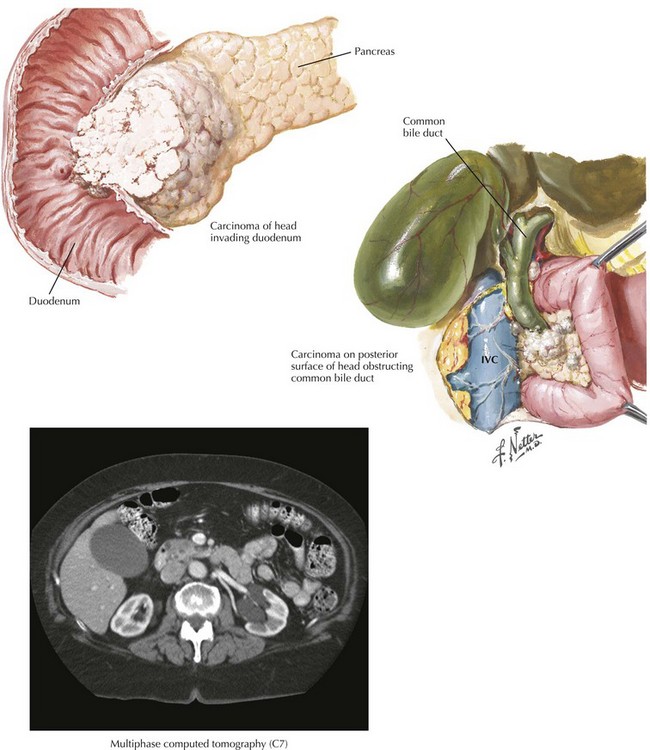
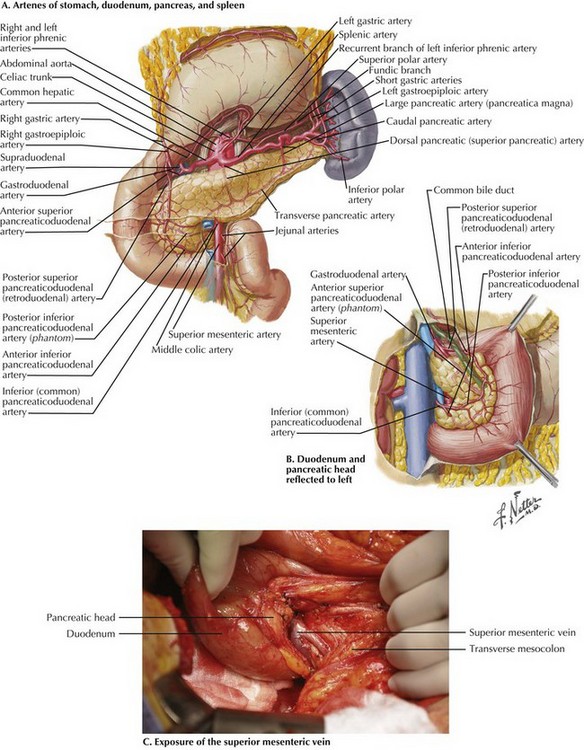
Chapter 16 Resection of tumors of the periampullary region has its origins in the writings of Kausch (1912) and Whipple (1935). Pancreaticoduodenectomy, or pancreatoduodenectomy, previously was accompanied by a mortality rate of 20% to 25%. Currently, however, most experienced pancreatic surgery centers report a mortality rate of 3% or less. Complication rates remain 20% to 50%, with the most troublesome complication being leakage at the pancreatic anastomosis. The treatment of pancreatic cancer begins with accurate staging, including a complete history and physical examination. The most important component of staging is a multiphase computed tomography (CT) scan of the abdomen using a multidetector scanner (Fig. 16-1). With CT of the chest, this allows patients to be staged clinically as resectable (15% to 25%), borderline resectable or locally advanced/unresectable (30% to 40%), or metastatic (40% to 50%). Endoscopic ultrasound is rarely needed for staging purposes, and laparoscopy is favored by some authors. Debate continues about the utility of preoperative biliary decompression in jaundiced patients. Recently, laparoscopic approaches to pancreaticoduodenectomy have been described, but these remain nascent. The dissection begins with a generous Kocher maneuver to lyse the lateral retroperitoneal attachments of the duodenum (Fig. 16-2, A and B). This elevates the duodenum and head of the pancreas out of the retroperitoneum. By taking the Kocher maneuver to its fullest extent, the surgeon identifies the superior mesenteric vein (SMV) in the groove between the head of the pancreas and the transverse mesocolon (Fig. 16-2, C). Further, the relationship of the tumor in the head of the pancreas to the SMV and superior mesenteric artery (SMA) is assessed. At this point, the surgeon should feel for evidence of a replaced or accessory right hepatic artery coming off the SMA (Fig. 16-3).
Pancreaticoduodenectomy
Introduction
Principles of Pancreatic Cancer Treatment
Surgical Approach
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine