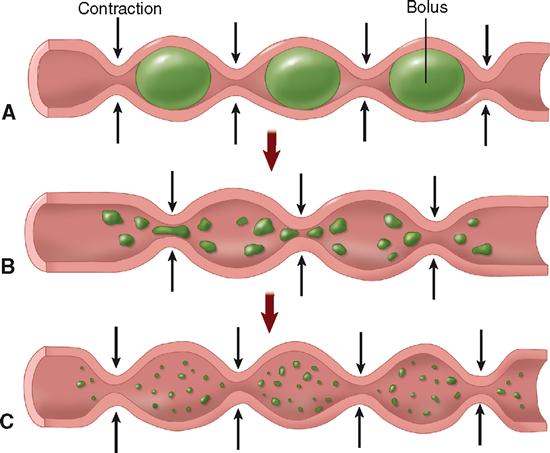
Segmentation can be described simply as mixing movement. Segmentation occurs when digestive reflexes cause a forward and backward movement within a single region, or segment, of the GI tract (Figure 29-5). Such movement helps mechanically break down food particles, mixes food and digestive juices thoroughly, and brings digested food in contact with intestinal mucosa to facilitate absorption.
Peristalsis and segmentation can occur in an alternating sequence. When this happens, food is churned and mixed as it slowly progresses along the GI tract.
REGULATION OF MOTILITY
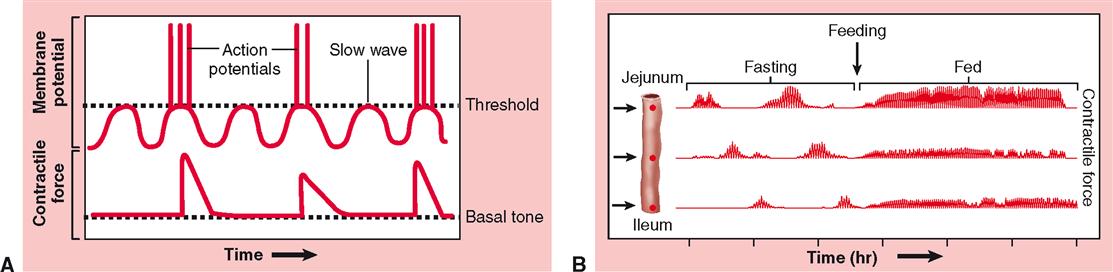
Gastric Motility
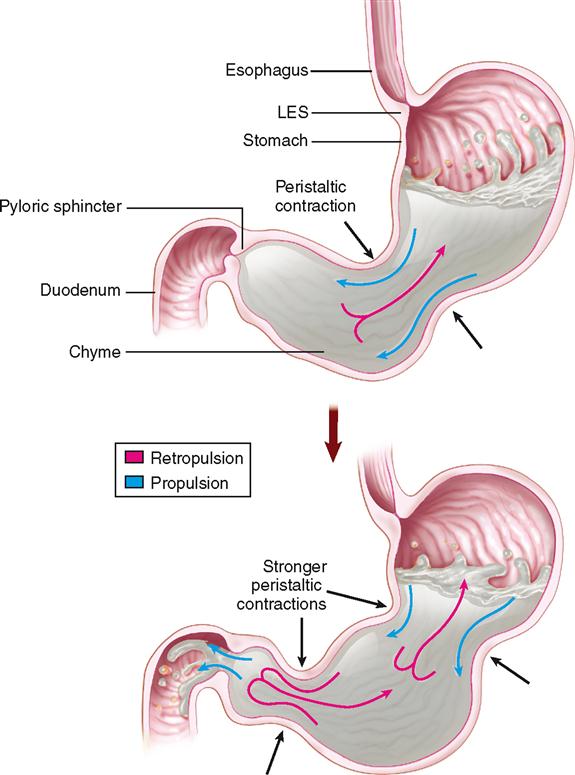
The process of emptying the stomach takes about 2 to 6 hours after a meal, depending on the amount and content of the meal. During its “storage time” in the stomach, food is churned with gastric juices to form a thick, milky material known as chyme, which is ejected about every 20 seconds into the duodenum. As you can see in Figure 29-6, while chyme is in the stomach, it is continually being pushed toward the pyloric sphincter by waves of peristaltic contractions—a process called propulsion. Because the pyloric sphincter remains closed most of the time, the chyme is forced to move backward—a process called retropulsion. Thus, because the chyme is temporarily “trapped,” peristalsis creates a sort of “back-and-forth” movement that helps mix the chyme and gastric juice. Eventually, the contraction force of the pyloric sphincter decreases, allowing a little of the chyme to pass through to the duodenum.
Because the volume of the stomach is large and that of the duodenum is small, gastric emptying must be regulated to prevent overburdening of the duodenum. Such control occurs by way of two principal mechanisms—one hormonal and one nervous. Fats and other nutrients in the duodenum stimulate the intestinal mucosa to release a hormone called gastric inhibitory peptide (GIP) into the bloodstream. When it reaches the stomach wall via the circulation, GIP has an inhibitory effect on gastric muscle, decreasing its peristalsis and thus slowing passage of food into the duodenum. Nervous control results from receptors in the duodenal mucosa that are sensitive to the presence of acid and to distention. Sensory and motor fibers in the vagus nerve then cause a reflex inhibition of gastric peristalsis. This nervous mechanism is known as the enterogastric reflex.
Box 29-3 discusses one important application of concepts of gastric motility.
INTESTINAL MOTILITY
Intestinal motility includes both peristaltic contractions and segmentation. Segmentation in the duodenum and upper jejunum mixes the incoming chyme with digestive juices from the pancreas, liver, and intestinal mucosa. This mixing action also allows the products of digestion to contact the intestinal mucosa, where they can be absorbed into the internal environment. Peristalsis continues as the chyme nears the end of the jejunum—moving the food through the rest of the small intestine and into the large intestine. After leaving the stomach, chyme normally takes about 5 hours to pass all the way through the small intestine.
Several mechanisms are involved in the control of intestinal motility. Peristalsis is regulated in part by the intrinsic stretch reflexes already described. It is also thought to be stimulated by the hormone cholecystokinin (CCK), which is secreted by endocrine cells of the intestinal mucosa when chyme is present.
A list of definitions of the different processes involved in mechanical digestion, along with the organs that accomplish them, is presented in Table 29-2.
TABLE 29-2
Processes of Mechanical Digestion
| ORGAN | MECHANICAL PROCESS | NATURE OF PROCESS |
| Mouth (teeth and tongue) | Mastication | Chewing movements—reduce size of food particles and mix them with saliva |
| Deglutition | Swallowing—movement of food from mouth to stomach | |
| Pharynx | Deglutition | See description above |
| Esophagus | Deglutition | See description above |
| Peristalsis | Rippling movements that squeeze food downward in digestive tract; a constricted ring forms first in one section, then the next, and so on, causing waves of contraction to spread along entire canal | |
| Stomach | Churning |