Other Special Types of Invasive Duct Carcinoma
MAMMARY CARCINOMA WITH OSTEOCLAST-LIKE GIANT CELLS
Less than 100 examples of this type of breast carcinoma have been reported since the first series was published in 1979 (1). The clinical features are generally similar to those of breast carcinoma. Patients ranged in age from 28 to 88 years, with an average age at diagnosis in three reviews of 53 years (1,2,3). Mammographically, the well-circumscribed margin of most tumors suggests a benign lesion, such as a cyst or fibroadenoma (2). The gross appearance is quite striking due to the dark brown or red-brown color of the bisected tumor. Reported diameters range from 0.5 cm to 10 cm, with most measuring 3 cm or less.
The mechanism by which osteoclast-like giant cells are formed in breast carcinoma is not known. In a case study, Sano et al. (4) found that the carcinoma cells in one such tumor secreted excess vascular endothelial growth factor (VEGF). They hypothesized that VEGF “promotes tumor angiogenesis and migration of macrophages,” which “fuse with each other,” giving rise to osteoclast-like giant cells. Additional studies are needed to evaluate this interesting observation.
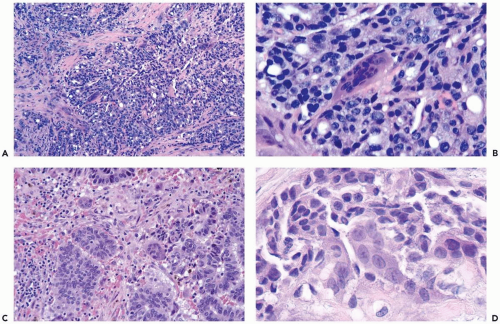
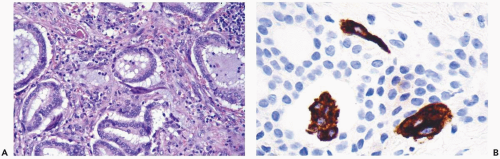
Most of these lesions are moderately or poorly differentiated invasive duct carcinomas (Fig. 20.1). A cribriform growth pattern is present relatively more often than among usual duct carcinomas. Osteoclast-like giant cells have been encountered in well-differentiated or tubular, infiltrating lobular, squamous, papillary, apocrine, mucinous, and metaplastic carcinomas (1,2,3) (Fig. 20.2). An unusual instance of bilateral invasive lobular carcinoma with osteoclast-like giant cells has been reported (5). Rarely, the carcinoma has a glandular pattern reminiscent of infiltrating colonic carcinoma. The giant cells are located close to the edges of carcinomatous glands, and they may be found in the glandular lumens. Extravasated erythrocytes and hemosiderin are usually present in the intervening highly vascular stroma. Erythrophagocytosis by the giant cells is uncommon, and they contain scant hemosiderin that is detectable by light microscopy. Fibroblastic reaction, collagenization, and lymphocytic infiltration are variably present. Mammary carcinoma with osteoclast-like giant cells may be a variant of metaplastic carcinoma that has giant cells in areas of osseous and cartilaginous differentiation (6). However, no bone, cartilage, or osteoid is found in tumors classified as mammary carcinoma with osteoclast-like giant cells.
The giant cells are stained by various antibodies that react with macrophages and osteoclasts, exhibiting strong reactivity for acid phosphatase (7,8), alpha-1-antitrypsin, KP-1 (CD68), and lysozyme (9,10) (Fig. 20.2). The tumors have had low levels of estrogen receptor, but many had remarkably high progesterone receptors (2).
Axillary lymph node metastases have been reported in approximately a third of cases. Osteoclast-like giant cells are found in some, but not all, metastases in axillary lymph nodes or other sites, and within intralymphatic tumor emboli (1,2). Nearly two-thirds of patients have been reported to be alive and well with follow-up rarely reaching beyond 5 years (1,2,10).
CRIBRIFORM CARCINOMA
Invasive carcinomas with a cribriform pattern are termed classical cribriform carcinomas. Some of these tumors have cribriform and tubular components. The diagnosis of mixed invasive cribriform carcinoma has been reserved for
tumors in which less than 50% of the lesion has a cribriform pattern and the remainder of the tumor is composed of nontubular, less well-differentiated areas. Fewer than 6% of invasive mammary carcinomas have a cribriform component, with nearly equal proportions of pure and mixed lesions (11,12).
tumors in which less than 50% of the lesion has a cribriform pattern and the remainder of the tumor is composed of nontubular, less well-differentiated areas. Fewer than 6% of invasive mammary carcinomas have a cribriform component, with nearly equal proportions of pure and mixed lesions (11,12).
A mammographic study of eight cases revealed spiculated masses measuring 20 to 35 mm in four of the patients (13). Two of these lesions contained a few punctate calcifications. Four other tumors were not visualized radiographically. Venable et al. (14) reported that 16 classical and mixed cribriform carcinomas were estrogen receptor-positive and that 11 of the 16 (69%) tumors were also progesterone receptor-positive. No appreciable difference was present in progesterone receptor positivity between classical and mixed cribriform tumors.
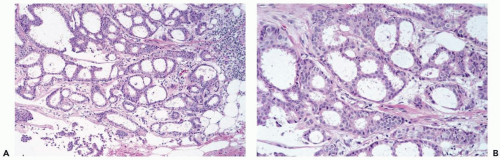
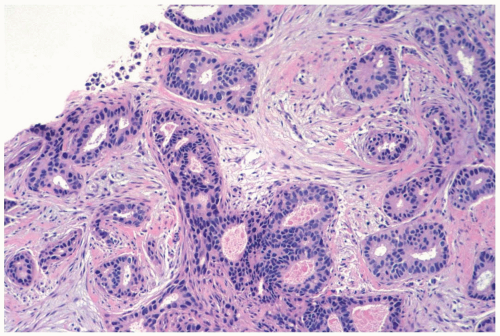
A small proportion of cribriform carcinomas occur as multifocal lesions (11,12). The invasive component of cribriform carcinoma duplicates the sieve-like growth pattern of conventional cribriform intraductal carcinoma (Fig. 20.3). The rounded and angular masses of uniform, well-differentiated tumor cells are embedded in variable amounts of collagenous stroma (Fig. 20.4). Some tumors have areas of tubular growth that comprise up to 50% of the tumor. Page et al. (11) found tubular areas in 6 of 35 classical cribriform tumors (17%). Mucin-positive secretion is present in varying amounts within the cribriform lumina, and they may contain microcalcifications (15,16). The intraductal component has a cribriform pattern in most, but not all, classical invasive cribriform carcinomas. When present, nodal metastases from classical tumors usually also have a cribriform structure, whereas metastases derived from mixed tumors are more likely to have a noncribriform pattern (11,14).
Cribriform carcinoma should be distinguished morphologically from adenoid cystic carcinoma. Cribriform growth produces a fenestrated structural pattern that lacks the cylindromatous components composed of basal lamina material characteristic of adenoid cystic carcinoma. However, cribriform areas are found in those adenoid cystic carcinomas where glands are more prominent than cylindromatous elements (17).
The majority of patients have been treated by mastectomy and axillary dissection (11,14). Two studies concluded that patients with classical cribriform carcinoma were less likely to have axillary lymph node metastases than women with mixed cribriform (11) or ordinary invasive duct carcinoma (14). No deaths due to classical cribriform carcinoma occurred among 34 patients studied by Page et al. (11), with follow-up of 10 to 21 years. Among 16 women with mixed cribriform carcinoma followed an average of 12.5 years, there were 6 deaths resulting from the
breast carcinoma. Venable et al. (14) reported a disease-free survival of 100% among 45 patients with classical cribriform carcinoma followed for 1 to 5 years.
breast carcinoma. Venable et al. (14) reported a disease-free survival of 100% among 45 patients with classical cribriform carcinoma followed for 1 to 5 years.
SMALL CELL (OAT CELL) CARCINOMA
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree