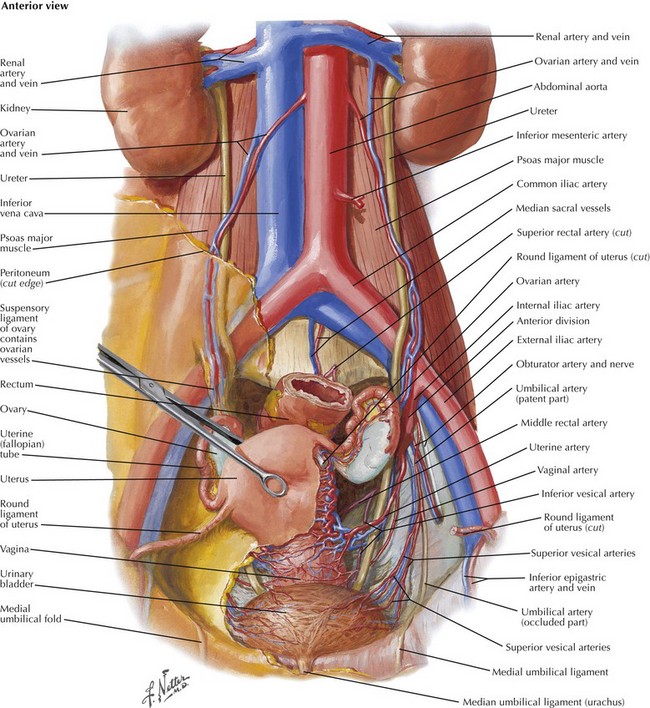
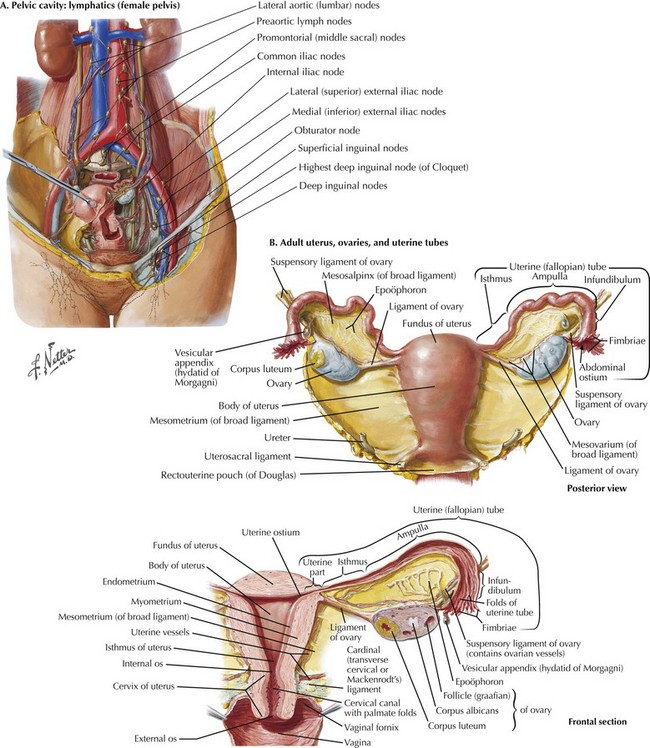
Chapter 52 The adnexa refers to both the ovary and fallopian tube. An intimate understanding of the vascular supply to the adnexa and the relationship to the underlying ureter and uterus is required before commencing surgery (Fig. 52-1). The general principles are similar regardless of surgical approach (open, laparoscopic, or robotic). The best approach to removing a pelvic mass is first to open the retroperitoneum and identify the gonadal vessels and ureter. The gonadal blood supply, or infundibulopelvic ligament (IP), originates from the aorta and runs parallel to the ureter, crossing into the pelvis over the bifurcation of the common iliac vessels (Fig. 52-2, A).
Oophorectomy for Benign and Malignant Conditions
Anatomy and Dissection of the Adnexa
Gonadal Vessels and Infundibulopelvic Ligament
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Oophorectomy for Benign and Malignant Conditions