32
Pharmacotherapy of Gastric Acidity, Peptic Ulcers, and Gastroesophageal Reflux Disease
This chapter will be most useful after having a basic understanding of the material in Chapter 45, Pharmacotherapy of Gastric Acidity, Peptic Ulcers, and Gastroesophageal Reflux Disease in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition. In addition to the material presented here, the 12th Edition contains:
• A description of the physiology of gastric secretion
• Therapeutic strategies for the treatment of specific acid-peptic disorders
• Table 45-2 which shows the composition and acid neutralizing capacities of popular antacid preparations
LEARNING OBJECTIVES
 Identify the sites in the gastric parietal cell where drugs act to suppress acid secretion.
Identify the sites in the gastric parietal cell where drugs act to suppress acid secretion.
 Describe the mechanism of action of proton pump inhibitors, H2 receptor antagonists, and prostaglandin analogs to suppress gastric acid secretion.
Describe the mechanism of action of proton pump inhibitors, H2 receptor antagonists, and prostaglandin analogs to suppress gastric acid secretion.
 Describe the limitations to the use of H2 receptor antagonists in chronic acid suppression.
Describe the limitations to the use of H2 receptor antagonists in chronic acid suppression.
 Identify potential drug interactions with proton pump inhibitors and H2 receptor antagonists.
Identify potential drug interactions with proton pump inhibitors and H2 receptor antagonists.
 Describe the mechanism of action of drugs that enhance gastric cytoprotection.
Describe the mechanism of action of drugs that enhance gastric cytoprotection.
 Describe the recommendations for therapy of gastroesophageal reflux disease (GERD) and peptic ulcer disease.
Describe the recommendations for therapy of gastroesophageal reflux disease (GERD) and peptic ulcer disease.
 Understand the role of Helicobacter pylori infection in peptic ulcer disease and the therapeutic principles for its eradication.
Understand the role of Helicobacter pylori infection in peptic ulcer disease and the therapeutic principles for its eradication.
 Describe appropriate therapy for NSAID-induced ulcers.
Describe appropriate therapy for NSAID-induced ulcers.
DRUGS INCLUDED IN THIS CHAPTER
Cimetidine (TAGAMET, others)
Dexlansoprazole (KAPIDEX)
Esomeprazole (NEXIUM)
Famotidine (PEPSID, others)
Lansoprazole (PREVACID)
Misoprostol (CYTOTEC)
Nizatidine (AXID, others)
Omeprazole (PRILOSEC, others)
Pantoprazole (PROTONIX)
Rabeprazole (ACIPHEX)
Ranitidine (ZANTEC, others)
Sucralfate (CARAFATE, others)
MECHANISMS OF ACTION OF DRUGS USED TO TREAT GASTRIC ACID DISEASES
A 42-year-old woman is seen because of worsening heartburn during the past week. She was first diagnosed with GERD 1 month ago and treatment was begun with cimetidine 400 mg once daily. Two weeks later the cimetidine dosage was increased to 400 mg twice daily.
a. What is the reason for the worsening of her GERD symptoms?
Cimetidine is an H2 receptor antagonist and tolerance to acid suppressing effects of these drugs has been shown to develop as early as 2 to 5 days after beginning treatment. One mechanism for this phenomenon is secondary to the hypergastrinemia that stimulates histamine release and overcomes the H2 receptor blockade.
b. What are the mechanisms of action of H2 receptor blockers and proton pump inhibitors?
