, Arthur H. Cohen2, Robert B. Colvin3, J. Charles Jennette4 and Charles E. Alpers5
(1)
Department of Pathology, Microbiology and Immunology, Vanderbilt University Medical Center, Nashville, Tennessee, USA
(2)
Department of Pathology and Laboratory Medicine, Cedars-Sinai Medical Center, Los Angeles, California, USA
(3)
Department of Pathology Harvard Medical School, Massachusetts General Hospital, Boston, Massachusetts, USA
(4)
Department of Pathology and Laboratory Medicine, University of North Carolina, Chapel Hill, North Carolina, USA
(5)
Department of Pathology, University of Washington, Seattle, Washington, USA
Abstract
Other abnormal substances besides amyloid may infiltrate glomeruli and cause significant dysfunction. Certain glomerular diseases are defined by ultrastructural features of protein deposits. While typical immune complex electron dense deposits have a uniform appearance, some disorders are characterized by an organized substructure to infiltrating proteins. These include cryoglobulinemia and lupus nephritis among others. The two discussed below were described within a few years of one another in the 1970–1980s and, for some time, were considered to be variants of the same disease.
Introduction
Other abnormal substances besides amyloid may infiltrate glomeruli and cause significant dysfunction. Certain glomerular diseases are defined by ultrastructural features of protein deposits. While typical immune complex electron dense deposits have a uniform appearance, some disorders are characterized by an organized substructure to infiltrating proteins. These include cryoglobulinemia and lupus nephritis among others. The two discussed below, fibrillary glomerulonephritis and immunotactoid glomerulopathy, were described within a few years of one another in the 1970–1980s and, for some time, were considered to be variants of the same disease.
Fibrillary Glomerulonephritis
Clinical Setting
Perhaps among the more important of these is the lesion known as fibrillary glomerulonephritis (Fig. 19.1) [1–3]. Presenting manifestations are similar to other glomerulopathies: proteinuria, frequently with nephrotic range, hematuria (70 %), renal insufficiency, and hypertension.
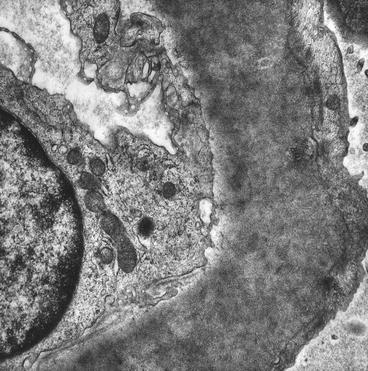
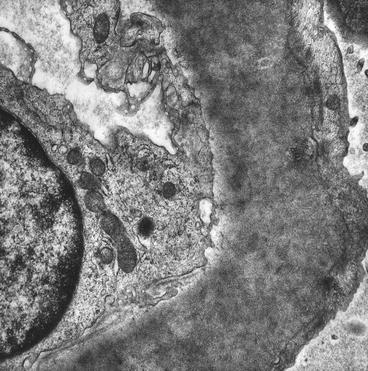
Fig. 19.1
Fibrillary glomerulonephritis; there are numerous randomly arranged fine fibrils permeating the basement membrane (electron microscopy)
Pathologic Findings
The light microscopy of glomeruli indicates variable increase in mesangial cellularity and irregularly thickened capillary walls. Crescents may be present [1, 4]. Immunofluorescence is positive, with coarse linear/confluent granular immunoglobulin G (IgG), C3, and one or both light chains. This disorder is ultrastructurally defined and is characterized by the accumulation of fibrils that are roughly 18–20 nm in thickness and are throughout the mesangial matrix and basement membranes in a manner very similar to amyloid [1]. Indeed, the fibrils bear striking similarity to amyloid. In contrast, however, the infiltrate is Congo red negative, unlike amyloid [5].
Extraglomerular and extrarenal involvement is rare [6, 7]. The typical clinical presentation is of heavy proteinuria with hematuria, hypertension, and some degree of renal insufficiency. Serologic studies are negative or noncontributory, although some patients may have a positive antinuclear antibody (ANA). Initially considered to be an idiopathic disorder, fibrillary glomerulonephritis is reported to be associated with carcinomas, dysproteinemia, or autoimmune disease in 23, 17, and 15 % of patients, respectively [8]. Thus, if not clinically evident, a biopsy diagnosis of fibrillary glomerulonephritis should stimulate a search for an associated disease. This disorder runs a chronic course with advanced renal insufficiency requiring renal replacement therapy in approximately 40 %. The nature of the fibrils is not known; one report described a circulating cryoprecipitated factor composed of immunoglobulins, light chains, and fibronectin [3]. The disease not infrequently recurs in the transplant [9, 10]. A comparison between amyloid and fibrillary glomerulonephritis is indicated in Table 19.1.
Table 19.1




Features of amyloid and fibrillary glomerulonephritis (GN)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


