Paget Disease of the Nipple
ELENA BRACHTEL
FREDERICK C. KOERNER
In 1874, Sir James Paget1 described “an eruption on the nipple and areola” with characteristics of “ordinary chronic eczema” or “psoriasis.” He observed that “cancer of the mammary gland has followed within at the most two years” and that “the formation of cancer has not in any case taken place first in the diseased part of the skin. It has always been in the substance of the mammary gland.” The carcinomas that occurred in these patients followed the clinical course of other cases without Paget disease and showed “nothing which might not be written in the ordinary history of cancer of the breast.”
Paget did not describe the histopathology of this condition. However, he inferred from his clinical observations that “a superficial disease induces in the structures beneath it, in the course of many months, such degeneracy as makes them apt to become the seats of cancer.” To support this conclusion, he referred to the development of carcinoma of the penis, tongue, and lip after “chronic soreness or irritation.”
The existence of extramammary Paget disease was recognized before the end of the 19th century, by which time the characteristic histologic features of the disease had been reported.2,3 Thin3 studied a series of specimens in the pathologic museum of the British Medical Association and concluded that “this malignant dermatitis has neither the symptoms nor the pathologic anatomy of any known skin disease.” He described the histopathologic features of breast carcinoma in Paget disease and illustrated the “blocking up of the lactiferous ducts in the affection by newly formed cancerous epithelium [which] may break through the wall of the duct into the connective tissue of the nipple.” Thin interpreted his observations as indicating that secretions emerging from the mammary ducts injured the epidermis and that this process induced the underlying carcinoma. Although histologic, electron microscopic, and immunohistochemical data have been put forward to support the view that Paget disease is a neoplasm derived from altered epidermal keratinocytes,4,5 this mechanism is no longer considered to be the histogenesis of the condition.
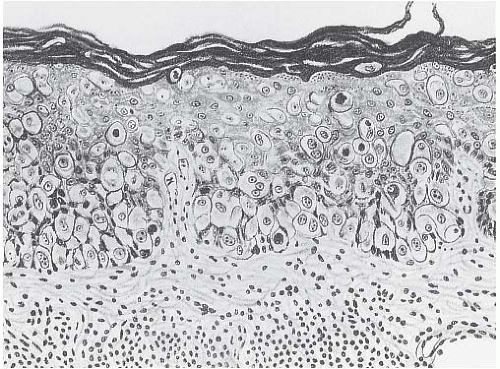
The concept that Paget disease represents the spread of carcinoma cells into the epidermis from an underlying mammary adenocarcinoma was first advanced in 1904 by Jacobaeus6 on the basis of a histologic study of three cases (Fig. 30.1). He concluded that “Paget disease is a carcinoma from its inception, derived from the glandular epithelium of the lactiferous ducts.” He also noted that extension through the duct system provided a mechanism for the development of Paget disease in association with a carcinoma located deep within the breast. These observations were confirmed in 1927 by Muir,7 who also described the phenomenon of “secondary” Paget disease, which occurs when an invasive primary carcinoma of the breast extending directly into the epidermis is accompanied by the intraepidermal spread of Paget cells. Secondary Paget disease has also been described in the skin at sites of adenocarcinoma metastatic from the breast.8
Considerable data from anatomic, histopathologic, and molecular studies support the evidence that Paget cells are derived from an underlying adenocarcinoma. In particular, the distribution of carcinoembryogenic antigen (CEA),9,10,11 casein,12 milk-fat globule membrane antigens,13,14 gross cystic disease fluid protein 15 (GCDFP-15),15 MUC proteins,16,17 cytokeratins (CKs),18,19,20 estrogen receptor (ER),21 and human epidermal growth factor 2 (HER2)22 indicates a glandular origin.
