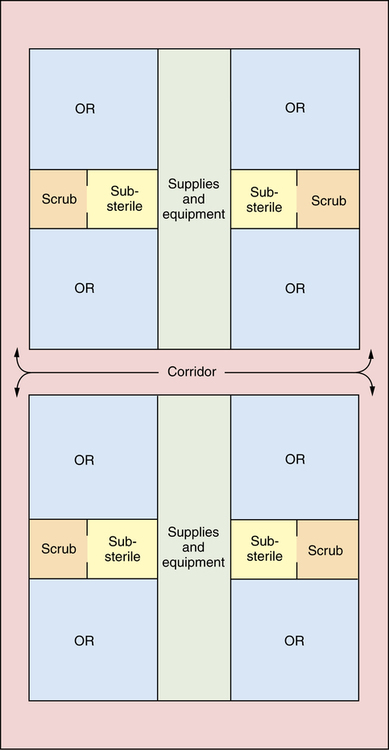
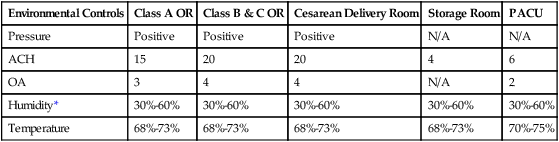
Chapter 10 After studying this chapter, the learner will be able to: • Identify specific areas within the surgical suite wherein attire and behaviors affect the manner of care delivery. • Discuss how environmental layout contributes to aseptic technique. • Describe methods of environmental controls that contribute to an aseptic environment. • Describe the specialty rooms used for endoscopy, minimally invasive procedures, and urology. The birth of a baby via an abdominal incision. Surgical procedures that use natural body orifices or percutaneous techniques with fiberoptic lighting to employ cameras and long specialized instruments during tissue manipulation and invasive intervention (e.g., colonoscopy, bronchoscopy). Interventional radiographic procedure A specialized surgical procedure that permits the use of radiologic imaging during tissue manipulation and invasive intervention through small incisional portals. A unidirectional flow of clean air from a higher plane to lower exhaust grilles. The uninterrupted flow permits higher air changes per hour (ACH) for a cleaner environment around the sterile field.1 Minimally invasive surgical (MIS) procedure Surgical procedures that use small incisions and fiberoptic lighting to employ cameras and long specialized instruments during tissue manipulation and invasive intervention (i.e., laparoscopy or mediastinoscopy). A specialized room where the actual surgery takes place. This room is one part of the restricted area of the surgical suite. A special room within the suite where sterile supplies are stored for ease of use. This room is one part of the restricted area of the surgical suite. A room with a double sink that is separated from the OR by a door and where select clean and contaminated activities take place during the process of the surgical procedure. Some substerile rooms have warming cabinets for solutions or blankets and a steam autoclave. A disposal sink for contaminated fluids might be in here (e.g., hopper). A collection of rooms that are used interactively during a surgical procedure wherein each room has a specific purpose (e.g., OR, substerile room, scrub sink room, and sterile storage core). An invisible layer of heat emanating from the equipment, team members, and the patient that can change the airflow and particulate distribution in the presence of laminar air diffusers.3,4 Efficient use of the physical facilities is important. The design of the surgical suite offers a challenge to the planning team to optimize efficiency by creating realistic traffic and workflow patterns for patients, visitors, personnel, and supplies. The design also should allow for flexibility and future expansion. Architects consult surgeons, perioperative nurses, and surgical services administrative personnel before designating functional space within the surgical suite.10 Most surgical suites are constructed according to a variation of one or more of four basic designs: 1. Central corridor, or hotel plan (Fig. 10-1). 2. Central core, or clean core plan with peripheral corridor (Fig. 10-2). 3. Combination central core and peripheral corridor, or racetrack plan (Fig. 10-3). 4. Grouping, or cluster plan with peripheral and central corridor (Fig. 10-4). Each design has its advantages and disadvantages.8,9 Efficiency is affected if corridor distances are too long in proportion to other space, if illogical relationships exist between space and function, and if inadequate consideration was given to storage space, material handling, and personnel areas. Provision must be made for traffic control. The type of design predetermines traffic patterns. Everyone—staff, patients, and visitors—should follow the delineated patterns in appropriate attire. Signs should be posted that clearly indicate the attire and environmental controls required (Table 10-1). The surgical suite is divided into three areas that are designated by the physical activities performed in each area. TABLE 10-1 Environmental Controls in the Surgical Suite *Note: Humidity is expected to decrease as low as 20% by the 2012 edition of the AIA Guidelines. The rationale is that the old 30% to 60% is based on the use of flammable anesthetics and the risk of fire by static spark, which is not a consideration in modern times. Modified from the Facility Guidelines Institute: Guidelines for design and construction of health care facilities, Chicago, 2010, ASHE (American Society for Healthcare Engineering), available at www.fgiguidelines.org/2010guidelines.html. The area must ensure privacy and offer 80 ft2 per patient of space to accommodate a transport cart.a It may be compartmentalized with individual cubicles or be an open area with curtains. Curtains do not deflect sound and offer little privacy when the nurse is performing assessment and having conversations with the patient. Curtains also accumulate dust and particles and should be laundered on a regular basis. Assignment and scheduling boards should not be within the view of the patients to avoid breaching privacy standards. When wipe-off boards are used for daily scheduling, care is taken not to use patient names. Coordination of the holding room staff and the personnel managing the surgical schedule is essential to prevent delays. More information about preoperative patient care areas is available in Chapter 21. Hospitals and ambulatory care facilities accommodate patients and their families during the perioperative waiting period. A designated waiting area is provided for families of surgical patients. This is most conveniently located outside the surgical suite adjacent to the recovery area. More information about the PACU can be found in Chapter 30.
Physical facilities
Physical layout of the surgical suite
Type of physical plant design
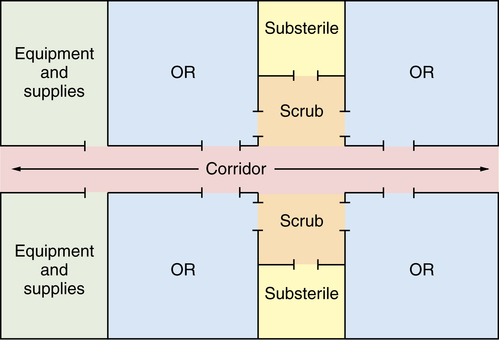
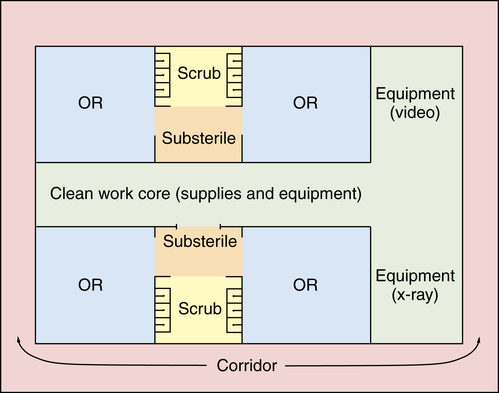
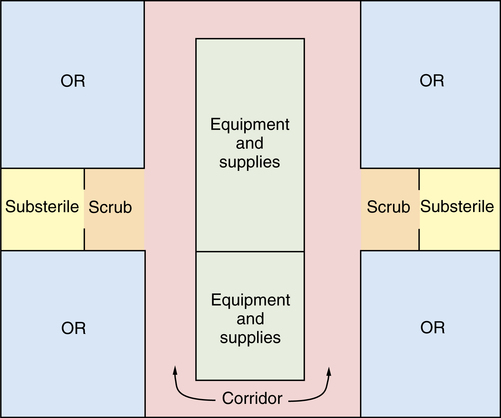
Space allocation and traffic patterns
Environmental Controls
Class A OR
Class B & C OR
Cesarean Delivery Room
Storage Room
PACU
Pressure
Positive
Positive
Positive
N/A
N/A
ACH
15
20
20
4
6
OA
3
4
4
N/A
2
Humidity*
30%-60%
30%-60%
30%-60%
30%-60%
30%-60%
Temperature
68%-73%
68%-73%
68%-73%
68%-73%
70%-75%
Transition zones
Preoperative admission and holding unit
Postanesthesia care unit
Peripheral support areas
Basicmedical Key
Fastest Basicmedical Insight Engine

 Website
Website