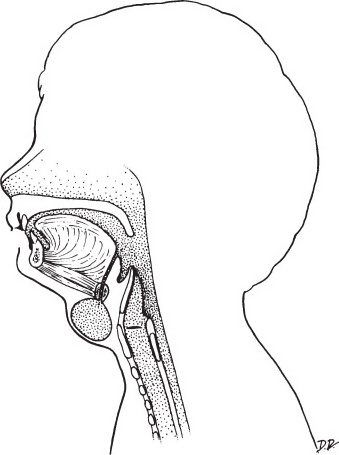
Anatomic location of branchial cleft remnants and external openings. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, et al., eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Branchial Cleft
•A series of four arches that form in the neck early in development (4 to 6 weeks)
•Cysts are trapped remnants of clefts or pouches
•Sinuses open into the pharynx internally or the skin externally
•Fistulae have both internal and external openings
•Diagnosis: Clinical; can get CT or MRI for confirmation
•Treatment: Complete resection of the cyst and tract
•First branchial cleft
•Duplication of the external auditory canal
•Can communicate to the oral cavity below the angle of the mandible
•Care must be taken to avoid injuring the facial nerve during resection
•Second branchial cleft
•Most common (90%) of branchial cleft anomalies
•External opening along the anterior border of SCM and internal opening at the tonsillar fossa
•Courses between carotid vessels and over hypoglossal and glossopharyngeal nerves
•Third branchial cleft
•External opening along the anterior border of SCM and internal opening at the piriform sinus
•Courses behind carotid vessels and below the hypoglossal nerve, above the glossopharyngeal nerve
A second branchial cleft anomaly is the most common type.
An otherwise healthy child presents with a midline neck mass below the hyoid bone that is nontender. The mass moves with swallowing. What is the most likely diagnosis?
Thyroglossal duct cysts are common congenital and developmental neck masses. The differential includes thyroglossal duct cyst, dermoid cyst, teratoma, branchial cleft cyst, laryngocele, lymphangioma, and hemangioma.
Thyroglossal duct cyst. (With permission from Fischer JE, Bland KI, Callery MP, et al., eds. Mastery of Surgery. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
Thyroglossal Duct Cyst
•The thyroid gland is formed at the base of the tongue and migrates through the tongue to its position in the neck
•Failure of the tract to obliterate following descent leads to a thyroglossal duct cyst
•Can occur anywhere along the path of descent
•80% are midline, and 80% are at or below the level of the hyoid bone
•A third of patients present before age 10 and about one-third of patients present after age 30
•Typically asymptomatic
•Move with swallowing and protrusion of the tongue
•Can become superinfected with upper respiratory tract infections and become tender and rapidly enlarge
•Evaluation should include imaging (CT or ultrasound) to differentiate from a thyroid mass
•An incision and drainage alone is inadequate
•Treatment is complete surgical excision of the cyst and tract to the foramen cecum at the base of the tongue and removal of the central portion of the hyoid bone (Sistrunk procedure)
•Recurrence is <10% after complete excision
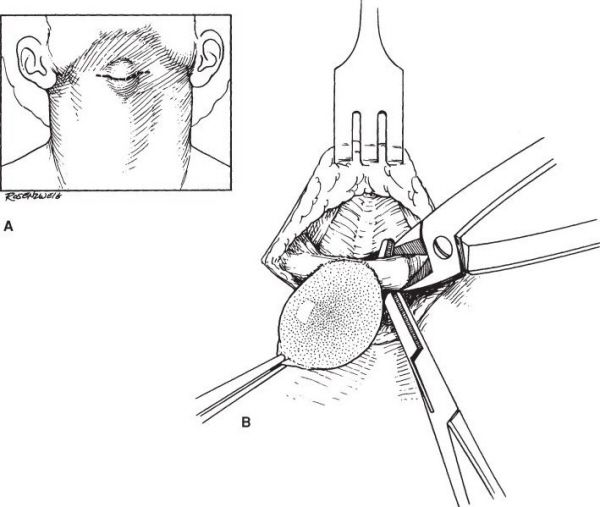
Sistrunk procedure. (With permission from Fischer JE, Bland KI, Callery MP, et al., eds. Mastery of Surgery. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
A 1-year-old girl presents with a soft lateral neck mass that transilluminates. What is the best test to confirm the diagnosis?
History and physical examination is essential to establish the diagnosis—lymphangioma. Transillumination of the mass is characteristic.
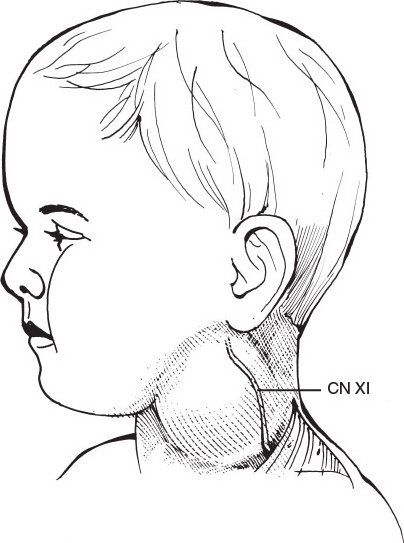
Cystic hygroma. (With permission from Fischer JE, Bland KI, Callery MP, et al., eds. Mastery of Surgery. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.)
Lymphangioma
•Developmental malformation of the lymphatics
•Divided into three categories: Simple, cavernous, and cystic hygroma
•90% present by age 2
•Most commonly found in the neck
•Soft, painless, ill-defined mass
•If large, can cause dysphagia or respiratory symptoms
•Slowly enlarges with time
•Treatment is surgical excision
•Recurrence rate is 10%
A 1-year-old girl presents with a soft lateral neck mass that is bluish in hue. What is the best test to confirm the diagnosis?
A history and physical examination establishes the diagnosis of a hemangioma. Imaging studies will demonstrate the vascular nature (CT with contrast) and feeding vessels (MRA or angiography).
Hemangioma
•Vascular malformations can be defined as capillary, cavernous, mixed, juvenile, or proliferative
•95% present by age 6 months
•Tend to be poorly defined, soft, compressible, cystic masses
•May have a bruit
•Initially have a period of growth followed by involution over the next 5 years
•Steroids have been shown to help arrest growth and promote resolution
•Surgical excision (possibly with embolization) is used for rare lesions that fail to resolve or for lesions that cause symptoms (CHF and Kasabach-Merritt syndrome)
One week after a total knee replacement, a 70-year-old man presents with painful, erythematous swelling over his left lower face. What is the most likely diagnosis?
Acute parotitis usually presents with fever, leukocytosis, swelling, tenderness, and foul discharge intraorally. Sialoadenitis refers to infection in one of the three, paired major salivary glands.
Sialoadenitis
•Causes of acute sialoadenitis
•Obstruction—sialolithiasis
•Dehydration—especially in the elderly and postoperative patients
•The most common causative organism is Staphylococcus aureus
•Treatment is hydration, sialogogues, antibiotics, warm compresses, and gentle massage of the affected gland
•Salivary gland stones (sialoliths) can cause obstruction leading to recurrent sialoadenitis
•Eventually, the affected gland will burn out and scar down
•Stones in the parotid (Stensen) or submandibular (Wharton) duct can be extracted transorally
•Stones deeper in the gland may necessitate removal of the gland
•A parotid abscess is treated by incision and drainage—take care to incise the parotid along the course of the branches of the facial nerve
A 42-year-old woman with dental caries presents with new onset fever, neck swelling, pain, dysphagia, and a firm floor of the mouth. What is the most likely diagnosis?
Ludwig angina is a severe infection of the floor of the mouth in the submandibular and submental spaces. Spread of infection occurs along fascial planes.
Ludwig Angina
•Infection typically of dental origin
•Spreads around the mylohyoid muscle into the submandibular space
•Infection past the mylohyoid progresses rapidly
•Presents with swelling and displacement of the tongue superiorly and posteriorly, trismus, odynophagia, woody induration of the neck, as well as induration of the floor of the mouth
•Usually not a discrete abscess (absence of frank pus)
•Treatment is with IV antibiotics, tracheostomy (occasionally), and wide drainage
•Complications include loss of airway, septic emboli, septic shock, and aspiration
•The “danger space” is located between the prevertebral and alar divisions of the cervical fascia because of the easy spread of infection from this location to the mediastinum
A 22-year-old man arrives to the emergency department with a Glasgow coma scale (GCS) of 15, pulse of 110, blood pressure of 120/60, and a stab wound to the lateral neck above the level of the mandible. What is the next step in management?
Angiography should be performed for a Zone 3 injury that lacks indications for immediate neck exploration.
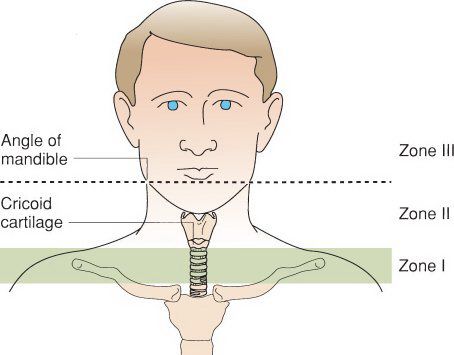
Zones of the neck. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, et al., eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Neck Zones
•Zone 1: Manubrium to cricoid cartilage
•Most lethal when carotid is injured
•Esophageal injuries can lead to mediastinitis
•Zone 2: Cricoid cartilage to angle of mandible
•Most frequently injured
•Zone 3: Angle of mandible to skull base
•Least frequently injured
•Carotid artery is injured in 6% of cases
•Indications for a neck exploration in trauma patients
•Severe, active bleeding
•Expanding hematoma
•Progressing neurologic deficit
•Loss of pulse
•Hemoptysis/hematemesis
•Subcutaneous emphysema, dyspnea, or stridor
There is some controversy about how to best manage penetrating neck trauma. Zone 1 and Zone 3 injuries are usually evaluated with arteriography to assess for occult vascular injury. Stable Zone 2 injuries are the easiest to follow with clinical examinations. Examination should include fiberoptic laryngoscopy.
A 23-year-old presents with epistaxis after being inadvertently elbowed during a basketball game. What is the appropriate treatment?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


