Algorithm for addressing maternal injuries with a gravid uterus. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
A 35-year-old gravida 5, para 4004 at 34 weeks of gestation presents with a complaint of bleeding (similar to menstrual bleeding) noted on her bed when she awoke in the morning. What is the next step in management?
Obtain a detailed history especially with regards to hypertension, drug abuse, and trauma, and perform a transabdominal pelvic ultrasound to determine the location of the placenta (transvaginal ultrasound is contraindicated).
Third Trimester Bleeding
•Affects 2% to 6% of all pregnancies
•Vaginal spotting may be secondary to massive hemorrhage
•Differential diagnosis: Vasa previa, placenta previa, abruptio placenta (placental abruption)
Vasa Previa
•Umbilical vein insertion into placental membranes instead of the central region of the placenta
•Bleeding occurs when one of these vessels ruptures near the internal os
•Associated with fetal hemorrhage leading to emergent delivery via cesarean section
Placenta Previa
•Implantation of the placenta partially or completely over the cervical os
•Presents as painless bright red vaginal bleeding
•Do NOT perform a vaginal exam! (speculum exam is ok)
•Achieve maternal and fetal hemodynamic stability followed by delivery (vaginal or cesarean)
A 28-year-old woman at 20 weeks of gestation presents to the emergency department following a motor vehicle crash. She is now having abdominal pain, severe lower abdominal tenderness, and contractions. Her physical examination is significant for blood in the vagina, uterine contractions, and a fetal heart rate of 75 bpm. What diagnostic step can confirm a placental abruption?
A Kleihauer-Betke test can confirm placental abruption. It detects fetal blood in the maternal circulation.
•Deceleration injury where the placenta separates from the uterus
•Can present as vaginal bleeding, abdominal tenderness, contractions, or fetal distress
•Non-trauma-related causes/risk factors include advanced maternal age, smoking, cocaine use, maternal hypertension, multiparity, and chorioamnionitis
•High fetal mortality
•Can test for the presence of fetal blood in the maternal circulation (Kleihauer-Betke test) to confirm the diagnosis
•Achieve maternal and fetal hemodynamic stability followed by delivery as indicated (vaginal or cesarean)
A 31-year-old pregnant woman presents to the emergency department following a motor vehicle crash. She is Rh-positive. She has multiple injuries but none involving the abdomen or pelvis. On ultrasound, the uterus is intact. What is the recommended management of her Rh-positive status?
Rh immunoglobulin therapy is only indicated in the pregnant, Rh-negative trauma patient.
Trauma in Pregnancy
•Blood loss can be significant without signs of shock due to increased blood volume in pregnancy
•Emergent C-section can be performed for worsening maternal condition
•All pregnant Rh-negative trauma patients should be considered for Rh immunoglobulin therapy unless the injury is remote from the uterus
Uterine Rupture
•The most common location is the posterior fundus
•Delivery of the baby may be indicated based on viability
•Aggressive resuscitation often required until uterus clamps down after delivery
An 18-year-old female presents with a history of foul-smelling discharge for 2 days with a sudden onset of lower abdominal pain for 1 day along with some nausea and vomiting. Her past medical history is remarkable for a sexual history of five partners and multiple sexually transmitted diseases. She has not had an appendectomy. What are the possible surgical emergencies that should be ruled out prior to making the above diagnosis?
While pelvic inflammatory disease (PID) is the most likely etiology of her illness, acute appendicitis and ectopic pregnancy must be immediately ruled out.
Pelvic Inflammatory Disease
•Most commonly multibacterial (e.g., Neisseria gonorrhoeae, Chlamydia trachomatis, bacterial vaginosis, Escherichia coli, Actinomyces israelii, Mycoplasma hominis)
•Absolute diagnostic criteria include bilateral adnexal pain and cervical motion tenderness
•Relative criteria include elevated WBC, erythrocyte sedimentation rate, vaginal discharge, and fevers
•Pelvic ultrasound is useful to look for hydrosalpinx, pyosalpinx, or a tubo-ovarian abscess
•Differential diagnosis: Ovarian torsion, appendicitis, ectopic pregnancy, diverticulitis, Crohn’s disease, urinary tract infection, pyelonephritis, and nephrolithiasis in the differential diagnosis
•Outpatient treatment typically cefoxitin plus probenecid/doxycycline
•Inpatient treatment reserved for patients unable to tolerate oral intake or with complications
•Sequelae
•Infertility due to tubal damage or adhesions
•Tubo-ovarian abscess
•Diagnosed by ultrasound
•Treated with antibiotics
•If does not resolve, proceed to surgical resection or radiological drain placement in premenopausal women
•In postmenopausal women, perform a TAH-BSO because of the high incidence of cancer
A 22-year-old female was seen and diagnosed with a left ectopic pregnancy with some complex fluid in the cul-de-sac, but left against medical advice 4 hours ago with a hematocrit of 26. She has now returned with worsening pain and a hematocrit of 22. What is the next step in management?
Emergent operative salpingectomy or salpingostomy. An ectopic pregnancy is a true surgical emergency.
Ectopic Pregnancy
•A pregnancy implanted anywhere but the uterus (most commonly in the fallopian tubes)
•Risk factors include PID, previous ectopic pregnancy, presence of an intrauterine device (IUD), and diethylstilbestrol (DES) exposure
•Presents with a positive β-hCG and abdominal pain
•Ruptured ectopic pregnancies may present with shoulder pain, abdominal distention, and shock
•A physical exam may reveal a palpable adnexal mass (sometimes visible as an early fetus on ultrasound)
•Criteria for methotrexate treatment
•Hemodynamically stable (no evidence of rupture)
•Quantitative β-hCG <15,000
•No evidence of liver or renal disease
•Size <3.5 cm
•Patient can be relied upon to take the medication
•Pregnancy is not an intra-uterine
•If criteria for methotrexate treatment are not met, a surgical resection (salpingostomy or salpingectomy) is indicated
•Remember to look at the other fallopian tube at the time of surgery
A 26-year-old woman with regular menses is noted to have a firm mass in the cul-de-sac on a rectovaginal exam. The mass is slightly tender to palpation. Transvaginal ultrasonography reveals a 3 × 3 cm complex mass. What is the most appropriate next step in evaluation?
Follow up transvaginal ultrasonography in 3 months. CA-125 has a low sensitivity in premenopausal woman and should be ordered sparingly. OVA-1 test can be ordered in premenopausal women to triage and appropriately refer this patient.
•Ovarian masses less than 5 cm are generally benign
•Other signs of benign masses include simple cysts and unilateral cysts
•Common among premenopausal ovulating women
•Freely mobile
If discovered incidentally during a non-gynecological operation, do NOT perform a hysterectomy, bilateral salpingo-oophorectomy, or biopsy of the mass. If consent is already available and the mass has been discussed with the patient preoperatively, then a unilateral salpingo-oophorectomy may be appropriate.
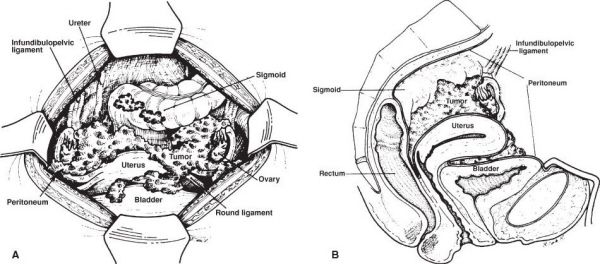
Anatomy of an ovarian tumor. (With permission from Fischer JE, Bland KI, Callery MP, et al., eds. Mastery of Surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


