The gastrointestinal (GI) system is composed of the mouth, esophagus, stomach, small intestine, and large intestine. Digestion, which is primarily a function of the small intestine, is the process by which starches, proteins, lipids, nucleic acids, and other complex molecules are degraded to simple constituents (molecules) for absorption and use in the body. This chapter discusses the physiology and biochemistry of gastric secretion, intestinal physiology, pathologic aspects of intestinal function, and tests of gastric and intestinal function.
The pancreas is a large gland that is involved in the digestive process but located outside of the GI system. It is composed of both endocrine and exocrine tissues. The liver is the other major external gland that is involved in the digestive process, and it is covered in Chapter 25. The endocrine functions of the pancreas include production of insulin and glucagon; both hormones are involved in carbohydrate metabolism. Exocrine function involves the production of many enzymes used in the digestive process. This chapter discusses the physiology of pancreatic function, diseases of the pancreas, and tests of pancreatic function.
PHYSIOLOGY OF PANCREATIC FUNCTION
As a digestive gland, the pancreas is only second in size to the liver, weighing about 70 to 105 g. It is located behind the peritoneal cavity across the upper abdomen at about the level of the first and second lumbar vertebrae, about 1 to 2 in. above the umbilicus. It is located in the curve made by the duodenum (Fig. 28.1). The pancreas is composed of two morphologically and functionally different tissues: endocrine tissue and exocrine tissue. The endocrine (hormone-releasing) component is by far the smaller of the two and consists of the islets of Langerhans, which are well-delineated, spherical or ovoid clusters composed of at least four different cell types. The islet cells secrete at least four hormones into the blood: insulin, glucagon, gastrin, and somatostatin. The larger, exocrine pancreatic (enzyme-secreting) component secretes about 1.5 to 2 L/d of fluid, which is rich in digestive enzymes, into ducts that ultimately empty into the duodenum.
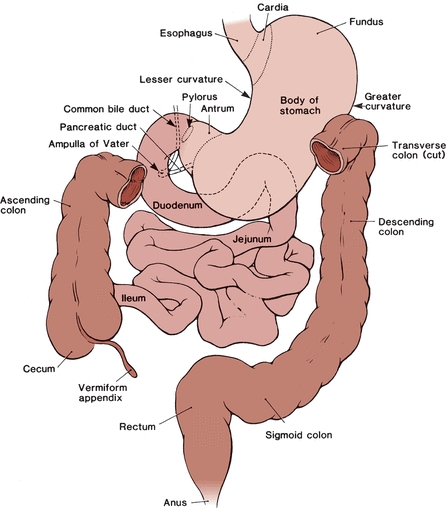
FIGURE 28.1 Peritoneum and mesenteries. The parietal peritoneum lines the abdominal cavity, and the visceral peritoneum covers abdominal organs. Retroperitoneal organs are covered by the parietal peritoneum. The mesenteries are membranes that connect abdominal organs to each other and to the body wall. (Reprinted from Thompson JS, Akesson EJ, eds. Thompson’s Core Textbook of Anatomy. 2nd ed. Philadelphia, PA: JB Lippincott; 1990:115, with permission.)
This digestive fluid is produced by pancreatic acinar cells (grape-like clusters), which line the pancreas and are connected by small ducts. These small ducts empty into progressively larger ducts, eventually forming one major pancreatic duct and a smaller accessory duct. The major pancreatic duct and the common bile duct open into the duodenum at the major duodenal papilla (Fig. 28.2). Normal, protein-rich, pancreatic fluid is clear, colorless, and watery, with an alkaline pH that can reach up to 8.3. This alkalinity is caused by the high concentration of sodium bicarbonate present in pancreatic fluid, which is used eventually to neutralize the hydrochloric acid in gastric fluid from the stomach as it enters the duodenum. The bicarbonate and chloride concentrations vary reciprocally so that they total about 150 mmol/L.

FIGURE 28.2 Diagram of the pancreas and its relationship to the duodenum.
Pancreatic fluid has about the same concentrations of potassium and sodium as serum. The digestive enzymes, or their proenzymes secreted by the pancreas, are capable of digesting the three major classes of food substances (proteins, carbohydrates, and fats) and include (1) the proteolytic enzymes trypsin, chymotrypsin, elastase, collagenase, leucine aminopeptidase, and some carboxypeptidases; (2) lipid-digesting enzymes, primarily lipase and lecithinase; (3) carbohydrate-splitting pancreatic amylase; and (4) several nucleases (ribonuclease), which separate the nitrogen-containing bases from their sugar-phosphate strands.
Pancreatic activity is under both nervous and endocrine control. Branches of the vagus nerve can cause a small amount of pancreatic fluid secretion when food is smelled or seen, and these secretions may increase as the bolus of food reaches the stomach. Most of the pancreatic action, however, is under the hormonal control of secretin and cholecystokinin (CCK; formerly called pancreozymin). Secretin is responsible for the production of bicarbonate-rich and, therefore, alkaline pancreatic fluid, which protects the lining of the intestine from damage. Secretin is synthesized in response to the acidic contents of the stomach reaching the duodenum. It can also affect gastrin activity in the stomach. This pancreatic fluid contains few digestive enzymes. CCK, in the presence of fats or amino acids in the duodenum, is produced by the cells of the intestinal mucosa and is responsible for release of enzymes from the acinar cells by the pancreas into the pancreatic fluid.
DISEASES OF THE PANCREAS
Other than trauma, only three diseases cause more than 95% of the medical attention devoted to the pancreas. If they affect the endocrine function of the pancreas, these diseases can result in altered digestion and nutrient metabolism. The role of the pancreas in diabetes mellitus is discussed in Chapter 14.
Cystic fibrosis (known by various other terms, such as fibrocystic disease of the pancreas and mucoviscidosis) is an inherited autosomal recessive disorder characterized by dysfunction of mucous and exocrine glands throughout the body. The disease is relatively common and occurs in about 1 of 1,600 live births. It has various manifestations and can initially present in such widely varying ways as intestinal obstruction of the newborn, excessive pulmonary infections in childhood, or, uncommonly, as pancreatogenous malabsorption in adults. The disease causes the small and large ducts and the acini to dilate and convert into small cysts filled with mucus, eventually resulting in the prevention of pancreatic secretions reaching the duodenum or, depending on the age of the patient, a plug that blocks the lumen of the bowel, leading to obstruction. As the disease progresses, there is increased destruction and fibrous scarring of the pancreas and a corresponding decrease in function. Cystic fibrosis is transmitted as an autosomal recessive disorder with a high degree of penetrance. It occurs primarily in persons of Northern European descent. The cystic fibrosis gene known as CFTR occurs on chromosome 7, and more than 900 mutations causing this disorder have been identified; however, some occur more commonly than others. In areas of high frequency, such as Brittany in Western France, more than 10% of the population may carry a cystic fibrosis mutation, and 1 in 3,000 infants may be affected, making it the most common genetic disorder in these populations. Genetic screening is now widely carried out.1, 2, 3
Pancreatic carcinoma is the fourth most frequent form of fatal cancer and causes about 38,000 deaths each year in the United States, which represents about 7% of all deaths from malignant neoplasms. The disease is slightly more common in males than in females and in African Americans than in Whites. The 5-year survival rate is about 6%, and most patients die within 1 year of diagnosis. Most pancreatic tumors arise as adenocarcinomas of the ductal epithelium. Because the pancreas has a rich supply of nerves, pain is a prominent feature of the disease. If the tumor arises in the body or tail of the pancreas, detection does not often occur until an advanced stage of the disease because of its central location and the associated vague symptoms. Cancer of the head of the pancreas is usually detected earlier because of its proximity to the common bile duct. Signs of these tumors are jaundice, weight loss, anorexia, and nausea. Jaundice is associated with signs of posthepatic hyperbilirubinemia (intrahepatic cholestasis) and low levels of fecal bilirubin, resulting in clay-colored stools. However, findings are not specific for pancreatic tumors, and other causes of obstruction must be ruled out.
Islet cell tumors of the pancreas affect the endocrine capability of the pancreas. If the tumor occurs in beta cells, hyperinsulinism is often seen, resulting in low blood glucose levels, sometimes followed by hypoglycemic shock. Pancreatic cell tumors, which overproduce gastrin, are called gastrinomas; they cause Zollinger-Ellison syndrome and can be duodenal in origin. These tumors are associated with watery diarrhea, recurring peptic ulcer, and significant gastric hypersecretion and hyperacidity. Pancreatic cell glucagon-secreting tumors are rare; the hypersecretion of glucagon is associated with diabetes mellitus.
Pancreatitis, or inflammation of the pancreas, is ultimately caused by autodigestion of the pancreas as a result of reflux of bile or duodenal contents into the pancreatic duct. Pathologic changes can include acute edema, with large amounts of fluid accumulating in the retroperitoneal space and an associated decrease in effective circulating blood volume; cellular infiltration, leading to necrosis of the acinar cells, with hemorrhage as a possible result of necrotic blood vessels; and intrahepatic and extrahepatic pancreatic fat necrosis. Pancreatitis is generally classified as acute (no permanent damage to the pancreas), chronic (irreversible injury), or relapsing/recurrent, which can also be acute or chronic. It commonly occurs in midlife. Painful episodes can occur intermittently, usually reaching a maximum within minutes or hours, lasting for several days or weeks, and frequently accompanied by nausea and vomiting. Pancreatitis is often associated with alcohol abuse or biliary tract diseases such as gallstones, but patients with hyperlipoproteinemia and those with hyperparathyroidism are also at a significantly increased risk for this disease.
Other etiologic factors associated with acute pancreatitis include mumps, obstruction caused by biliary tract disease, gallstones, pancreatic tumors, tissue injury, atherosclerotic disease, shock, pregnancy, hypercalcemia, hereditary pancreatitis, immunologic factors associated with postrenal transplantation, and hypersensitivity. Symptoms of acute pancreatitis include severe abdominal pain that is generalized or in the upper quadrants and often radiates toward the back or down the right or left flank. The etiology of chronic pancreatitis is similar to that of acute pancreatitis, but chronic excessive alcohol consumption appears to be the most common predisposing factor.
Laboratory findings include increased amylase, lipase, triglycerides, and hypercalcemia, which is often associated with underlying hyperparathyroidism. Hypocalcemia may be found and has been attributed to the sudden removal of large amounts of calcium from the extracellular fluid because of impaired mobilization or as a result of calcium fixation by fatty acids liberated by increased lipase action on triglycerides. Hypoproteinemia is attributable mainly to the notable loss of plasma into the retroperitoneal space. A shift of arterial blood flow from the inflamed pancreatic cells to less affected or normal cells causes oxygen deprivation and tissue hypoxia in the area of damage, including the surrounding organs and tissue.
All three conditions can result in severely diminished pancreatic exocrine function, which can significantly compromise digestion and absorption of ingested nutrients. This is the essence of the general malabsorption syndrome, which embodies abdominal bloating and discomfort; the frequent passage of bulky, malodorous feces; and weight loss. Failure to digest or absorb fats, known as steatorrhea, renders a greasy appearance to feces (more than 5 g of fecal fat per 24 hours). The malabsorption syndrome typically involves abnormal digestion or absorption of proteins, polysaccharides, carbohydrates, and other complex molecules, as well as lipids. Severely deranged absorption and metabolism of electrolytes, water, vitamins (particularly fat-soluble vitamins A, D, E, and K), and minerals can also occur. Malabsorption can involve a single substance, such as vitamin B12, which results in a megaloblastic anemia (pernicious anemia), or lactose caused by a lactase deficiency. In addition to pancreatic exocrine deficiency, the malabsorption syndrome can be caused by biliary obstruction, which deprives the small intestine of the emulsifying effect of bile, and various diseases of the small intestine, which inhibit absorption of digested products.
TESTS OF PANCREATIC FUNCTION
Depending on etiology and clinical picture, pancreatic function may be suspect when there is evidence of increased amylase and lipase.4, 5, 6, 7 The reader is referred to Chapter 13 for an in-depth discussion of these enzymes. Other laboratory tests of pancreatic function include those used for detection of malabsorption (e.g., examination of stool for excess fat, d-xylose test, and fecal fat analysis), tests measuring other exocrine function (e.g., secretin, CCK, fecal fat, trypsin, and chymotrypsin), tests assessing changes associated with extrahepatic obstruction (e.g., bilirubin), and endocrine-related tests (e.g., gastrin, insulin, and glucose) that reflect changes in the endocrine cells of the pancreas.
Direct evaluation of pancreatic fluid may include measurement of the total volume of pancreatic fluid and the amount or concentration of bicarbonate and enzymes, which requires pancreatic stimulation. Stimulation may be accomplished using a predescribed meal or administration of secretin, which allows for volume and bicarbonate evaluation, or secretin stimulation followed by CCK stimulation, which adds enzymes to the pancreatic fluid evaluation. The advantage of these tests, both of which require intubation of the patient, is that the chemical and cytologic examinations are performed on actual pancreatic secretions. Cytologic examination of the fluid can often establish the presence, or at least the suspicion, of malignant neoplasms, although the precise localization of the primary organ of involvement (i.e., pancreas, biliary system, ampulla of Vater, or duodenum) is not possible by duodenal aspiration.
Because of advances in imaging techniques, these stimulation tests are used less often; none have proved especially useful in diagnosis of mild or acute pancreatic disease in which the acute phase has subsided. Most of the tests have found clinical utility in excluding the pancreas from diagnosis. The sweat test, used for screening cystic fibrosis, is not specific for assessing pancreatic involvement but, when used along with the clinical picture at the time of testing, can provide important diagnostic information. The following pancreatic function tests are reviewed briefly: secretin/CCK test, fecal fat analysis, sweat chloride determinations, and amylase and lipase interpretation.
CASE STUDY 28.1
A 38-year-old man entered the emergency department with the complaint of severe, midabdominal pain of 6 hours’ duration. A friend, who had driven him to the hospital, stated that the patient fainted three times as he was being helped into the automobile. The patient had a 15-year history of alcoholism and drank 1 to 2 pints of whiskey everyday. He had last been hospitalized for acute alcoholism 3 months ago, at which time he had relatively minor abnormalities of liver function. On this admission, his blood pressure was 80/40 mm Hg; pulse, 110 beats/min and thready; and respirations, 24 breaths per minute and shallow. Clinical laboratory test results are shown in Case Study Table 28.1.1.
CASE STUDY TABLE 28.1.1 Laboratory Results
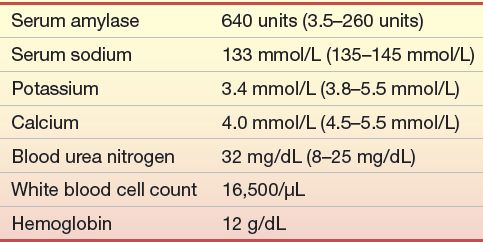
Questions
1. What is the probable disease?
2. What is the cause for the low serum calcium?
3. What is the cause for the increased blood urea nitrogen?
Secretin/CCK Test
The secretin/CCK test is a direct determination of the exocrine secretory capacity of the pancreas. The test involves intubation of the duodenum without contamination by gastric fluid, which would neutralize any bicarbonate. The test is performed after a 6-hour or overnight fast. Pancreatic secretion is stimulated by intravenously administered secretin in a dose varying from 2 to 3 U/kg of body weight, followed by CCK administration. If a simple secretin test is desired, the higher dose of secretin is given alone.
No single protocol has been uniformly established for the test. Pancreatic secretions are collected variously for 30, 60, or 80 minutes after administration of the stimulants, either as 10-minute specimens or as a single, pooled collection. The pH, secretory rate, enzyme activities (e.g., trypsin, amylase, or lipase), and amount of bicarbonate are determined. The average amount of bicarbonate excreted per hour is about 15 mmol/L for men and 12 mmol/L for women, with an average flow of 2 mL/kg. Assessment of enzymes must be taken in view of total volume output. Decreased pancreatic flow is associated with pancreatic obstruction and increase in enzyme concentrations. Low concentrations of bicarbonate and enzymes are associated with cystic fibrosis, chronic pancreatitis, pancreatic cysts, calcification, and edema of the pancreas.
CASE STUDY 28.2
A 56-year-old man who is an alcoholic presents with a 2-week history of midabdominal pain. He also describes clay-colored stools, mild icterus, nausea, vomiting, and a 10-lb weight loss. Laboratory findings are shown in Case Study Table 28.2.1.
CASE STUDY TABLE 28.2.1 Laboratory Results
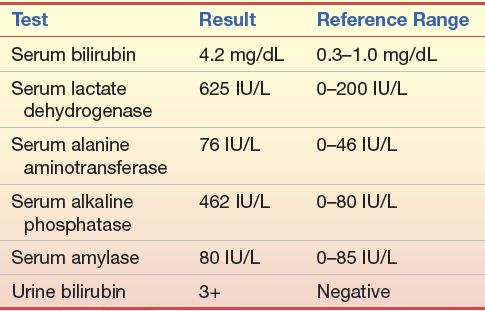
Questions
1. What organ system is primarily involved?
2. What are the major diagnostic considerations?
3. What do the laboratory results mean? What additional laboratory tests would be useful in establishing a diagnosis?
4. What other studies or procedures might be required?
Fecal Fat Analysis
Fecal lipids are derived from four sources: unabsorbed ingested lipids, lipids excreted into the intestine (predominantly in the bile), cells shed into the intestine, and metabolism of intestinal bacteria. Patients on a lipid-free diet still excrete 1 to 4 g of lipid in the feces in a 24-hour period. Even with a lipid-rich diet, the fecal fat does not normally exceed about 7 g in a 24-hour period. Normal fecal lipid is composed of about 60% fatty acids; 30% sterols, higher alcohols, and carotenoids; 10% triglycerides; and small amounts of cholesterol and phospholipids. Although significantly increased fecal fat can be caused by biliary obstruction, severe steatorrhea is usually associated with exocrine pancreatic insufficiency or disease of the small intestine.
Qualitative Screening Test for Fecal Fat
Various screening tests have been devised for detecting steatorrhea. These tests commonly use fat-soluble stains (e.g., Sudan III, Sudan IV, Oil Red O, or Nile blue sulfate), which dissolve in and color lipid droplets. Of greater importance than the particular technical procedure is the level of experience and dependability of the clinical laboratorian performing the test.
Sudan Staining for Fecal Fat
Neutral fats (triglycerides) and many other lipids stain yellow-orange to red with Sudan III because the dye is much more soluble in lipid than in water or ethanol.8,9 Free fatty acids do not stain appreciably unless the specimen is heated in the presence of the stain with 36% acetic acid. The slide may be examined warm or cool and the number of fat droplets assessed. As the slide cools, the fatty acids crystallize out in long, colorless, needle-like sheaves. Detection of meat fiber is accomplished by a third aliquot of fecal sample mixed on the slide with 10% alcohol and a solution of eosin stained for 3 minutes. The meat fiber should stain as rectangular cross-striated fibers. Splitting the sample and detecting neutral fats, fatty acids, and undigested meat fibers can provide diagnostic information. Increases in fats and undigested meat fibers are indicative of patients with steatorrhea of pancreatic origin. A representative fecal specimen is used for analysis.
Normal feces can have up to 40 or 50 small (1 to 5 mm), neutral lipid droplets per high-power microscope field. Steatorrhea is characterized by an increase in the number and size of stainable droplets, often with some fat globules in the 50- to 100-mm range. Fatty acid assessment greater than 100 stained small droplets, along with the presence of meat fiber, is expected in patients with steatorrhea.
Quantitative Fecal Fat Analysis
The definitive test for steatorrhea is the quantitative fecal fat determination, usually on a 72-hour stool collection, although the collection period may be increased to up to 5 days. Traditional methods for fecal fat determination are the gravimetric and titrimetric methods. Newer methods involve the use of infrared and nuclear magnetic resonance spectroscopy.10,11 In the gravimetric method, fatty acid soaps (predominantly calcium and magnesium salts of fatty acids) are converted to free fatty acids, followed by extraction of most of the lipids into an organic solvent, which is then evaporated so that the lipid residue can be weighed. In titrimetric methods, lipids are saponified with hydroxide, and the fatty acid salts are converted to free fatty acids using acid. The free fatty acids, along with various unsaponified lipids, are then extracted with an organic solvent, and the fatty acids are titrated with hydroxide after evaporation of the solvent and redissolving of the residue in ethanol. The titration methods obviously measure only saponifiable fatty acids and, consequently, render results about 20% lower than those from gravimetric methods. A further objection is that titrimetric methods use an assumed average molecular weight for fatty acids to convert moles of fatty acids to grams of lipid.
At one time, it was common to measure the amount of free fatty acids as a percentage of total lipids on the presumption that a high percentage of free fatty acids indicates adequate pancreatic lipase activity. This method is no longer considered reliable because of spurious results, particularly caused by lipase produced by intestinal bacteria.
It is essential that patients be placed on a lipid-rich diet for at least 2 days before instituting the fecal collection. The diet must contain at least 50 g, and preferably 100 g, of lipids each day. Fecal collections should extend for 3 or more successive days.
There are various ways to express fecal lipid excretion. Expressing lipid excretion as a percentage of wet or dry fecal weight is open to serious challenge because of wide variations in both fecal water content and dry residue as a result of dietary intake. The most widely accepted approach is to report the grams of fecal fat excreted in a 24-hour period.
Gravimetric Method for Fecal Fat Determination
The entire fecal specimen is emulsified with water. An aliquot is acidified to convert all fatty acid soaps to free fatty acids, which are then extracted with other soluble lipids into petroleum ether and ethanol. After evaporation of the organic solvents, the lipid residue is weighed. All feces for a 3-day period are collected in tared containers. The containers must not have a wax coating. The specimen must be kept refrigerated.
Total lipid does not change significantly during 5 days’ storage of the specimen at refrigerator temperatures. Patients must not ingest castor oil, mineral oil, or other oily laxatives and must not use rectal suppositories containing oil or lipid for 2 days before the test and during the test.
The reference range for fecal lipids in adults is 1 to 7 g per 24 hours.
Sweat Electrolyte Determinations
Measurement of the sodium and chloride concentration in sweat is the most useful test for the diagnosis of cystic fibrosis.12, 13, 14 Significantly elevated concentrations of both ions occur in more than 99% of affected patients. The twofold to fivefold increases in sweat sodium and chloride are diagnostic of cystic fibrosis in children. Even in adults, no other condition causes increases in sweat chloride and sodium above 80 mmol/L. Sweat potassium is also increased, but less significantly so, and is not generally relied on for diagnosis. Contrary to some assertions, sweat electrolyte determinations do not distinguish heterozygote carriers of cystic fibrosis from normal homozygotes.
Older methods for acquiring sweat specimens required skilled technologists who frequently performed the test. Induction of sweat included applying plastic bags or wrapping the patient in blankets, which was fraught with serious risks of dehydration, electrolyte disturbances, and hyperpyrexia. In 1959, pilocarpine administration by iontophoresis was reported as an efficient method for sweat collection and stimulation. Iontophoresis uses an electric current that causes pilocarpine to migrate into a limited skin area, usually the inside of the forearm, toward the negative electrode from a moistened pad on the positive electrode. A collection vessel is then applied to the skin. The sweat is then analyzed for chloride. For confirmation, the test should be repeated. Commercially available surface electrodes that analyze the sweat chloride are readily available. For details, the reader is referred to Chapter 29.
It is widely accepted that sweat chloride concentrations greater than 60 mmol/L are diagnostic of cystic fibrosis in children. Sweat sodium and chloride concentrations in female patients undergo fluctuation with the menstrual cycle and reach a peak 5 to 10 days before the onset of menstruation but do not overlap with the ranges associated with cystic fibrosis.
Serum Enzymes
Amylase is the serum enzyme most commonly relied on for detecting pancreatic disease.15,16 It is not, however, a function test. Amylase is particularly useful in the diagnosis of acute pancreatitis, in which significant increases in serum concentrations occur in about 75% of patients. Typically, amylase in serum increases within a few hours of the onset of the disease, reaches a peak in about 24 hours, and because of its clearance by the kidneys returns to normal within 3 to 5 days, often making urine amylase a more sensitive indicator of acute pancreatitis. The magnitude of the enzyme elevation cannot be correlated with the severity of the disease.
CASE STUDY 28.3
Parents brought their 7-year-old son to the pediatrician with the complaint of frequent fevers and failure to grow. The child had three bouts of pneumonia during the past 2 years and was bothered by chronic bronchitis, which caused him to cough up copious amounts of thick, yellow, mucoid sputum. Despite a big appetite, he had gained only 1 to 2 lb in the past 2 years and was of short, frail stature. He especially liked salty foods. He usually had three or four bulky, foul-smelling bowel movements daily. A 9-year-old sister was in excellent health.
questions
1. What is the most likely disease?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