CLINICAL PRESENTATION
Frequency
Paget disease is an uncommon manifestation of mammary carcinoma that affects 1% to 3% of patients with breast carcinoma.23 The majority of these women have a clinically evident nipple lesion. Ten percent to 28% of cases of Paget disease are detected only in histologic sections of the nipple removed at mastectomy, having caused no clinical abnormality. After reviewing incidence data recorded by nine registries in the Surveillance Epidemiology and End Results (SEER) program, Chen et al.23 reported a 45% decline in the incidence of reported Paget disease between 1988 (age-adjusted incidence/100,000, 1.31) and 2002 (age-adjusted incidence/100,000, 0.64). The decline in incidence was limited to patients who had documented DCIS or invasive duct carcinoma (IDC). The incidence of Paget disease without associated clinical ductal carcinoma remained stable during this period. As a consequence, the relative portion of Paget disease without associated clinical ductal carcinoma increased from 12% to 15%. The authors did not discriminate between clinically apparent Paget disease and occult Paget disease discovered in routine sections of the nipple from mastectomy specimens. It is likely that the shift to breastconserving surgery during this period contributed to the apparent decline in the incidence of Paget disease because fewer nipple samples were available for histologic examination. The fact that the incidence of Paget disease without underlying carcinoma, which is only detectable clinically, remained stable during this interval appears to support this interpretation.
Age
The age range of patients with Paget disease in several large series consisting cumulatively of 508 patients was 26 to 88 years,18,24,25,26 and the average age at diagnosis in one series of 1,738 women was 62.5 years.23 In this group, the mean age for women with Paget disease and IDC was 63.8 years, for women with Paget disease and ductal carcinoma in situ (DCIS) 66.2 years, and for women with Paget disease without underlying carcinoma 66.2 years.23 Paget disease arose in the ectopic nipple of a 13-year-old girl27 and in the nipple of a 90-year-old woman.28
Male Breast
One might expect Paget disease to occur more frequently in men than in women because almost all carcinomas of the male breast involve the subareolar region,29 but fewer than 1% of reported cases of Paget disease have been found in men.30 It occurred in 2.8% of 229 patients in one series of men with breast carcinoma.31 About one-half of the early reports of Paget disease of the male breast lack histologic confirmation, so the literature contains fewer than 50 bona fide cases of Paget disease in men. Desai et al.32 tabulated details of 33 convincing cases described before 1996, and several well-documented case descriptions have been published since.33,34,35,36,37,38,39,40,41,42,43,44,45,46 In the series by Goss et al.,31 men with Paget disease spanned 23 to 97 years in age, essentially the range seen in women with the disease.
Laterality
Risk Factors
Researchers have not identified factors that specifically predispose to the development of Paget disease, but a few reports mention factors that generally predispose patients to the development of breast carcinomas. Loizou et al.56 described a 36-year-old woman who underwent “extensive cardiac fluoroscopy” at birth and again at the age of 7 years who developed Paget disease at the age of 36 years. Paget disease has been found associated with breast carcinoma developing in men with Klinefelter syndrome.53,57
Unusual Presentation
Several cases of Paget disease have presented in unusual clinical settings. Kawawa et al.58 detailed the case of a 66-year-old woman with Paget disease and neurofibromatosis, and Holloway et al.38 described a similar case in a man. Fouad59 reported a case of a man with Paget disease and lymphomatoid papulosis. A 35-year-old woman who had systemic scleroderma involving the skin of the breast with coexistent Paget disease has been described.60 Kao et al.61 observed DCIS and Paget disease in ectopic breast tissue on the chest of a 58-year-old woman, and two reports document Paget disease in accessory nipples.27,62 Two women developed Paget disease confined to the areola.63,64 Mendez-Fernandez et al.65 detected Paget disease in the nipple of a woman 8 years after subcutaneous mastectomy for fibrocystic disease. Two cases of axillary Paget disease associated with mammary carcinoma have been described.66,67
Recurrent Carcinoma as Paget Disease
Recurrences of conventional breast carcinomas sometimes take the form of Paget disease. It developed in the nipple of a woman treated with excision alone68 and those of 15 women treated with breast-conserving excision and irradiation,69,70,71,72,73,74,75,76 3 women treated with subcutaneous mastectomy,771 woman treated with an areola-sparing mastectomy,78 and 7 women treated with a nipple-sparing mastectomy.79 Basu et al.80 reported an especially unusual case of a 64-year-old woman who underwent a left mastectomy and subsequent transverse rectus abdominus muscle (TRAM) flap reconstruction for carcinoma. During that procedure, the left nipple was reconstructed by means of the nipple-sharing technique using tissue from the right nipple. Six years later, Paget disease developed in the right nipple, and 7 years after that it arose in the reconstructed left nipple.
Symptoms and Clinical Appearance
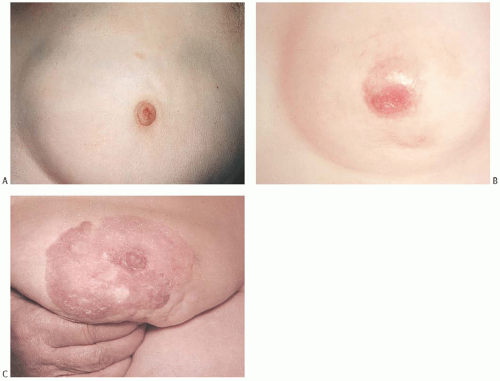
Pain and itching are frequent complaints. Physical examination typically reveals a thickened, erythematous, scaling papule or plaque with irregular borders involving the nipple. The changes may be limited to the nipple or extend to the areola, and in advanced cases the lesion also involves the skin surrounding the areola (Fig. 30.2). Haagensen81 wrote that “erosions that involve the areola or the skin of the adjacent breast leaving the nipple uninvolved are not Paget disease”; however, examples confined to the areola have been described.63,64 Advanced cases often demonstrate ulceration, crusting, serous or bloody discharge from the nipple, and nipple retraction or inversion.82 In one exceptional case, the alterations extended to the skin of the abdomen,83 and in another, they involved the skin of the back and the proximal one-third of the arm.84
Because of the nonspecific nature of the clinical signs of Paget disease, a delay of 6 to 12 months prior to biopsy during which the symptoms are treated topically is not uncommon. In the series of Ascensão et al.,85 the symptomatic intervals from 1 week to 20 years were recorded, and the average period of delay was 2.25 years.
Lesions that Mimic Paget Disease
The findings in Paget disease can be mistaken for eczema86 or other inflammatory conditions such as seborrheic dermatitis, contact dermatitis, postirradiation dermatitis, psoriasis, and pagetoid dyskeratosis.87 Pennell et al.88 reported a case of cutaneous para-areolar schistosomiasis that mimicked Paget disease. Minute vesicles sometimes erupt and seem to heal, and this phenomenon may bring to mind the presence of a bullous disease such as pemphigus. Guyton et al.89 described a case of pemphigus vulgaris initially thought to represent Paget disease and cited other examples of confusion of these two entities.90,91 Rae et al.92 described a 63-year-old woman in whom both pemphigus vulgaris and Paget disease involved the right nipple. Neoplastic lesions clinically confused with Paget disease include adult Langerhans cell histiocytosis,93 intraepidermal squamous carcinoma (Bowen disease), and unusual examples of basal cell carcinoma94 and melanoma.95
Pigmented Paget Disease
In an uncommon variant of Paget disease known as pigmented Paget disease, accumulation of melanin imparts
a brown color to the affected region. The publication by Soler et al.96 lists details of 17 published cases, and other reports describe 7 additional examples.39,42,45,97,98,99,100 One notes that a disproportionately high number of cases occurred in men.37,39,42,44,45,46,101 For additional information regarding pigmented Paget disease, see Chapter 42.
a brown color to the affected region. The publication by Soler et al.96 lists details of 17 published cases, and other reports describe 7 additional examples.39,42,45,97,98,99,100 One notes that a disproportionately high number of cases occurred in men.37,39,42,44,45,46,101 For additional information regarding pigmented Paget disease, see Chapter 42.
Palpable Breast Tumor
Fifty percent to 60% of patients have a palpable tumor in the breast that exhibits Paget disease. In one study, the mean age of women with a tumor (49 years) was significantly less than that of women without a tumor (58 years).25 An invasive carcinoma was detected in more than 75% to 90% of women who had Paget disease accompanied by a tumor,18,24,102 and 45% to 66% of them reportedly had axillary lymph node (ALN) metastases.18,24,25,102 In the absence of a clinically apparent tumor, invasive carcinoma occurs in no more than 40% of cases, and axillary metastases have been reported in 5% to 13% of cases.18,24,25,102
Imaging Studies
A number of mammographic abnormalities may be found in the breast underlying Paget disease.103,104 Lesions anywhere in the breast may be indicative of a separate distant coexistent carcinoma. In the nipple-subareolar region, the significant findings include thickening of the nipple, an underlying mass, possibly with nipple retraction, and calcifications. Patients with clinically apparent Paget disease tend to have radiologic findings in the nipple-subareolar region. When Paget disease is not evident clinically, mammography more often discloses lesions away from the nipple region. Such abnormalities include a suspicious mass, asymmetry, architectural distortion, and suspicious calcifications. These observations notwithstanding, mammography is not a reliable procedure for either detecting Paget disease or determining its extent. In 22%105 to 50%103 of patients with Paget disease, the mammograms appeared normal and they underestimated the extent of disease in nearly one-half of the patients.103,105,106,107,108 In a study of 25 breasts that proved to have Paget disease on pathologic examination, only three cases (12%) had nipple abnormalities on mammography.109 Fourteen patients with clinical evidence of Paget disease in this series had underlying carcinomas. Among these 14 patients, mammography identified the underlying tumor in 6 (43%). Ultrasonography can sometimes reveal calcifications, dilatation of ducts, or flattening, asymmetry, or thickening of the nipple-areolar complex. The frequency of detection of abnormalities is similar to that of mammography.106,110 Magnetic resonance imaging (MRI) of patients with Paget disease can disclose abnormal nipple enhancement, thickening and enhancement of the nipple-areolar complex, and coexisting enhancing DCIS or suspicious masses.111,112 In both individual case reports113,114,115 and small series,112,116 this modality improved the detection of associated carcinomas in patients with clinical signs of Paget disease and negative mammography and ultrasonography.
GROSS PATHOLOGY
The macroscopic pathologic changes of Paget disease on the surface of the resected nipple are those observed clinically. Occasionally, enlarged lactiferous ducts can be detected if the nipple and underlying breast are examined carefully.
