Objectives
- Lists and describes the mechanisms by which the lung is protected from the contaminants in inspired air.
- Describes the “air-conditioning” function of the upper airways.
- Describes the filtration and removal of particles from the inspired air.
- Describes the removal of biologically active material from the inspired air.
- Describes the reservoir and filtration functions of the pulmonary circulation.
- Lists the metabolic functions of the lung, including the handling of vasoactive materials in the blood.
Nonrespiratory Functions of the Lung: Introduction
The main function of the respiratory system in general and of the lung in particular is gas exchange. However, the lung has several other tasks. These nonrespiratory functions of the lung include its own defense against inspired particulate matter, the storage and filtration of blood for the systemic circulation, the handling of vasoactive substances in the blood, and the formation and release of substances used in the alveoli or circulation.
Pulmonary Defense Mechanisms
![]() Every day about 10,000 L of air is inspired into the airways and the lungs, bringing it into contact with approximately 50 to 100 m2 of what may be the most delicate tissues of the body. This inspired air contains (or may contain) dust, pollen, fungal spores, ash, and other products of combustion; microorganisms such as bacteria; particles of substances such as asbestos and silica; and hazardous chemicals or toxic gases. As one reviewer (Green) put it, “Each day a surface as large as a tennis court is exposed to a volume of air and contaminants that would fill a swimming pool.” In this section, the mechanisms by which the lungs are protected from contaminants in inspired air, as well as from material such as liquids, food particles, and bacteria that may be aspirated (accidentally inspired from the oropharynx or nasopharynx) into the airways, are discussed.
Every day about 10,000 L of air is inspired into the airways and the lungs, bringing it into contact with approximately 50 to 100 m2 of what may be the most delicate tissues of the body. This inspired air contains (or may contain) dust, pollen, fungal spores, ash, and other products of combustion; microorganisms such as bacteria; particles of substances such as asbestos and silica; and hazardous chemicals or toxic gases. As one reviewer (Green) put it, “Each day a surface as large as a tennis court is exposed to a volume of air and contaminants that would fill a swimming pool.” In this section, the mechanisms by which the lungs are protected from contaminants in inspired air, as well as from material such as liquids, food particles, and bacteria that may be aspirated (accidentally inspired from the oropharynx or nasopharynx) into the airways, are discussed.
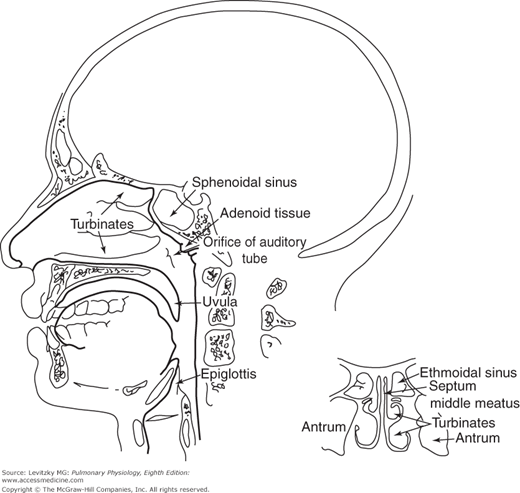
The temperature and the humidity of the ambient air vary widely, and the alveoli must be protected from the cold and from drying out. The mucosa of the nose, the nasal turbinates, the oropharynx, and the nasopharynx have a rich blood supply and constitute a large surface area. The nasal turbinates alone have a surface area said to be about 160 cm2. As inspired air passes through these areas and continues through the tracheobronchial tree, it is heated to body temperature and humidified if one is breathing through the nose.
Because the olfactory receptors are located in the posterior nasal cavity rather than in the trachea or alveoli, a person can sniff to attempt to detect potentially hazardous gases or dangerous material in the inspired air. This rapid, shallow inspiration brings gases into contact with the olfactory sensors without bringing them into the lung. Of course, not all hazardous gases have an odor that can be detected, for example, carbon monoxide.
The respiratory tract has an elaborate system for the filtration of the inspired air and the removal of particulate matter from the airways. The filtration system works better if one is breathing through the nose.
Inhaled particles may be deposited in the respiratory tract as a result of impaction, sedimentation, Brownian motion, and other, less important mechanisms. Air passing through the nose is first filtered by passing through the nasal hairs, or vibrissae. This removes most particles larger than 10 to 15 μm in diameter. Most of the particles greater than 10 μm in diameter are removed by impacting in the large surface area of the nasal septum and turbinates (Figure 10–1). The inspired air stream changes direction abruptly at the nasopharynx so that many of these larger particles impact on the posterior wall of the pharynx because of their inertia. The tonsils and adenoids are located near this impaction site, providing immunologic defense against biologically active material filtered at this point. Air entering the trachea contains few particles larger than 10 μm, and most of these will impact mainly at the carina or within the bronchi.
Sedimentation of most particles in the size range of 2 to 5 μm occurs by gravity in the smaller airways, where airflow rates are extremely low. Thus, most of the particles between 2 to 10 μm in diameter are removed by impaction or sedimentation and become trapped in the mucus that lines the upper airways, trachea, bronchi, and bronchioles. Smaller particles and all foreign gases reach the alveolar ducts and alveoli. Some smaller particles (0.1 μm and smaller) are deposited as a result of Brownian motion due to their bombardment by gas molecules. The other particles, between 0.1 and 0.5 μm in diameter, mainly stay suspended as aerosols, and about 80% of them are exhaled.
Filtered or aspirated material trapped in the mucus that lines the respiratory tract can be removed in several ways.