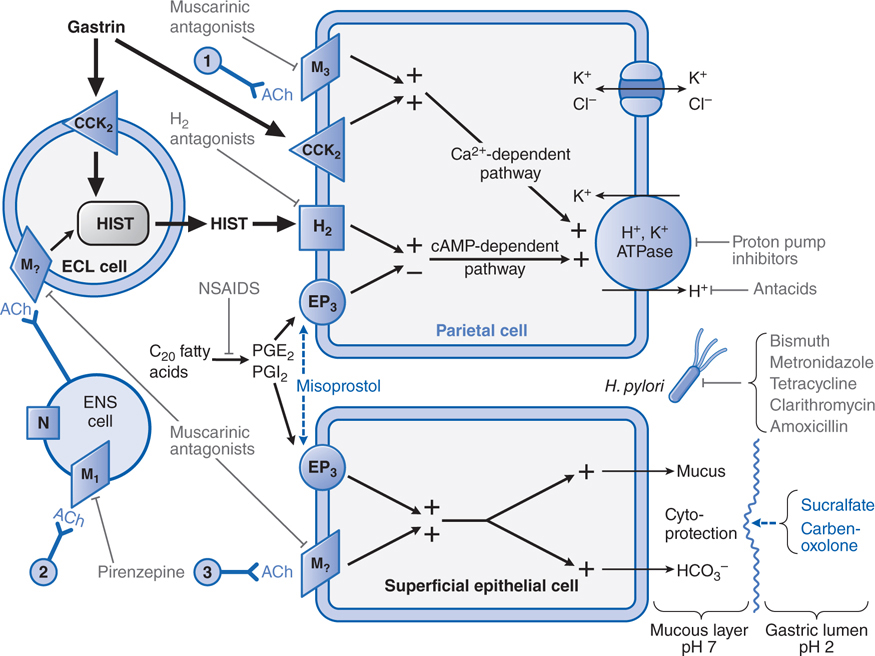
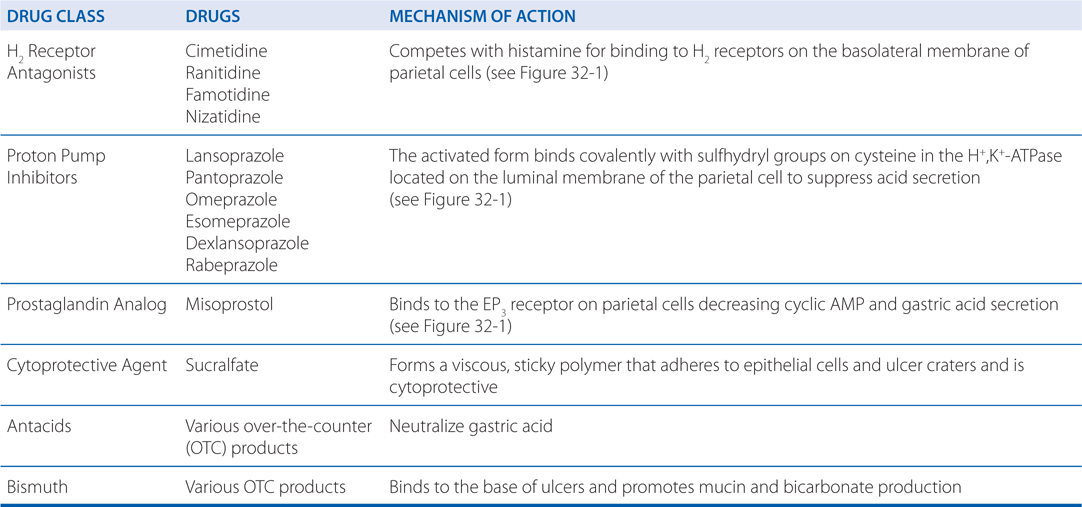
The mechanisms of action of these drugs is shown in Figure 32-1. The H2 receptor blockers suppress gastric acid secretion by competing with histamine for binding to H2 receptors on the basolateral membrane of parietal cells. The structural similarity of the H2 receptor antagonists and histamine is shown in Figure 32-2.
FIGURE 32-1 Physiological and pharmacological regulation of gastric secretion: the basis for therapy of acid-peptic disorders. Shown are the interactions among an enterochromaffin-like (ECL) cell that secretes histamine, a ganglion cell of the enteric nervous system (ENS), a parietal cell that secretes acid, and a superficial epithelial cell that secretes mucus and bicarbonate. Physiological pathways, shown in solid black, may be stimulatory (+) or inhibitory (–). 1 and 3 indicate possible inputs from postganglionic cholinergic fibers; 2 shows neural input from the vagus nerve. Physiological agonists and their respective membrane receptors include acetylcholine (ACh), muscarinic (M), and nicotinic (N) receptors; gastrin, cholecystokinin receptor 2 (CCK2); histamine (HIST), H2 receptor; and prostaglandin E2 (PGE2), EP3 receptor. A gray indicates targets of pharmacological antagonism. A blue dashed arrow indicates a drug action that mimics or enhances a physiological pathway. Shown in gray are drugs used to treat acid-peptic disorders. NSAIDs are nonsteroidal anti-inflammatory drugs, which can induce ulcers via inhibition of cyclooxygenase (see Chapter 22).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree