DRUG CLASSES
Otic preparations
Ophthalmic
Preparations
PHARMACOLOGY IN PRACTICE

Janna Wong, a 16-year-old high school student, recently switched from eyeglasses to contact lenses. She is experiencing minor eye irritation. In this chapter learn how to teach Janna the correct way to use her eye drops.
This chapter provides information on drugs that are topically applied to the eyes and ears. Because the eyes and ears help us to interpret our environment, any disease or injury that has the potential for partial or total loss of function of these organs should be treated.
OTIC PREPARATIONS
The term “otic” means auditory in Latin. It is important to remember the connection between the words “otic” and “ear,” because harm can be done when these preparations are swallowed or administered into the eye.
Disorders of the ear are categorized according to the part of the ear affected: the outer, the middle, or the inner ear (Fig. 53.1). The disorders of the outer and middle ear are discussed in this chapter. Otitis media, by far the most common disorder of the middle ear, is fluid in the middle ear accompanied by symptoms of intense local or systemic infection. Symptoms include pain in the ear, drainage of fluid from the ear canal, and hearing loss. Other symptoms that may be present if the disorder becomes systemic include fever, irritability, headache, and anorexia. The most common causes are viruses and bacteria.
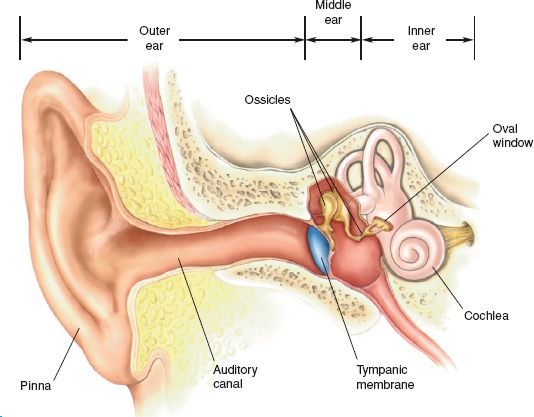
Figure 53.1 The outer, middle, and inner ear. (From Bear, M. F., Connors, B. W., & Parasido, M. A. [2001]. Neuroscience—Exploring the Brain [2nd ed.]. Philadelphia: Lippincott Williams & Wilkins.)
Actions
Otic preparations can be divided into three categories: (1) antibiotics, (2) antibiotic/steroid combinations, and (3) miscellaneous preparations. The miscellaneous preparations usually contain one or more of the following ingredients:
• Benzocaine—a local anesthetic used to temporally relieve pain
• Phenylephrine—a vasoconstrictor decongestant
• Hydrocortisone—corticosteroid for anti-inflammatory and antipruritic effects
• Glycerin—an emollient and a solvent
• Antipyrine—an analgesic
• Acetic acid, boric acid, benzalkonium, aluminum, benzethonium—provide antifungal or antibacterial action
• Carbamide peroxide—aids in removing cerumen (yellowish or brownish ear wax) by softening and breaking up the wax
Examples of otic preparations are given in the Summary Drug Table: Selected Otic Preparations.
Uses
Otic preparations are instilled in the external auditory canal and may be used to:
• Relieve pain
• Treat infection and inflammation
• Aid in the removal of cerumen
When the patient has an inner ear infection, systemic antibiotic therapy is indicated.
Adverse Reactions
When otic drugs are applied topically, the amount of drug that enters the systemic circulation usually is not sufficient to produce adverse reactions. Local adverse reactions that may occur include:
• Ear irritation
• Itching
• Burning
Prolonged use of otic preparations containing an antibiotic, such as ofloxacin, may result in a superinfection (an overgrowth of bacterial or fungal microorganisms not affected by the antibiotic being administered).
Contraindications, Precautions, and Interactions
These drugs are contraindicated in patients with a known hypersensitivity to the drugs. The otic drugs are used with caution during pregnancy and lactation. The pregnancy category of most of these drugs is unknown when they are used as otic drugs. Drugs to remove cerumen are not used if ear drainage, discharge, pain, or irritation is present; if the eardrum is perforated; or after ear surgery. Otic drugs may be available in dropper bottles and can be dangerous if ingested. Therefore, these drugs are stored safely out of the reach of children and pets.
If an allergy is suspected, the drug is not administered. Ofloxacin is a pregnancy category C drug and should be administered in pregnancy only if the potential benefit justifies the risk to the fetus. No significant interactions have been reported with use of the otic preparations.
NURSING PROCESS
PATIENT TEACHING FOR MEDICATION INFORMATION
ASSESSMENT
Preadministration Assessment
When a patient is seen in the clinic setting, you may be responsible for examining the outer structures of the ear (i.e., the earlobe and the skin around the ear) as part of the intake procedure. Be sure to document a description of any drainage or visible wax. Before prescribing an otic preparation, the primary health care provider examines the ear’s external and internal structures. Perforated eardrums may be a contraindication to some of the otic preparations. Check with the primary health care provider before administering an otic preparation to a patient with a perforated eardrum.
Ongoing Assessment
Assess the patient’s response to therapy. For example, a decrease in pain or inflammation should occur. Examine and palpate the outer ear and ear canal for any local redness or irritation that may indicate sensitivity to the drug.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Pediatric
When assessing the infant, look for pulling, grabbing, or tugging at his or her ears. Because infants cannot tell you about pain, this may be a sign that the child’s ear hurts. Since infants do pull their ears for all kinds of reasons or for no reason at all, validate this behavior with the parent or caregiver. Additional signs include a change in behavior, crying, fussiness or irritability, or a fever.
Drug-specific nursing diagnoses include the following:
 Risk for Infection (superinfection) related to prolonged use of the anti-infective otic drug
Risk for Infection (superinfection) related to prolonged use of the anti-infective otic drug
 Anxiety related to ear pain or discomfort, changes in hearing, diagnosis, or other factors
Anxiety related to ear pain or discomfort, changes in hearing, diagnosis, or other factors
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected outcomes of the patient depend on the reason for administering the drug and may include an optimal response to the drug, support of patient needs related to the management of adverse reactions, a reduction in anxiety, and confidence in an understanding of the application and use of an otic preparation.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
Ear disorders may result in symptoms such as pain, a feeling of fullness in the ear, tinnitus, dizziness, or a change in hearing. Some of these same sensations may be felt by the patient from the solutions used for treatment. Before instilling an otic solution, tell the patient that a feeling of fullness may be felt in the ear and that hearing in the treated ear may be impaired while the solution remains in the ear canal.
Before instillation of otic preparations, hold the container in your hand for a few minutes to warm it to body temperature. Cold and too warm (above body temperature) preparations may cause dizziness or other sensations after being instilled into the ear.
 NURSING ALERT
NURSING ALERT
Only preparations labeled as “otic” are instilled in the ear. Check the label of the preparation carefully for the name of the drug and a statement indicating that the preparation is for otic use.
To keep solutions in the ear when instilling ear drops, have the patient lie on his or her side with the affected ear up toward the ceiling. If the patient wishes to remain in an upright position, the head is tilted toward the untreated side with the ear toward the ceiling (Fig. 53.2). When administering an otic drug, the ear canal should be straightened. To straighten the ear canal in the adult and children age 3 years and older, the cartilaginous portion of the outer ear is gently pulled up and back. Be particularly gentle, because some conditions make the ear canal very sensitive. Drop the solution into the ear canal; never insert the dropper or applicator tip into the ear canal (Fig. 53.2).
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Pediatric
In children younger than 3 years of age, the ear canal is straighter and needs less manipulation. Gently pull the outer ear down (instead of up) and back.
The patient is kept lying on the untreated side after the medication is instilled for approximately 5 minutes to facilitate the penetration of the drops into the ear canal. If medication is needed in the other ear, it is best to wait at least 5 minutes after instillation of the first ear drops before administering drops to the other ear. Once the patient is upright, the solution running out of the ear may be gently removed with gauze. A piece of cotton can be loosely inserted into the ear canal to prevent the medication from flowing out. The cotton is not inserted too deeply, because it may cause increased pressure within the ear canal.

Figure 53.2 Instilling ear drops. With the head turned toward the unaffected side, pull the cartilaginous portion of the outer ear (pinna) up and back in the adult and instill the prescribed number of drops on the side of the auditory canal.
Cerumen is a natural product of the ear and is produced by modified sweat glands in the auditory canal. Sometimes too much cerumen is produced, particularly in older adults. Drugs that loosen cerumen, such as Cerumenex, work by softening the dried ear wax inside the ear canal. Cerumenex is available by prescription and is not allowed to stay in the ear canal more than 30 minutes before irrigation. When Cerumenex is administered, the ear canal is filled with the solution and a cotton plug is inserted. The drug is allowed to remain in the ear for 15 to 30 minutes, and then the ear is flushed with warm water using a soft rubber bulb ear syringe.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Cerumen is thicker in the older adult, making the accumulation of excess wax more likely. When hearing loss is suspected in the older adult, mentally impaired, or debilitated patient, the ear should be checked for excess cerumen.
Monitoring and Managing Patient Needs
RISK FOR INFECTION. When using the otic antibiotics there is a danger of a superinfection, or another infection on top of the original one, from prolonged use of the drug (see Chapter 9 for a discussion of superinfection). If after administering the drops as directed for 1 week the infection does not improve, the primary health care provider should be notified.
ANXIETY. Patients with an ear disorder or injury usually have great concern over the effect the problem will have on their hearing. Reassure the patient that every effort is being made to treat the disorder and relieve the symptoms.
Educating the Patient and Family
Provide the patient or a family member written instructions or a demonstration of the instillation technique of an otic preparation.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Pediatric
Because some children are prone to recurrent attacks of acute otitis media, parents should be taught to identify early signs and symptoms of otitis media and seek medical attention when their child exhibits these symptoms.
The following information may be given to the patient when an ear ointment or solution is prescribed:
 Wash the hands thoroughly before cleansing the area around the ear (when necessary) and instilling ear drops or ointment.
Wash the hands thoroughly before cleansing the area around the ear (when necessary) and instilling ear drops or ointment.
 If the solution is cool or cold, warm to room temperature by holding solution in the hand for 1 to 2 minutes before administering.
If the solution is cool or cold, warm to room temperature by holding solution in the hand for 1 to 2 minutes before administering.
 Instill the prescribed number of drops in the ear. Do not put the applicator or dropper tip in the ear or allow the tip to become contaminated from the fingers or other sources.
Instill the prescribed number of drops in the ear. Do not put the applicator or dropper tip in the ear or allow the tip to become contaminated from the fingers or other sources.
 Immediately after use, replace the cap or dropper and refrigerate the solution if so stated on the label.
Immediately after use, replace the cap or dropper and refrigerate the solution if so stated on the label.
 If the drops are in a suspension form, shake the container well for 10 seconds before using.
If the drops are in a suspension form, shake the container well for 10 seconds before using.
 Keep the head tilted or lie on the untreated side for approximately 5 minutes to allow the solution to remain in contact with the ear. Excess solution and solution running out of the ear can be wiped off with a tissue.
Keep the head tilted or lie on the untreated side for approximately 5 minutes to allow the solution to remain in contact with the ear. Excess solution and solution running out of the ear can be wiped off with a tissue.
 Do not insert anything into the ear canal before or after applying the prescribed drug unless advised to do so by the primary health care provider. At times a soft cotton plug may be inserted into the affected ear.
Do not insert anything into the ear canal before or after applying the prescribed drug unless advised to do so by the primary health care provider. At times a soft cotton plug may be inserted into the affected ear.
 Complete a full course of treatment with the prescribed drug to achieve satisfactory results.
Complete a full course of treatment with the prescribed drug to achieve satisfactory results.
 Do not use nonprescription ear products during or after treatment unless such use has been approved by the primary health care provider.
Do not use nonprescription ear products during or after treatment unless such use has been approved by the primary health care provider.
 Remember that temporary changes in hearing or a feeling of fullness in the ear may occur for a short time after the drug has been instilled.
Remember that temporary changes in hearing or a feeling of fullness in the ear may occur for a short time after the drug has been instilled.
 Notify the primary health care provider if symptoms do not improve or become worse.
Notify the primary health care provider if symptoms do not improve or become worse.
DRUGS USED TO REMOVE CERUMEN
 Do not put anything in the ear canal such as a Q-tip.
Do not put anything in the ear canal such as a Q-tip.
 Do not use a drug to remove cerumen if ear drainage, discharge, pain, or irritation occurs.
Do not use a drug to remove cerumen if ear drainage, discharge, pain, or irritation occurs.
 Do not use for more than 4 days. If excessive cerumen remains, consult the primary health care provider.
Do not use for more than 4 days. If excessive cerumen remains, consult the primary health care provider.
 Any wax remaining after the treatment may be removed by gently flushing the ear with warm water using a soft rubber bulb ear syringe.
Any wax remaining after the treatment may be removed by gently flushing the ear with warm water using a soft rubber bulb ear syringe.
 If dizziness occurs, consult the primary health care provider.
If dizziness occurs, consult the primary health care provider.
EVALUATION
 Therapeutic effect is achieved.
Therapeutic effect is achieved.
 Adverse reactions are identified, reported to the primary health care provider, and managed successfully with appropriate nursing interventions:
Adverse reactions are identified, reported to the primary health care provider, and managed successfully with appropriate nursing interventions:
• No evidence of infection is seen.
• Anxiety is managed successfully.
 Patient and family express confidence and demonstrate an understanding of the drug regimen.
Patient and family express confidence and demonstrate an understanding of the drug regimen.
OPHTHALMIC PREPARATIONS
Various types of preparations are used for treating ophthalmic (eye) disorders, such as glaucoma, to lower the intraocular pressure (IOP; the pressure within the eye); and to treat bacterial or viral infections of the eye, inflammatory conditions, and symptoms of allergy related to the eye.
Glaucoma
Glaucoma is a condition of the eye in which there is an increase in the IOP, causing progressive atrophy of the optic nerve with deterioration of vision and, if untreated, blindness. The eye’s lens, iris, and cornea are continuously bathed and nourished by a fluid called aqueous humor. As aqueous humor is produced, excess fluid normally flows out through a complex network of tissue called the canal of Schlemm. An angle is formed where the canal of Schlemm and iris meet. This forms a filtration angle that maintains the normal pressure within the eye by allowing excess aqueous humor to leave the anterior chamber of the eye (Fig. 53.3).
There are two types of glaucoma: angle-closure glaucoma and open-angle, or chronic, glaucoma (Fig. 53.4). The limitation of outflow in both types of glaucoma causes an accumulation of intraocular fluid, followed by increased IOP. As a result, the higher the IOP, the greater the risk of optic nerve damage, visual loss, and blindness. Some individuals have an anatomic defect that causes the angle to be more narrow than normal but do not have any symptoms and do not develop glaucoma under normal circumstances. However, certain situations, such as medication that causes dilation of the eye, fear, or pain, may precipitate an attack. The aim of treatment in glaucoma is to lower the IOP. The Summary Drug Table: Selected Ophthalmic Preparations provides examples of the drugs used to treat both glaucoma and other ophthalmic problems.
Actions and Uses
The drugs used to treat ophthalmic conditions are from the same classes of drugs used in other body systems and conditions. Systemic effects are rare because only small amounts of these preparations may be absorbed systemically.
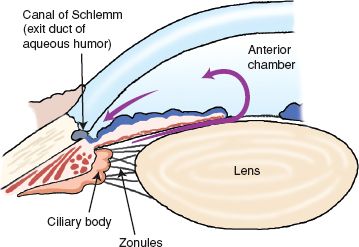
Figure 53.3 Flow of aqueous humor in the normal eye.
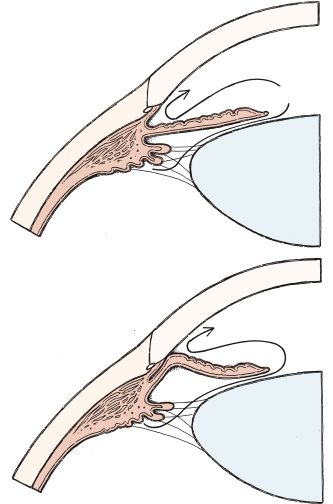
Figure 53.4 In open-angle glaucoma, the angle where aqueous humor drains is normal but does not function properly and excess fluid cannot leave the anterior chamber as shown in the top picture. In angle-closure glaucoma, the iris blocks the canal and limits the flow of aqueous humor from the anterior chamber of the eye as shown in the bottom picture.
Alpha (α)2-Adrenergic Drugs
Brimonidine is an α2-adrenergic receptor agonist used to lower IOP in patients with open-angle glaucoma or ocular hypertension. This drug acts to reduce production of aqueous humor and increase the outflow of aqueous humor.
Sympathomimetic Drugs
Sympathomimetics have α- and beta (β)-adrenergic activity (see Chapter 24 for a detailed discussion of adrenergic drugs). These drugs lower the IOP by increasing the outflow of aqueous humor in the eye and are used to treat glaucoma. Apraclonidine is used to control or prevent postoperative elevations in IOP.
α-Adrenergic Blocking Drugs
Dapiprazole acts by blocking the α-adrenergic receptor in smooth muscle and produces miosis (constriction of the pupil) through an effect on the dilator muscle of the iris. The drug is used primarily after ophthalmic examinations to reverse the diagnostic mydriasis (dilation of the pupil).
β-Adrenergic Blocking Drugs
The β-adrenergic blocking drugs decrease the rate of production of aqueous humor and thereby lower the IOP. These drugs are used to treat glaucoma.
Miotics, Direct Acting, and Cholinesterase Inhibitors
Miotics contract the pupil of the eye (miosis), resulting in an increase in the space through which the aqueous humor flows, decreasing IOP. The miotics were, for a number of years, the drug of choice for glaucoma. These drugs have lost that first-choice treatment status to the β-adrenergic blocking drugs.
Carbonic Anhydrase Inhibitors
Carbonic anhydrase is an enzyme found in many tissues of the body, including the eye. Inhibition of carbonic anhydrase in the eye decreases aqueous humor secretion, resulting in a decrease of IOP. These drugs are used in the treatment of elevated IOP seen in open-angle glaucoma. Except for dorzolamide and brinzolamide, carbonic anhydrase inhibitors are administered systemically.
Prostaglandin Agonists
Prostaglandin agonists are used to lower IOP in patients with open-angle glaucoma and ocular hypertension who do not tolerate other IOP-lowering medications or have an insufficient response to these medications. These drugs act to lower IOP by increasing the outflow of aqueous humor through the trabecular meshwork.
Mast Cell Stabilizers
Mast cell stabilizers currently approved for ophthalmic use are nedocromil and pemirolast. These drugs are used to prevent itching of the eyes caused by allergic conjunctivitis. Mast cell stabilizers inhibit the antigen-induced release of inflammatory mediators (e.g., histamine) from human mast cells.
Nonsteroidal Anti-Inflammatory Drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit prostaglandin synthesis (see Chapter 14 for a discussion of the NSAIDs), thereby exerting anti-inflammatory action. These drugs are used to treat postoperative pain and inflammation after cataract surgery, for the relief of itching of the eyes caused by seasonal allergies, and during eye surgery to prevent miosis.
Corticosteroids
These drugs possess anti-inflammatory activity and are used for inflammatory conditions, such as allergic conjunctivitis, keratitis, herpes zoster keratitis, and inflammation of the iris. Corticosteroids also may be used after injury to the cornea or after corneal transplantation to prevent rejection.
Antibiotics and Sulfonamides
Antibiotics possess antibacterial activity and are used in the treatment of eye infections. Sulfonamides possess a bacteriostatic effect against a wide range of gram-positive and gram-negative microorganisms. They are used in treating conjunctivitis, corneal ulcer, and other superficial infections of the eye. See Chapter 6 for additional information on the sulfonamides.
Silver
Silver possesses antibacterial activity against gram-positive and gram-negative microorganisms. Silver proteinate is occasionally used in the treatment of eye infections. Silver nitrate is occasionally used to prevent gonorrheal ophthalmia neonatorum (gonorrheal infection of the newborn’s eyes). Ophthalmic tetracycline and erythromycin have largely replaced the use of silver nitrate in newborns.
Antiviral Drugs
Antiviral drugs interfere with viral reproduction by altering DNA synthesis. These drugs are used in the treatment of herpes simplex infections of the eye, in the treatment of immunocompromised patients with cytomegalovirus (CMV) retinitis, and for the prevention of CMV retinitis in patients undergoing transplantation.
Antifungal Drugs
Natamycin is the only ophthalmic antifungal in use. This drug possesses antifungal activity against a variety of yeast and other fungi.
Vasoconstrictors/Mydriatics
Mydriatics are drugs that dilate the pupil (mydriasis), constrict superficial blood vessels of the sclera, and decrease the formation of aqueous humor. Depending on the specific drug and strength, these drugs may be used before eye surgery in the treatment of glaucoma, for relief of minor eye irritation, and to dilate the pupil for examination of the eye.
Cycloplegic Mydriatics
Cycloplegic mydriatics cause mydriasis and cycloplegia (paralysis of the ciliary muscle, resulting in an inability to focus the eye). These drugs are used in the treatment of inflammatory conditions of the iris and uveal tract of the eye and for examination of the eye.
Artificial Tear Solutions
These products lubricate the eyes and are used for conditions such as dry eyes and eye irritation caused by inadequate tear production. Inactive ingredients may be found in some preparations. Examples of these inactive ingredients include preservatives and antioxidants, which prevent deterioration of the product, and drugs that slow drainage of the drug from the eye into the tear duct.
Adverse Reactions
Although adverse reactions are rare, these drugs can cause visual impairment such as blurring of vision and local irritation and burning. These reactions are most often self-limiting and resolve if the patient waits a few minutes. Visual impairment that does not clear within 30 minutes after therapy should be reported to the primary health care provider.
Drugs to Treat Glaucoma
Drugs used to treat glaucoma may cause transient local reactions and systemic reactions. Although side effects are usually mild they may include:
• Locally in or near the eye—burning and stinging, headache, visual blurring, tearing, foreign body sensation, ocular allergic reactions, and ocular itching
• Systemic effects—fatigue and drowsiness, palpations, nausea
Corticosteroids
Local adverse reactions associated with administration of the corticosteroid ophthalmic preparations include elevated IOP with optic nerve damage, loss of visual acuity, cataract formation, delayed wound healing, secondary ocular infection, exacerbation of corneal infections, dry eyes, ptosis, blurred vision, discharge, ocular pain, foreign body sensation, and pruritus.
Antibiotics, Sulfonamides, and Silver
The antibiotic and sulfonamide ophthalmics are usually well tolerated, and few adverse reactions are seen. Local adverse reactions include occasional transient irritation, burning, itching, stinging, inflammation, and blurred vision. With prolonged or repeated use, a superinfection may occur.
Antiviral Drugs
Administration of the antiviral ophthalmics may cause local reactions such as irritation, pain, pruritus, inflammation, edema of the eyes or eyelids, foreign body sensation, and corneal clouding. Systemic reactions include photophobia and allergic reactions.
Antifungal Drugs
Adverse reactions are rare. Occasional local irritation to the eye may occur.
Artificial Tear Solutions
Adverse reactions are rare, but on occasion redness or irritation may occur.
Contraindications, Precautions, and Interactions
Drugs Used to Treat Glaucoma
These drugs are contraindicated in patients with hypersensitivity to the drug or any component of the drug. Adrenergic-based drugs are contraindicated in patients taking monoamine oxidase inhibitors (MAOIs). Epinephrine is contraindicated in patients with narrow-angle glaucoma, or patients with a narrow angle but no glaucoma, and aphakia (absence of the crystalline lens of the eye). Patients wearing soft contact lenses should be cautioned, because the preservative in the drug may be absorbed by soft contact lenses and discoloration of the lenses may occur. The drug is used cautiously during pregnancy (epinephrine, pregnancy category B; and apraclonidine, pregnancy category C) and lactation and in patients with cardiovascular disease, depression, cerebral or coronary insufficiency, hypertension, diabetes, hyperthyroidism, or Raynaud’s phenomenon. When brimonidine is used with central nervous system (CNS) depressants, such as alcohol, barbiturates, opiates, sedatives, or anesthetics, there is a risk for an additive CNS depressant effect. Use the drugs cautiously in combination with antihypertensive drugs and cardiac glycosides, because a synergistic effect may occur.
Adrenergic blocking drugs are contraindicated in patients with bronchial asthma, obstructive pulmonary disease, sinus bradycardia, heart block, cardiac failure, or cardiogenic shock, and in patients with hypersensitivity to the drug or any components of the drug. These drugs should not be used in conditions in which pupil constriction is not desirable, such as in acute iritis (inflammation of the iris), and in the treatment of IOP in open-angle glaucoma.
These drugs are in pregnancy category C (dapiprazole is pregnancy category B) and are used cautiously during pregnancy and lactation and in patients with cardiovascular disease, diabetes (may mask the symptoms of hypoglycemia), and hyperthyroidism (may mask symptoms of hyperthyroidism). The patient taking β-adrenergic blocking drugs for ophthalmic reasons may experience increased or additive effects when the drugs are administered with the oral β-adrenergic blockers. Coadministration of timolol and calcium antagonists may cause hypotension, left ventricular failure, and condition disturbances within the heart. There is a potential additive hypotensive effect when the β-adrenergic blocking ophthalmic drugs are administered with the phenothiazines.
Miotic drugs are contraindicated in patients with hypersensitivity to the drug or any component of the drug and in conditions where constriction is undesirable (e.g., iritis, uveitis, and acute inflammatory disease of the anterior chamber). The drugs are used cautiously in patients with corneal abrasion, pregnancy (pregnancy category C), lactation, cardiac failure, bronchial asthma, peptic ulcer, hyperthyroidism, gastrointestinal spasm, urinary tract infection, Parkinson’s disease, renal or hepatic impairment, recent myocardial infarction, hypotension, or hypertension. These drugs are also used cautiously in patients with angle-closure glaucoma, because miotics occasionally can precipitate angle-closure glaucoma by increasing the resistance to aqueous flow from posterior to anterior chamber.
Cholinesterase inhibitors are used cautiously in patients with myasthenia gravis (may cause additive adverse effects), before and after surgery, and in patients with chronic angle-closure (narrow-angle) glaucoma or those with anatomically narrow angles (may cause papillary block and increase the angle blockage). When cholinesterase inhibitors are administered with systemic anticholinesterase drugs, there is a risk for additive effects. Individuals such as farmers, warehouse workers, or gardeners working with carbamate–organophosphate insecticides or pesticides are at risk for systemic effects of cholinesterase inhibitors from absorption of the pesticide or insecticide through the respiratory tract or the skin. Individuals working with pesticides or insecticides containing carbamate–organophosphate and taking a cholinesterase inhibitor should be advised to wear respiratory masks, change clothes frequently, and wash exposed clothes thoroughly.
Drugs Used to Treat Inflammation
These drugs are contraindicated in patients with hypersensitivity to the drug or any component of the drug. The mast cell stabilizers are used cautiously in patients who wear contact lenses (preservative may be absorbed by the soft contact lenses). NSAIDs are used cautiously in patients with bleeding tendencies. When used topically, there is less risk of interactions with drugs or other substances. There is a possibility of a cross-sensitivity reaction when NSAIDs are administered to patients allergic to salicylates. Corticosteroids and antibiotics are used cautiously in patients with sulfite sensitivity, because an allergic-type reaction may result. The corticosteroid ophthalmic preparations are used cautiously in patients with infectious conditions of the eye. Prolonged use of corticosteroids may result in elevated IOP and optic nerve damage. The antibiotic and sulfonamide ophthalmics are contraindicated in patients with epithelial herpes simplex keratitis, varicella, mycobacterial infection of the eye, and fungal diseases of the eye. These drugs are pregnancy category B or C drugs and are used cautiously during pregnancy and lactation.
Artificial tears are contraindicated in patients who are allergic to any component of the solution. No precautions or interactions have been reported.
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Bilberry, also known as whortleberry, blueberry, and huckleberry, is a shrub with bluish flowers that appear in early spring and ripen in July and August. A beneficial use appears to be in promoting healthy eyes. Other benefits reportedly include improved visual acuity, improved night vision, prevention of free radical damage, and promotion of capillary blood flow in the eyes, hands, and feet. Bilberry extract has been used in treating nonspecific, mild diarrhea and as a mouthwash or gargle for inflammation of the mouth and throat. Bilberry fruit is a safe substance with no known adverse reactions or toxicity. There are no known contraindications to its use as directed unless the individual has an allergy to bilberry. The dosage of standard extract is 80 to 160 mg per day (DerMarderosian, 2003).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