Mechanical or chemical stimulation of receptors in the nose, trachea, larynx, or elsewhere in the respiratory tract may produce bronchoconstriction to prevent deeper penetration of the irritant into the airways and may also produce a cough or a sneeze. A sneeze results from stimulation of receptors in the nose or nasopharynx; a cough results from stimulation of receptors in the trachea. In either case, a deep inspiration, often near to the total lung capacity, is followed by a forced expiration against a closed glottis. Intrapleural pressure may rise to more than 100 mm Hg during this phase of the reflex. The glottis opens suddenly, and pressure in the airways falls rapidly, resulting in compression of the airways and an explosive expiration, with linear airflow velocities said to approach the speed of sound. Such high airflow rates through the narrowed airways are likely to carry the irritant, along with some mucus, out of the respiratory tract. In a sneeze, of course, the expiration is via the nose; in a cough, the expiration is via the mouth. The cough or sneeze reflex is also useful in helping to move the mucous lining of the airways toward the nose or mouth. The term “cough” is not specific to this complete involuntary respiratory reflex. Coughs can be initiated by many causes, including postnasal drip from allergies or viral infections, asthma, gastroesophageal reflux disease, as an adverse effect of the very commonly prescribed angiotensin-converting enzyme inhibitors, mucus production from chronic bronchitis, infections, and bronchiectasis. Voluntary coughs are not usually as pronounced as the violent involuntary reflex described above.
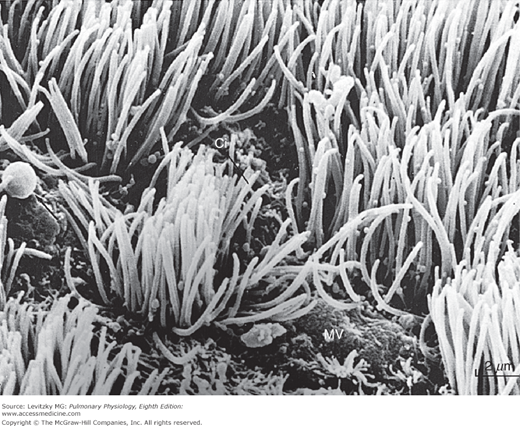
The entire respiratory tract, from the upper airways down to the terminal bronchioles, is lined by a mucus-covered ciliated epithelium, with an estimated total surface area of 0.5 m2. The only exceptions are parts of the pharynx and the anterior third of the nasal cavity. A typical portion of the epithelium of the airways (without the layer of mucus that would normally cover it) is shown in Figure 10–2.
The airway secretions are produced by goblet cells and mucus-secreting glands. The mucus is a complex polymer of mucopolysaccharides. The mucous glands are found mainly in the submucosa near the supporting cartilage of the larger airways. In pathologic states, such as chronic bronchitis, the number of goblet cells may increase and the mucous glands may hypertrophy, resulting in greatly increased mucous gland secretion and increased viscosity of mucus.
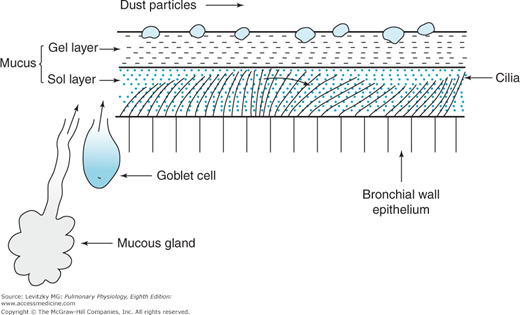
The cilia lining the airways beat in such a way that the mucus covering them is always moved up the airway, away from the alveoli, and toward the pharynx, as shown in Figure 10-3. The mucus comprises 2 layers, an outer gel layer with trapped inspired particles and a sol layer that directly covers the ciliated epithelium. The mucus is normally 5- to 100-microns thick and has a fairly low pH of 6.6 to 6.9. Exactly how the ciliary beating is coordinated is unknown—the cilia do not appear to beat synchronously but instead probably produce local waves. The mucous blanket appears to be involved in the mechanical linkage between the cilia. The cilia beat at frequencies between 600 and 900 beats/min, and the mucus moves progressively faster as it travels from the periphery. In small airways (1–2 mm in diameter), linear velocities range from 0.5 to 1 mm/min; in the trachea and bronchi, linear velocities range from 5 to 20 mm/min. Several studies have shown that ciliary function is inhibited or impaired by cigarette smoke.
The “mucociliary escalator” is an especially important mechanism for the removal of inhaled particles that come to rest in the airways. Material trapped in the mucus is continuously moved upward toward the pharynx. This movement can be greatly increased during a cough, as described previously. Mucus that reaches the pharynx is usually swallowed, expectorated, or removed by blowing one’s nose. It is important to remember that patients who cannot clear their tracheobronchial secretions (an intubated patient or a patient who cannot cough adequately) continue to produce secretions. If the secretions are not removed from the patient by suction or other means, airway obstruction will develop.
Dendritic cells, like the alveolar macrophages discussed in the next section, are mononuclear phagocytic cells. They inhabit the airways all the way from the trachea to the terminal respiratory units. “Immature” dendritic cells can phagocytize bacteria and other antigens or ingest them by pinocytosis. After contact with antigens, they “mature” and migrate to lymphoid tissues to promote tolerance to the antigen and prevent the immune response by releasing anti-inflammatory cytokines, or if the antigen is recognized as a pathogen, activate T-lymphocytes and the immune response and inflammation by releasing stimulatory molecules.
Inspired material that reaches the terminal airways and alveoli may be removed in several ways, including ingestion by alveolar macrophages, nonspecific enzymatic destruction, entrance into the lymphatics, and immunologic reactions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree