Body weight and lean mass in males and females. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
Ideal and Adjusted Body Weight
•IBW is calculated using the following formula:
•Women: 100 lbs for 5΄0˝ of height, plus 5 lbs for each inch over 5΄0˝
•Men: 106 lbs for 5΄0˝ of height, plus 6 lbs for each inch over 5΄0˝
•For individuals shorter than 5΄0˝ subtract 2 lbs for every inch under 5΄0˝
•Adjusted body weight = ((actual weight – IBW) × 0.25) + IBW
•In the patient above, ((263 – 115) × 0.25) + 115 = 152 lbs
A 27-year-old female develops an anastomotic leak 5 days after undergoing Roux-en-Y gastric bypass surgery. Conservative treatment with TPN is planned. Her weight on admission is 300 lbs, and her height is 5’. How should her caloric requirements be calculated?
There are three different methods for calculating caloric requirement: rough estimate, Harris-Benedict equation, and indirect calorimetry and Weir equation, each of which is described in further detail below.
1.Rough estimate
•25 kcal/kg/day (35 kcal/kg/day for a critically ill or stressed patient)
2.Calculation of basal energy expenditure (BEE) using the Harris-Benedict equation:
•Female BEE (kcal/day) = 655+ (9.6 × wt in kg) + (1.8 × ht in cm) – (4.7× age)
•Male BEE (kcal/day) = 66 + (13.7 × wt in kg) + (5 × ht in cm) – (6.8 × age)
•NOTE: It is NOT necessary to memorize these formulas
•Use actual body weight for non-obese or underweight patients
•Use adjusted body weight for obese patients (>120% of IBW)
3.Calculation of BEE using indirect calorimetry and the Weir Equation
•This method measures oxygen consumed in L/minute (VO2) and carbon dioxide produced in L/minute (VCO2) to estimate the 24-hour resting energy expenditure
•BEE = [(3.9 × VO2) + (1.1 × VCO2)] × 1.44 – (2.8 × UUN)
•UUN = 24-hour urinary urea nitrogen
•Indications for use of indirect calorimetry
•Multiple trauma victim
•Severe sepsis
•Failure to wean from ventilator
•Morbid obesity
•Poorly healing wounds
•Burn patient
•To account for the increased caloric requirements under stress, the BEE may be multiplied by a stress factor based on the patient’s condition.
•Low stress: 1.2
•Moderate stress: 1.3
•Severe stress: 1.5
•Burns and sepsis: 2.0 to 2.5
A 70-year-old female with a history of COPD on TPN has persistent difficulty weaning from the ventilator due to CO2 retention. What nutritional modifications can be made to optimize her chances of extubation?
Indirect calorimetry may be used to determine the respiratory quotient (RQ) of this patient. The RQ can be used to adjust the nutritional composition of the TPN. For this case, it may be possible to reduce CO2 production by decreasing the carbohydrate load in the TPN.
Respiratory Quotient
•RQ is a measure of energy expenditure
•RQ = Carbon dioxide produced (VCO2)/oxygen consumed (VO2)
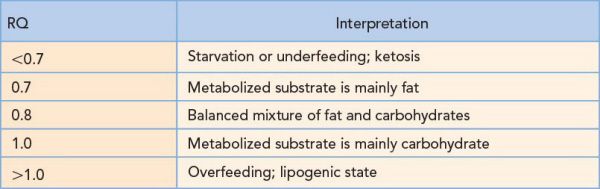
It is important to keep the RQ between 0.7 and 1.0 to prevent fat accumulation in the liver and to alleviate potential respiratory distress secondary to excess glucose.
Which of the following two patients should the surgeon be more concerned about with regard to nutritional status: A well-appearing 35-year-old female with rheumatoid arthritis and a serum albumin level of 2.8, or a 64-year-old male with esophageal cancer preparing for transhiatal esophagectomy with an albumin of 2.8 and a BMI of 17.8?
The 35-year-old female with rheumatoid arthritis is most likely not malnourished. Visceral proteins (albumin, prealbumin, and transferrin), which are commonly used to estimate nutritional status, are influenced by many non-nutritional factors. This patient’s low serum albumin (normal >3.5 g/dL) is likely due to chronic inflammation from her rheumatoid arthritis. The 64-year-old male with esophageal cancer, on the other hand, has an albumin <3.5 and is most likely malnourished from the disease process and his inability to eat. This is reflected in his low BMI of 17.8.
Assessment of Nutritional Status
•BMI and serum albumin are the most commonly used objective markers of nutritional status
•A preoperative BMI <18.5 kg/m2 or albumin <3.5 g/dL is associated with increased morbidity
•Serum albumin is best used as an initial marker of the patient’s overall nutritional status
•It is not a good measure of acute changes in nutritional status because of its long half-life (21 days)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


