High-Yield Terms to Learn
Antipyretic A drug that reduces fever (eg, aspirin, NSAIDs, acetaminophen) Cyclooxygenase (COX) The enzyme at the head of the enzymatic pathway for prostaglandin synthesis (Figure 36-2) Cytotoxic drug Drugs that interfere with essential metabolic processes, especially DNA maintenance and replication and cell division. Such drugs generally kill rapidly dividing cells and are used for cancer chemotherapy and immunosuppression (Chapters 54 and 55) Disease-modifying antirheumatic drugs (DMARDs) Diverse group of drugs that modify the inflammatory processes underlying rheumatoid arthritis; they have a slow (weeks to months) onset of clinical effects Nonsteroidal anti-inflammatory drugs (NSAIDs) Inhibitors of cyclooxygenase; the term nonsteroidal differentiates them from steroid drugs that mediate anti-inflammatory effects through activation of glucocorticoid receptors (eg, cortisol; Chapter 39) Reye’s syndrome A rare syndrome of rapid liver degeneration and encephalitis in children treated with aspirin during a viral infection Tumor necrosis factor- (TNF-
(TNF- ) A cytokine that plays a central role in inflammation Uricosuric agent A drug that increases the renal excretion of uric acid Xanthine oxidase A key enzyme in the purine metabolism pathway that ends with the production of uric acid
) A cytokine that plays a central role in inflammation Uricosuric agent A drug that increases the renal excretion of uric acid Xanthine oxidase A key enzyme in the purine metabolism pathway that ends with the production of uric acid
Aspirin & Other Nonselective NSAIDs
Classification and Prototypes
Aspirin (acetylsalicylic acid) is the prototype of the salicylates and other nonsteroidal anti-inflammatory drugs (NSAIDs; Table 36-1). The other older nonselective NSAIDs ( ibuprofen , indomethacin , many others) vary primarily in their potency, analgesic and anti-inflammatory effectiveness, and duration of action. Ibuprofen and naproxen have moderate effectiveness; indomethacin has greater anti-inflammatory effectiveness; and ketorolac has greater analgesic effectiveness. Celecoxib was the first member of a newer NSAID subgroup, the cyclooxygenase-2 (COX-2)-selective inhibitors, which were developed in an attempt to lessen the gastrointestinal toxicity associated with COX inhibition while preserving efficacy. Unfortunately, clinical trials involving some of the highly selective COX-2 inhibitors have shown a higher incidence of cardiovascular thrombotic events than the nonselective drugs.
TABLE 36-1 Selected NSAIDs.
Drug Half-life (hours) Aspirin 0.25 Celecoxib 11 Diclofenac 1.1 Diflunisal 13 Etodolac 6.5 Fenoprofen 2.5 Flurbiprofen 3.8 Ibuprofen 2 Indomethacin 4-5 Ketoprofen 1.8 Ketorolac 4-10 Meloxicam 20 Nabumetonea
26 Naproxen 14 Oxaprozin 58 Piroxicam 57 Sulindac 8 Tolmetin 1
aNabumetone is a prodrug; the half-life is for its active metabolite.
(Modified and reproduced, with permission, from Katzung BG, editors: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009.)
Mechanism of Action
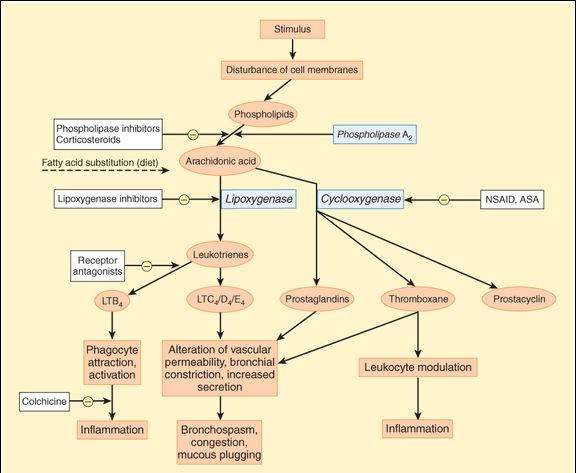
As noted in Chapter 18, cyclooxygenase is the enzyme that converts arachidonic acid into the endoperoxide precursors of prostaglandins, important mediators of inflammation (Figure 36-1). Cyclooxygenase has at least 2 isoforms: COX-1 and COX-2. COX-1 is primarily expressed in noninflammatory cells, whereas COX-2 is expressed in activated lymphocytes, polymorphonuclear cells, and other inflammatory cells.
FIGURE 36-1
Prostanoid mediators derived from arachidonic acid and sites of drug action. ASA, acetylsalicylic acid (aspirin); LT, leukotriene; NSAID, nonsteroidal anti-inflammatory drug.
(Reproduced, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009: Fig. 36-2.)
Aspirin and nonselective NSAIDs inhibit both cyclooxygenase isoforms and thereby decrease prostaglandin and thromboxane synthesis throughout the body. Release of prostaglandins necessary for homeostatic function is disrupted, as is release of prostaglandins involved in inflammation. The COX-2-selective inhibitors have less effect on the prostaglandins involved in homeostatic function, particularly those in the gastrointestinal tract.
The major difference between the mechanisms of action of aspirin and other NSAIDs is that aspirin (but not its active metabolite, salicylate) acetylates and thereby irreversibly inhibits cyclooxygenase, whereas the inhibition produced by other NSAIDs is reversible. The irreversible action of aspirin results in a longer duration of its antiplatelet effect and is the basis for its use as an antiplatelet drug (Chapter 34).
Effects
Arachidonic acid derivatives are important mediators of inflammation; cyclooxygenase inhibitors reduce the manifestations of inflammation, although they have no effect on underlying tissue damage or immunologic reactions. These inhibitors also suppress the prostaglandin synthesis in the CNS that is stimulated by pyrogens and thereby reduces fever (antipyretic action). The analgesic mechanism of these agents is less well understood. Activation of peripheral pain sensors may be diminished as a result of reduced production of prostaglandins in injured tissue; in addition, a central mechanism is operative. Cyclooxygenase inhibitors also interfere with the homeostatic function of prostaglandins. Most important, they reduce prostaglandin-mediated cytoprotection in the gastrointestinal tract and autoregulation of renal function.
Pharmacokinetics and Clinical Use
Aspirin
Aspirin has 3 therapeutic dose ranges: The low range (<300 mg/d) is effective in reducing platelet aggregation; intermediate doses (300-2400 mg/d) have antipyretic and analgesic effects; and high doses (2400-4000 mg/d) are used for an anti-inflammatory effect. Aspirin is readily absorbed and is hydrolyzed in blood and tissues to acetate and salicylic acid. Salicylate is a reversible nonselective inhibitor of cyclooxygenase. Elimination of salicylate is first order at low doses, with a half-life of 3-5 h. At high (anti-inflammatory) doses, half-life increases to 15 h or more and elimination becomes zero order. Excretion is via the kidney.
Other NSAIDs
The other NSAIDs are well absorbed after oral administration. Ibuprofen has a half-life of about 2 h, is relatively safe, and is the least expensive of the older, nonselective NSAIDs. Naproxen and piroxicam are noteworthy because of their longer half-lives (Table 36-1), which permit less frequent dosing. These other NSAIDs are used for the treatment of mild to moderate pain, especially the pain of musculoskeletal inflammation such as that seen in arthritis and gout. They are also used to treat many other conditions, including dysmenorrhea, headache, and patent ductus arteriosus in premature infants. Ketorolac is notable as a drug used mainly as a systemic analgesic, not as an anti-inflammatory (although it has typical nonselective NSAID properties). It is the only NSAID available in a parenteral formulation. Nonselective NSAIDs reduce polyp formation in patients with primary familial adenomatous polyposis. Long-term use of NSAIDs reduces the risk of colon cancer.
Toxicity
Aspirin
The most common adverse effect from therapeutic anti-inflammatory doses of aspirin is gastric upset. Chronic use can result in gastric ulceration, upper gastrointestinal bleeding, and renal effects, including acute failure and interstitial nephritis. Aspirin increases the bleeding time. When prostaglandin synthesis is inhibited by even small doses of aspirin, persons with aspirin hypersensitivity (especially associated with nasal polyps) can experience asthma from the increased synthesis of leukotrienes. This type of hypersensitivity to aspirin precludes treatment with any NSAID. At higher doses of aspirin, tinnitus, vertigo, hyperventilation, and respiratory alkalosis are observed. At very high doses, the drug causes metabolic acidosis, dehydration, hyperthermia, collapse, coma, and death. Children with viral infections who are treated with aspirin have an increased risk for developing Reye’s syndrome, a rare but serious syndrome of rapid liver degeneration and encephalopathy.
Nonselective NSAIDs
Like aspirin, these agents are associated with significant gastrointestinal disturbance, but the incidence is lower than with aspirin. There is a risk of renal damage with any of the NSAIDs, especially in patients with preexisting renal disease. Because these drugs are cleared by the kidney, renal damage results in higher, more toxic serum concentrations. Use of parenteral ketorolac is generally restricted to 72 h because of the risk of gastrointestinal and renal damage with longer administration. Serious hematologic reactions have been noted with indomethacin.
COX-2-Selective Inhibitors
The COX-2-selective inhibitors (celecoxib, rofecoxib, valdecoxib) have a reduced risk of gastrointestinal effects, including gastric ulcers and serious gastrointestinal bleeding. The COX-2 inhibitors carry the same risk of renal damage as nonselective COX inhibitors, presumably because COX-2 contributes to homeostatic renal effects. Clinical trial data suggest that highly selective COX-2 inhibitors such as rofecoxib and valdecoxib carry an increased risk of myocardial infarction and stroke. The increased risk of arterial thrombosis is believed to be due to the COX-2 inhibitors having a greater inhibitory effect on endothelial prostacyclin (PGI2 ) formation than on platelet TXA2 formation. Prostacyclin promotes vasodilation and inhibits platelet aggregation, whereas TXA2 has the opposite effects. Several COX-2 inhibitors have been removed from the market, and the others are now labeled with warnings about the increased risk of thrombosis.
Acetaminophen
Classification and Prototype
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree