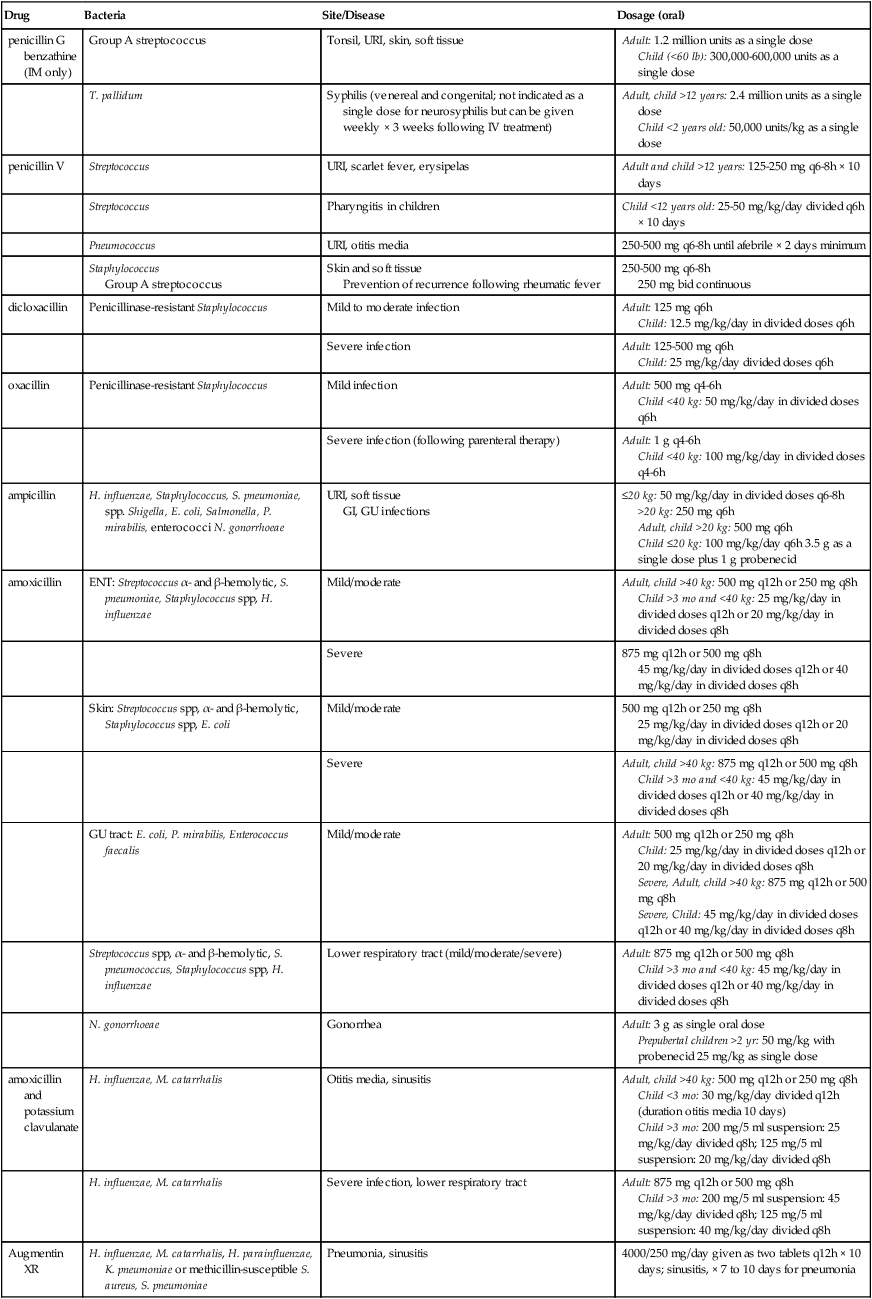
penicillin G benzathine (IM only) |
Group A streptococcus |
Tonsil, URI, skin, soft tissue |
Adult: 1.2 million units as a single dose
Child (<60 lb): 300,000-600,000 units as a single dose |
|
T. pallidum |
Syphilis (venereal and congenital; not indicated as a single dose for neurosyphilis but can be given weekly × 3 weeks following IV treatment) |
Adult, child >12 years: 2.4 million units as a single dose
Child <2 years old: 50,000 units/kg as a single dose |
penicillin V |
Streptococcus |
URI, scarlet fever, erysipelas |
Adult and child >12 years: 125-250 mg q6-8h × 10 days |
|
Streptococcus |
Pharyngitis in children |
Child <12 years old: 25-50 mg/kg/day divided q6h × 10 days |
|
Pneumococcus |
URI, otitis media |
250-500 mg q6-8h until afebrile × 2 days minimum |
|
Staphylococcus
Group A streptococcus |
Skin and soft tissue
Prevention of recurrence following rheumatic fever |
250-500 mg q6-8h
250 mg bid continuous |
dicloxacillin |
Penicillinase-resistant Staphylococcus |
Mild to moderate infection |
Adult: 125 mg q6h
Child: 12.5 mg/kg/day in divided doses q6h |
|
|
Severe infection |
Adult: 125-500 mg q6h
Child: 25 mg/kg/day divided doses q6h |
oxacillin |
Penicillinase-resistant Staphylococcus |
Mild infection |
Adult: 500 mg q4-6h
Child <40 kg: 50 mg/kg/day in divided doses q6h |
|
|
Severe infection (following parenteral therapy) |
Adult: 1 g q4-6h
Child <40 kg: 100 mg/kg/day in divided doses q4-6h |
ampicillin |
H. influenzae, Staphylococcus, S. pneumoniae, spp. Shigella, E. coli, Salmonella, P. mirabilis, enterococci N. gonorrhoeae |
URI, soft tissue
GI, GU infections |
≤20 kg: 50 mg/kg/day in divided doses q6-8h
>20 kg: 250 mg q6h
Adult, child >20 kg: 500 mg q6h
Child ≤20 kg: 100 mg/kg/day q6h 3.5 g as a single dose plus 1 g probenecid |
amoxicillin |
ENT: Streptococcus α- and β-hemolytic, S. pneumoniae, Staphylococcus spp, H. influenzae |
Mild/moderate |
Adult, child >40 kg: 500 mg q12h or 250 mg q8h
Child >3 mo and <40 kg: 25 mg/kg/day in divided doses q12h or 20 mg/kg/day in divided doses q8h |
|
|
Severe |
875 mg q12h or 500 mg q8h
45 mg/kg/day in divided doses q12h or 40 mg/kg/day in divided doses q8h |
|
Skin: Streptococcus spp, α- and β-hemolytic, Staphylococcus spp, E. coli |
Mild/moderate |
500 mg q12h or 250 mg q8h
25 mg/kg/day in divided doses q12h or 20 mg/kg/day in divided doses q8h |
|
|
Severe |
Adult, child >40 kg: 875 mg q12h or 500 mg q8h
Child >3 mo and <40 kg: 45 mg/kg/day in divided doses q12h or 40 mg/kg/day in divided doses q8h |
|
GU tract: E. coli, P. mirabilis, Enterococcus faecalis |
Mild/moderate |
Adult: 500 mg q12h or 250 mg q8h
Child: 25 mg/kg/day in divided doses q12h or 20 mg/kg/day in divided doses q8h
Severe, Adult, child >40 kg: 875 mg q12h or 500 mg q8h
Severe, Child: 45 mg/kg/day in divided doses q12h or 40 mg/kg/day in divided doses q8h |
|
Streptococcus spp, α- and β-hemolytic, S. pneumococcus, Staphylococcus spp, H. influenzae |
Lower respiratory tract (mild/moderate/severe) |
Adult: 875 mg q12h or 500 mg q8h
Child >3 mo and <40 kg: 45 mg/kg/day in divided doses q12h or 40 mg/kg/day in divided doses q8h |
|
N. gonorrhoeae |
Gonorrhea |
Adult: 3 g as single oral dose
Prepubertal children >2 yr: 50 mg/kg with probenecid 25 mg/kg as single dose |
amoxicillin and potassium clavulanate |
H. influenzae, M. catarrhalis |
Otitis media, sinusitis |
Adult, child >40 kg: 500 mg q12h or 250 mg q8h
Child <3 mo: 30 mg/kg/day divided q12h (duration otitis media 10 days)
Child >3 mo: 200 mg/5 ml suspension: 25 mg/kg/day divided q8h; 125 mg/5 ml suspension: 20 mg/kg/day divided q8h |
|
H. influenzae, M. catarrhalis |
Severe infection, lower respiratory tract |
Adult: 875 mg q12h or 500 mg q8h
Child >3 mo: 200 mg/5 ml suspension: 45 mg/kg/day divided q8h; 125 mg/5 ml suspension: 40 mg/kg/day divided q8h |
Augmentin XR |
H. influenzae, M. catarrhalis, H. parainfluenzae, K. pneumoniae or methicillin-susceptible S. aureus, S. pneumoniae |
Pneumonia, sinusitis |
4000/250 mg/day given as two tablets q12h × 10 days; sinusitis, × 7 to 10 days for pneumonia |
![]()
![]()