Most studies of Paget disease give little information about the distribution of underlying carcinoma in the breast. It can usually be found in at least one lactiferous duct. An invasive tumor, if present, tends to be central, but instances of peripherally placed tumors have been recorded.117 Chaudary et al.18 reported that 45% of palpable invasive carcinomas associated with Paget disease in their series were located in the upper outer quadrant. Clinically palpable tumors have no specific gross pathologic features. A small percentage of women who present with Paget disease and have no tumor detected on clinical examination are found to have a grossly evident invasive carcinoma in the resected breast.24,117
MICROSCOPIC PATHOLOGY
Biopsy Diagnosis
The diagnosis of Paget disease can be made from specimens obtained by a wedge biopsy, a superficial “shave” biopsy of epidermis, or punch biopsy. The wedge biopsy is most likely to yield a diagnostic specimen because the epidermis is adequately represented, and this type of specimen is likely to include a section of lactiferous duct. The shave biopsy is less likely to contain a sufficient number of Paget cells, because these specimens sometimes consist largely of superficial keratinized debris or inflammatory exudate. Although a punch biopsy will include the underlying stroma and possibly part of a duct, there is frequently very little epidermis to study. However, none of these procedures is always successful, and it is sometimes necessary to perform a second biopsy or to excise the nipple. The detection of Paget cells in the epidermis in a biopsy sample that appears to contain a florid papillomatosis is indicative of an associated carcinoma, even if the portion of the underlying lesion seen in the biopsy specimen appears benign.118
Paget Cells
The characteristic histopathologic feature of this condition is the presence of adenocarcinoma cells (Paget cells) in the keratinizing epithelium of the nipple epidermis (Fig. 30.3). These cells occur singly in superficial epidermal layers. In rare instances, they extend into eccrine ducts36 and hair follicles.119 Paget cells are more likely to form clusters in the basal portions of the epidermis and to have a distribution similar to that of junctional melanocytes. The resemblance
to melanoma is enhanced if the carcinoma cells take up melanin pigment released by epidermal cells.120,121 Isolated Paget cells appear to lie in vacuoles within the epidermis. The cytoplasm is usually pale or clear, and it may contain mucin secretion vacuoles. Nuclei of Paget cells tend to have prominent nucleoli. Rarely, Paget disease forms glands within the epidermis of the nipple122,123 (Fig. 30.3F).
to melanoma is enhanced if the carcinoma cells take up melanin pigment released by epidermal cells.120,121 Isolated Paget cells appear to lie in vacuoles within the epidermis. The cytoplasm is usually pale or clear, and it may contain mucin secretion vacuoles. Nuclei of Paget cells tend to have prominent nucleoli. Rarely, Paget disease forms glands within the epidermis of the nipple122,123 (Fig. 30.3F).
Other microscopic aspects of Paget disease sometimes obscure the lesion, and they may interfere with the diagnosis. Hyperplasia and hyperkeratosis of the epidermis occur to some degree, and they are occasionally severe enough to suggest pseudoepitheliomatous hyperplasia (Fig. 30.4). The superficial, dermal stroma of the nipple is usually infiltrated by a moderate-to-marked lymphocytic reaction. When ulceration denudes the affected epithelium, a biopsy of the exposed stroma will reveal only the underlying inflammatory reaction. Unless this misleading appearance is recognized, the biopsy findings may reinforce
an erroneous clinical diagnosis of an inflammatory condition. It is, therefore, important to state in the pathologic report whether epidermal tissue is present. Absence of epidermis is an indication for rebiopsy when Paget disease is suspected clinically.
an erroneous clinical diagnosis of an inflammatory condition. It is, therefore, important to state in the pathologic report whether epidermal tissue is present. Absence of epidermis is an indication for rebiopsy when Paget disease is suspected clinically.
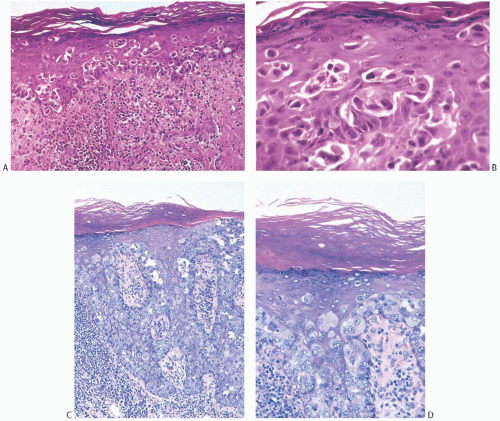 FIG. 30.3. Paget disease. A: Carcinoma cells form a band in the deep epidermis, and they are scattered individually throughout the squamous epithelium. B: A lacunar arrangement of carcinoma cells is commonly seen in Paget disease. C: A very extensive infiltrate with involvement largely concentrated in the deep epidermis. Lacunae are not conspicuous in this instance. D
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|