QUESTION 25.1
A. Desquamative interstitial pneumonia
B. Giant cell interstitial pneumonia
C. Lymphocytic interstitial pneumonia
D. Nonspecific interstitial pneumonia
E. Usual interstitial pneumonia
2. A 38-year-old woman with a history of heavy smoking presents with slowly progressive respiratory insufficiency. Chest x-rays show a bilateral ground-glass interstitial infiltrate involving the lung base. An open lung biopsy reveals the following histopathologic changes: alveolar spaces filled with histiocytes, hyperplasia of alveolar type II cells, and lymphomonocytic, plasma cell, and neutrophilic interstitial infiltrate. These changes are relatively homogeneous. The most likely diagnosis is:
A. Centriacinar emphysema with chronic bronchitis
B. Desquamative interstitial pneumonia
C. Nonspecific interstitial pneumonia
D. Respiratory bronchiolitis
E. Usual interstitial pneumonia
3. Extrinsic allergic alveolitis (also called hypersensitivity pneumonitis) is a reaction to long-term exposure to various antigens of animal or plant origin. The inflammatory infiltrate present in the lung is predominantly composed of:
A. Cytotoxic T lymphocytes and plasma cells
B. Eosinophils and neutrophils
C. Helper T lymphocytes and plasma cells
D. Histiocytes and multinucleated giant cells
E. Lymphocytes and histiocytes
4. Pulmonary conditions such as Löffler syndrome, tropical eosinophilia, allergic bronchopulmonary aspergillosis, and bronchocentric granulomatosis usually result from hypersensitivity reactions to:
A. Allergens of plant origin
B. Bacterial organisms
C. Fungi, parasites, and drugs
D. Nitrogen dioxide (NO2)
E. Viruses
5. An adult patient presents with a chest x-ray picture of bilateral areas of diffuse consolidation. Biopsies of involved areas demonstrate multiple necrotizing granulomas in close proximity to small bronchi. Bronchial spaces are filled with mucus, neutrophils, and eosinophils. No histologic evidence of arteritis is seen. Peripheral eosinophilia is mild, and antineutrophil cytoplasmic antibodies (ANCA) are undetectable. Which of the following is the most likely diagnosis?
A. Allergic bronchopulmonary aspergillosis (ABPA)
B. Allergic granulomatosis (Churg-Strauss syndrome)
C. Bronchiolitis obliterans–organizing pneumonia
D. Bronchocentric granulomatosis
E. Wegener granulomatosis limited to the lungs
6. Which of the following histopathologic findings is considered most characteristic of bronchiolitis obliterans–organizing pneumonia?
A. Hyaline membranes
B. Interstitial fibrosis
C. Intrabronchiolar fibroblastic plugs
D. Macrophages within alveolar spaces
E. Peribronchial granulomas
7. A lymphoma originating from BALT (bronchial-associated lymphoid tissue) is usually:
A. An aggressive high-grade lymphoma
B. Associated with lymphatic tracking
C. Composed of T lymphocytes, similar to lymphocytic interstitial pneumonia (LIP)
D. Not associated with lymphoepithelial lesions
E. Seen in young patients
8. The entity known as lymphomatoid granulomatosis is a/an:
A. Infectious condition due to mycobacteria
B. Leukemic infiltration
C. Malignant lymphoid proliferation
D. Process akin to mycobacterial pseudotumor
E. Reactive lymphoid process
9. A 20-year-old man undergoes surgery for resection of a well-circumscribed mass in the right lung. Histologically, it is composed of spindle cells arranged in fascicles variably admixed with a plasma cell population. The spindle cells react with antibodies to vimentin and actin and are negative for CD68. The plasma cell component is polyclonal as evaluated by light chain immunohistochemistry. The diagnosis most compatible with these features is:
A. Bronchiolitis obliterans–organizing pneumonia
B. Lymphomatoid granulomatosis
C. Mycobacterial pseudotumor
D. Plasma cell granuloma
E. Pulmonary hyalinizing granuloma
10. A 13-year-old child presents with recurrent hemoptysis and iron deficiency anemia. Granular perihilar infiltrates are present on chest x-rays. Which of the following histologic findings supports a diagnosis of idiopathic hemosiderosis instead of Goodpasture syndrome?
A. Absence of IgG deposition along basement membranes
B. Accumulation of hemosiderin-laden macrophages
C. Hyperplasia of alveolar cells
D. Presence of interstitial fibrosis
E. Presence of interstitial lymphocytic infiltration
11. A 35-year-old woman manifests increasingly severe respiratory distress and chest pain. Cardiac catheterization leads to a clinical diagnosis of pulmonary hypertension of unknown origin. In the earliest stages of this condition, an open lung biopsy would reveal predominantly:
A. Fibrin thrombi
B. Intimal hyperplasia
C. Medial thickening
D. Plexogenic lesions
E. Reduplication of elastic lamina
12. The condition known as lymphangiomyomatosis is seen exclusively in:
A. Children
B. Young men
C. Women of childbearing age
D. Postmenopausal women
E. Elderly persons
13. Which of the following pulmonary conditions is due to the accumulation of surfactant apoprotein within alveoli?
A. Alveolar proteinosis
B. Amyloidosis, diffuse alveolar septal type
C. Goodpasture syndrome
D. Idiopathic hemosiderosis
E. Pulmonary alveolar microlithiasis
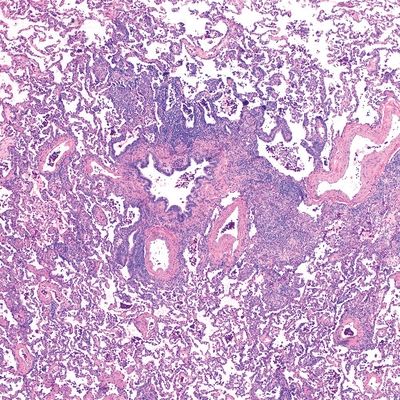
A. Usual interstitial pneumonitis (UIP)
B. Desquamative interstitial pneumonia (DIP)
C. Cryptogenic organizing pneumonia (COP)
D. Diffuse alveolar damage (DAD)
E. Respiratory bronchiolitis (RB)
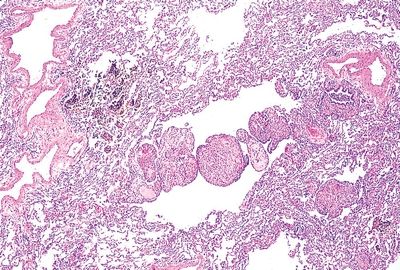
A. Bronchopneumonia
B. Diffuse alveolar damage
C. Desquamative interstitial pneumonitis
D. Extrinsic allergic alveolitis
E. Bronchocentric granulomatosis
A. Desquamative interstitial pneumonia
B. Bronchiocentric granulomatosis
C. IgG4-related disease
D. Respiratory bronchiolitis
E. Lymphangioleiomyomatosis
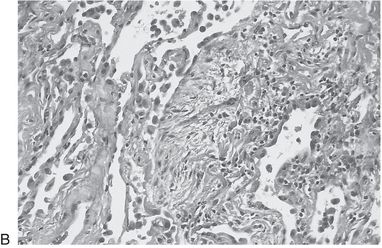
A. Giant cell pneumonia
B. Usual interstitial pneumonia
C. IgG4-related disease
D. Nonspecific interstitial pneumonia
E. Pulmonary Langerhans histiocytosis
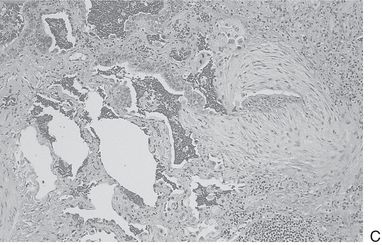
A. Cryptogenic organizing pneumonia
B. Extrinsic allergic alveolitis
C. Nonspecific interstitial pneumonitis
D. IgG4-related disease
E. Bronchocentric granulomatosis
A. Centrilobular emphysema
B. Pulmonary Langerhans cell histiocytosis
C. Lymphangioleiomyomatosis
D. Metastatic leiomyosarcoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree