Mechanisms of Progression
It has been known for many decades that individuals with CKD who have sustained a substantial loss of GFR often continue to lose renal function inexorably until they develop terminal renal failure (
28,
29,
30,
31). Although the rate of progression of renal failure varies greatly among patients, in many individuals the decline in kidney function is linear (
28,
29,
30). The percentage of patients with renal insufficiency who will progress to renal failure is not known, but it seems likely that most patients who sustain a loss of GFR of 60% or greater will show continued progression of renal failure. Renal failure may progress because of continued activity of the underlying renal disease or because of the superimposition of other diseases that may contribute to renal injury such as hypertension, adverse effects of nephrotoxic medicines (e.g., antibiotics or radiocontrast material), obstruction, kidney infection, hypercalcemia, or hyperuricemia. However, it is not rare for progression to continue even after the initial cause of the renal disease seems to have disappeared and when superimposed illnesses are not present (
32,
33,
34,
35). For example, progression of renal failure may continue in patients who have relief of urinary tract obstruction, control of hypertension, discontinuance of nephrotoxic medications, or partial recovery from acute renal failure.
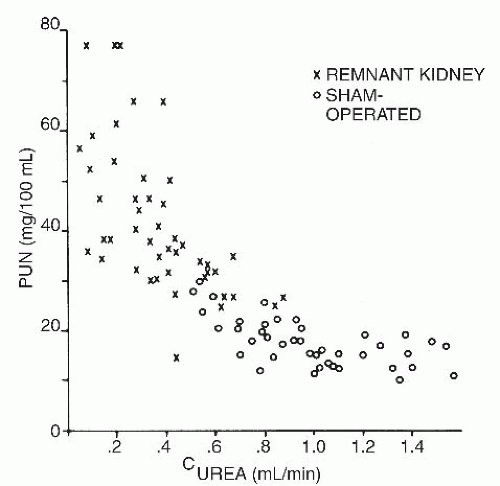
Studies of animal and in vitro models of CKD or renal failure have led to the following observations. There is a rather common set of physiologic and biochemical responses to chronic loss of renal function, that is, to a large degree, independent of the underlying type of kidney disease. When the loss of functioning nephrons becomes sufficient to cause renal insufficiency, the remaining individual functioning nephrons generally undergo an increase in the glomerular plasma flow and GFR and an enlargement in size of both the glomeruli and the tubules (i.e., nephron hypertrophy) (
36,
37). The capillary blood pressure and the blood pressure gradient across the capillary wall in the remaining functional glomeruli increase (
37,
38). In addition, the chemical and electrical, as well
as pore size, barriers to the movement of plasma proteins across the glomerulus and into the renal tubule lumen are impaired. This can lead to both proteinuria (leakage of protein into the urine) and deposition of proteins in renal tissue. This, in turn, can stimulate migration of leukocytes and monocytes, platelet aggregation, collagen deposition, cellular proliferation, and other inflammatory and scarifying changes (
39,
40). These processes may contribute to progressive renal damage. Many of the foregoing changes, some of which could be considered adaptive physiologic responses, are believed to promote further renal injury. These factors, as well as continuing activity of the underlying renal disease, can lead to progressive renal failure.
Current thinking regarding potential causes of progressive renal failure is summarized in
Table 97.2. Most of these processes have been investigated only in animal models, and it is inferred that they may play a role in human renal disease. It is pertinent that many of these mechanisms appear to be susceptible to amelioration or reversal by nutritional therapy (see
Table 97.2). For example, protein-restricted diets have been shown to reduce renal blood flow, GFR, and proteinuria in humans with renal disease (
27). Albuminuria itself is a risk factor for more rapid progression of CKD, and the magnitude of albuminuria, in general, is correlated with the rate of progression of a given type of CKD.
Human Studies on the Effect of Dietary Therapy on Progression of Chronic Renal Failure
To what extent are the animal data applicable to patients? From the mid-1970s to the present, many, but not all, dietary studies in humans with renal insufficiency have indicated that a low intake of dietary protein and phosphorus will retard the rate of progression of renal failure (
93,
94,
95,
96,
97,
98,
99,
100,
101,
102,
103,
104). Some evidence indicates that a low protein and phosphorus intake may each act separately to slow progressive renal failure (
61). The earlier studies of this question in humans suffered from one or more major defects in experimental design. Later studies, in general, were better designed. Diet studies generally evaluated low-protein, low-phosphorus diets that provide about 0.40 to 0.60 g protein/kg body weight/day or a very LPD containing about 0.28 g/kg/day (e.g., ˜16 to 25 g protein/day). This latter diet was supplemented with 10 to 20 g/day of the nine essential amino acids or of mixtures of several essential amino acids and ketoacid or hydroxyacid analogs of the other essential amino acids (
93,
95,
96,
97,
98,
100,
103). These diets were compared with either a more liberal diet containing approximately 1.0 g or more of protein/kg/day and more phosphorus or to an ad libitum diet.
The ketoacid or hydroxyacid analog is structurally identical to its corresponding essential amino acid, except that the amino (NH
2) group attached to the second (α) carbon of the amino acid is replaced with a keto group or hydroxy group, respectively. The ketoacid and hydroxyacid analogs can be transaminated in the body to the respective amino acids, although a proportion of the analogs are degraded rather than transaminated. Because the ketoacids and hydroxyacids lack the nitrogen containing amino group on the α carbon, these compounds provide the patient with a lesser nitrogen load. Because they are degraded in the body, they should engender fewer waste products that normally accumulate in renal failure. Ketoacid analogs of the branched-chain amino acids, especially of leucine, may be somewhat more likely to promote protein anabolism, possibly by decreasing protein degradation (
105,
106).
The largest and most intensive examination of whether low-protein, low-phosphorus diets retard the rate of progression of renal disease was the National Institutes of Health-funded Modification of Diet in Renal Disease (MDRD) Study (
103,
104). This project investigated, in an intention-to-treat analysis, the effects of 3 levels of dietary protein and phosphorus intakes and 2 blood pressure management goals on the progression of CKD. A total of 840 adults with various types of renal disease, but excluding diabetes mellitus, were divided into 2 study groups according to their GFR.
In Study A, 585 patients with a GFR, measured by iodine-148 iothalamate clearances, of 25 to 55 mL/1.73m
2/minute were examined. Patients were randomly assigned to either a usual-protein, usual-phosphorus diet (1.3 g/kg standard body weight/day of protein and 16 to 20 mg/kg/day of phosphorus) or to a low-protein, low-phosphorus diet (0.58 g/kg/day of protein and 5 to 10 mg/kg/day of phosphorus) and also to either a moderate or strict blood pressure goal: mean arterial blood pressure 107 mm Hg (113 mm Hg for those >61 years of age) or 92 mm Hg (98 mm Hg for those >61 years of age). Study B included 255 patients with a baseline GFR of 13 to 24 mL/1.73 m
2/minute. Patients were randomly assigned to the lowprotein, low-phosphorus diet or to the very-low-protein, very-low-phosphorus diet (0.28 g/kg/day of protein and 4 to 9 mg/kg/day of phosphorus) with a ketoacid-amino acid supplement (0.28 g/kg/day). They were also randomly assigned to either the moderate or strict blood pressure control groups, as in Study A. The adherence to the dietary protein prescription in the different diet groups was good (
103).
Among participants in Study A, those prescribed the LPD had significantly faster declines in GFR during the first 4 months than those assigned to the usual-protein diet. Thereafter, the rate of decline of the GFR in the lowprotein, low-phosphorus group was significantly slower than in the group fed the usual-protein, usual-phosphorus diet. Over the course of the entire treatment period, there was no difference in the overall rate of progression of renal failure in the two diet groups. However, it is likely that the initial greater fall in GFR in the patients prescribed the LPD may reflect a hemodynamic response to the reduction in protein intake rather than a greater rate of progression of the parenchymal renal disease. This response could in fact be beneficial, reflecting a reduction of intrarenal hyperfiltration and intrarenal hypertension. If this explanation is correct (and it is not proven that it is correct), the subsequently slower rate of progression of disease after the first 4 months of dietary treatment is consistent with a beneficial effect of this intervention on the renal disease. In Study B, the very LPD group had a marginally slower decline of GFR than the LPD group; the average rate of decline did not differ significantly between the two groups (p = .066).
In the MDRD Study, the very-low-protein ketoacidamino acid supplemented-diet was not compared with the usual protein intake. Moreover, it is possible that the lack of significant effect of the LPD on the progression of renal failure could reflect the rather short mean duration of treatment in the MDRD study—2.2 years. Indeed, if the trend toward slower progression of renal failure in the LPD groups that was present at the termination of the MDRD study had persisted during a longer follow-up period, a statistically significantly slower progression would have been observed with the 0.60 g/kg protein diet in Study A and the very-low-protein, ketoacid-amino acid-supplemented diet in Study B. Several other characteristics of the patient population and study design of the MDRD may have led to the lack of a statistically significant difference in progression of renal failure between the diet groups (
107).
It is also reported that vegetarian LPDs providing soy protein may retard progression of CRF more effectively than diets of similar protein content that contain animal protein (
52,
108,
109). The mechanisms of such an effect is not known, but it may be related to the total content and different composition of fats in the vegetarian diet. The vegetarian diet is reported to improve the serum lipid profile in patients with CKD and the nephrotic syndrome (
109,
110).
Several published metaanalyses have evaluated clinical trials of the effects of LPDs on the rate of progression of kidney failure. In general, the LPDs were also low in phosphorus. These metaanalyses each evaluated a somewhat different series of clinical trials, only some of which included the MDRD study (
111,
112,
113,
114). Three of the metaanalyses used, as the key outcome, the onset of end stage renal disease (ESRD) as determined by the patient with CRF who is starting treatment with MHD or CPD or receiving a kidney transplant (
111,
112,
114). These metaanalyses reported statistically significant reductions in the relative risk of a patient with CRF assigned to the LPDs reaching this end point to 0.54, about 0.67, and 0.61, respectively. One metaanalysis used the rate of decrease in GFR as the key outcome (
113). This last study described a slowing in the progression of renal failure of only 6% which, although statistically significant, was of questionable clinical significance.
The discrepancy between these two sets of findings may be explained in part by the fact that ingestion of LPDs leads to a reduction in the generation of metabolic products of protein and amino acids, and that some of these metabolic products are toxic. Indeed, patients ingesting LPDs are reported to be started on MHD or CPD at lower GFRs than are individuals with higher protein intakes. The fact that LPDs may ameliorate uremic symptoms and delay the need to inaugurate dialysis treatment or renal transplantation can be considered to be an advantage in itself to these LPDs, even if the degree of delay in the rate of progression of CKD is not very large. In this regard, in another study, elderly patients with GFRs of 5 to 7 mL/minute/1.73 m
2 were randomly assigned to treatment with MD or with a very-low-protein ketoacid-amino acid diet. The latter patients were treated with the ketoacid diet for 1.0 to 58.1 months (median, 10.7) (
115). The patients who were assigned to the ketoacid diet appeared to fare as well clinically and nutritionally as did those who were assigned initially to MD.
The foregoing metaanalyses also examined clinical trials that used an intention-to-treat type of analysis, whereby the data from individuals assigned to a given dietary intake were included in the results, whether or not they adhered to the dietary prescription or even were available for follow-up testing. Thus, these studies do not rule out the possibility that people who adhere closely to these LPDs may not have a significant delay in the rate of progression of their CKD.
Another metaanalysis analyzed the results of five prospective clinical trials of the effects of LPDs on progression of renal failure in patients with insulin-dependent diabetes mellitus (
112). This analysis indicated that LPDs also retard progression in these individuals. However, the results were much less definitive because smaller numbers of patients were analyzed; two of the trials had no randomized, concurrent control group, and the key end points were less definitive.
In a secondary analysis of Study B, in which the decrease in GFR was correlated with the actual quantity of protein ingested, there was no effect of ingesting the LPD versus the very LPD supplemented with ketoacids and amino acids on the progression of renal failure (
104). However, in Study A, when the data from the two groups were combined and then analyzed, there was a significant inverse relationship between the protein intake actually ingested, as determined from the urea nitrogen appearance (UNA) (see later), and the rate of decline in GFR (
104). The actual dietary protein intake associated with the lowest rate of decline in GFR was about 0.62 g/kg/day. More recently, at least one other small-scale randomized controlled study compared treatment with a very-lowprotein, ketoacid-amino acid-supplemented diet to a 0.6 g/day protein diet in patients with CKD. The results indicated that the ketoacid diet was more effective at slowing progression of CKD (
116).
The mechanism of action by which ketoacid diets retard progression of renal failure is unclear. Studies suggest that alkalinization of the urine can retard the progression of renal failure (
117,
118,
119). Because ketoacids in the dietary supplements are present as alkaline salts, perhaps it is the alkali in these supplements that actually retards progression of renal failure, if the rate of progression is indeed slowed.
A 12-year follow-up analysis was conducted in the Study A MDRD patients concerning the hazard ratio, adjusted for baseline characteristics, of developing ESRD or a combination of either ESRD or all-cause mortality (
120). ESRD was defined as commencing MD therapy
or receiving a kidney transplant. This study indicated that during the first 6 years after the onset of the dietary protein prescription, there was a statistically significant adjusted lower hazard ratio of incurring ESRD, or the combination of either ESRD or mortality in those assigned to the 0.60 g protein/kg/day diet versus those assigned to the 1.3 g protein/kg/day diet (
120). This difference tended to reverse itself in the second 6-year period of follow-up.
In Study B patients, those assigned to the ketoacid supplemented diet had a significantly greater hazard ratio, adjusted for baseline factors, for death after they developed ESRD during the 12 years after assignment to their diet prescription (
121). These data are particularly intriguing because patients were treated in the study, on average, only for the first 2.2 years of follow-up and were then referred back to their usual physicians. Moreover, with few exceptions, ketoacid mixtures were not available to patients in the United States after the MDRD Study ended. Thus, the Study B patients could not have taken ketoacids during most of this 12-year observation period. A rather large, retrospective study from France did not confirm any difference in long-term mortality rate in patients with CKD who are prescribed ketoacid diets (
122). However, this study compared survival of these former patients with survival data from the French dialysis registry and with patients who underwent transplant procedures in Bordeaux. It is possible that the patients who agreed to take the ketoacid diets were a more motivated, capable, disciplined, and healthier group of individuals; and one could imagine that, all else equal, their survival rate should be greater than that of the average French dialysis patient.
The Nurses’ Health Study compared spontaneous protein intakes of individuals with different levels of GFR, determined from their serum creatinine concentrations (
123). In this study, 1624 women, aged 42 to 68 years, had their protein intake measured in 1990 and again in 1994 using a semiquantitative food frequency questionnaire. Those women with mildly reduced baseline estimated GFR levels that were greater than 55 mL/minute/1.73 m
2 but less than 80 mL/minute/1.73 m
2 showed a fall in GFR of −1.69 mL/minute/1.73 m
2 per 10-g increase in protein intake. However, after adjustment for measurement of error, the change in estimated GFR was −7.72 mL/minute/1.73 m
2 per 10-g increase in protein intake. This association was of borderline statistical significance. A high intake of nondairy animal protein in people with mild renal insufficiency was associated with a significantly greater fall in estimated GFR (− 1.21 mL/minute/1.73 m
2 per 10-g increase in nondairy animal protein intakes). A retrospective study in renal transplant recipients indicated that those recipients who spontaneously ingested higher protein diets experienced greater losses of GFR (
124).
Taken together, the post hoc analysis of the MDRD Study data, the results of the approximately 12 years of follow-up to the MDRD Study, the Nurses’ Health Study, the study in renal transplant recipients, the four metaanalyses, and the newer randomized ketoacid studies all point to the probability that LPDs will retard the rate of progression of renal failure in individuals with CKD. Moreover, because these LPDs often engender sufficiently lower uremic toxicity for a given level of reduced renal function, patients fed these diets may be able to avoid MHD, CPD, or renal transplantation at GFR levels that would require individuals ingesting higher protein intakes to commence such therapy.
An interesting question is whether LPDs may prevent or retard the development of renal failure in individuals with no underlying renal disease. At the present time, there are no clear answers to this question.
Another unresolved issue is whether LPDs will retard progression of renal failure in patients receiving ACEIs and/or ARBs. Because dietary protein restriction exerts many of the same hemodynamic and other physiologic effects on the kidney as do ACEIs and ARBs (
44,
45,
125), it is possible that the renal-protective effects of LPDs, when combined with ACEIs and ARBs, are replicative, rather than additive. In a rather small study, 82 patients with type 1 diabetes mellitus were randomly assigned to an LPD (0.60 g protein/kg/day) or a more usual-protein diet (
126); most of the patients were receiving ACEIs. In this 4-year trial, the low-protein group experienced a 10% incidence of death or ESRD as compared with 27% in the patients eating the usual-protein diet
(p < .042). There was no difference in the rate of decline in GFR in the 2 groups (
126).
Because proteinuria is associated with greater progression of renal failure and increased risk of cardiovascular disease, and because ACEIs and ARBs, even in combination, and blood pressure lowering may reduce proteinuria but not eradicate it, there may be a role for LPDs at least in persistently proteinuric patients. More research in this area is clearly needed.