Patient Story
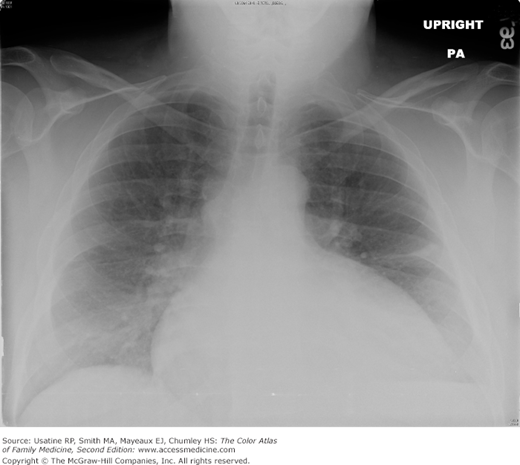
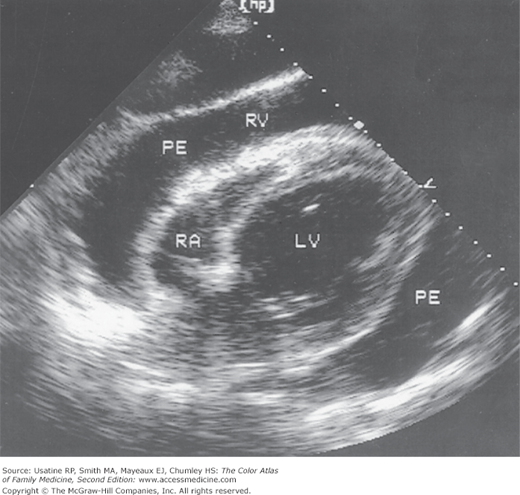
A 30-year-old woman presented to her family physician with increasing shortness of breath over the past 2 weeks. Prior to this, she had a flu-like illness and felt like she never recovered. She denied chest pain and edema, did not take any medications, and had not had any recent trauma or surgery. She had a normal examination. Her chest radiograph showed a classic globular heart as demonstrated in Figure 49-1. She had nonspecific ST changes on her ECG. An echocardiogram confirmed pericardial effusion (Figure 49-2). The underlying etiology was not elucidated and she recovered spontaneously over the next several months.
Introduction
Pericardial effusions are commonly found in the general population and the incidence increases with age. They can be caused by cardiac disease or surgery, connective tissue disorders, neoplasms, infections, renal disease, hypothyroidism, or medications; however, a cause is identified only 50% of the time. The definitive diagnosis is made by echocardiography.
Epidemiology
- Six-and-a-half percent of adults (<1% ages 20 to 30 years; 15% older than 80 years of age) had echocardiogram findings consistent with pericardial effusion in a population-based study of 5652 adults and adult family members of participants in the Framingham Heart Study.1
- Seventy-seven percent of patients after cardiac surgery for valves or bypass have pericardial effusions, which rarely (<1%) require therapy.2
- Forty percent of healthy pregnant women have small, asymptomatic pericardial effusions in the third trimester.3
Etiology and Pathophysiology
Risk Factors
- Congestive heart failure from other cardiac diseases, such as rheumatic heart disease, cor pulmonale, or cardiomyopathy.6
- After cardiac surgery or after a myocardial infarction.2
- Connective tissue disorders (scleroderma, lupus erythematosus, rheumatoid arthritis).6
- Neoplasms: benign (atrial myxoma); primary malignant (mesothelioma); secondary malignant (i.e., lung or breast cancer).6
- Chronic renal disease (uremia or hemodialysis) or other causes of hypoalbuminemia.
- Infections: acute (enterovirus, adenovirus, influenza virus, Streptococcus pneumonia, Coxiella burnetii—responsible for Q fever) or chronic (tuberculosis, fungus, parasites).4
- Medications (procainamide, hydralazine) or after radiation.6
- Severe hypothyroidism with myxedema.6
Diagnosis
Clinical features, chest radiograph, and electrocardiogram suggest pericardial effusion, which is confirmed by echocardiogram. The underlying etiology is identifiable in approximately 50% of cases.