QUESTION 33.4
A. Autoimmune enteropathy
B. Inflammatory bowel disease
C. Mastocytosis
D. Nonspecific duodenitis
E. Stasis syndrome
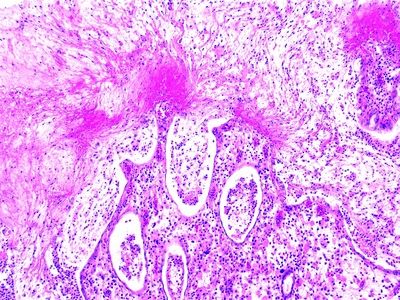
F. Tropical sprue
G. Zollinger-Ellison syndrome
5. A patient with history of common variable immunodeficiency presents with chronic diarrhea, malabsorption, and recurrent Giardia infection. Which of the following findings is likely to be found in a small intestinal biopsy from this patient?
A. Absent Iga-positive plasma cells
B. Infiltration by eosinophils
C. Infiltration by foamy macrophages
D. Lymphangiectasia associated with short broad villi
E. Thick subepithelial collagen band
6. A 35-year-old HIV-negative man presents with malabsorption syndrome and lymphadenopathy. A jejunal biopsy reveals diffuse infiltration of the lamina propria by macrophages whose cytoplasm is filled with PAS-positive granular material, as shown in this photomicrograph. Which of the following is the most likely pathogen in this condition?
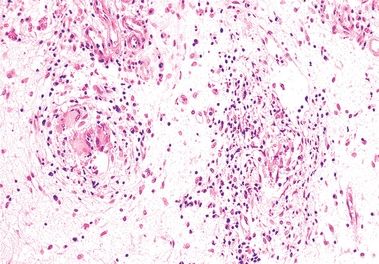
QUESTION 33.6
A. Bartonella henselae
B. Mycobacterium avium-intracellulare
C. Salmonella
D. Tropheryma whipplei
E. Yersinia
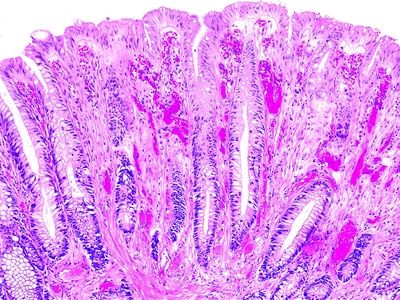
7. A duodenal biopsy from a patient suffering from intermittent diarrhea and malabsorption is shown in this high-power photomicrograph of an H&E-stained section. Which of the following is the most likely diagnosis?
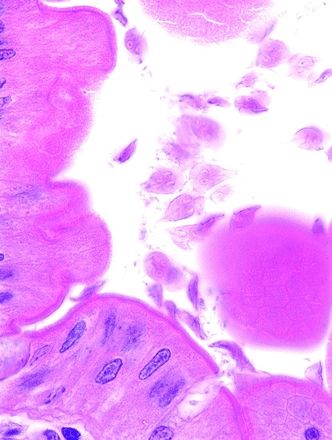
QUESTION 33.7
A. Capillariasis
B. Cryptosporidiosis
C. Giardiasis
D. Microsporidiosis
E. Strongyloidiasis
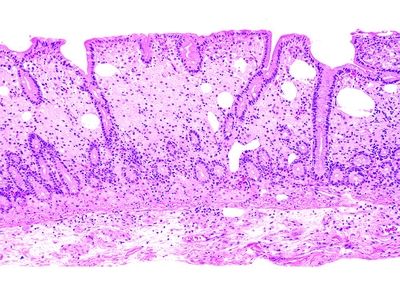
8. This photomicrograph of a colonic biopsy shows histologic changes most consistent with:
QUESTION 33.8
A. Diffuse active colitis
B. Focal active colitis
C. Ischemic colitis
D. Normal colonic mucosa
E. Quiescent ulcerative colitis
9. Which of the following histologic changes indicates the presence of active colitis?
A. Chronic inflammatory infiltrate in the lamina propria
B. Crypt distortion and branching
C. Depletion of mucin in goblet cells
D. Neutrophils in the lamina propria
E. Plasmacytosis in the lower mucosa
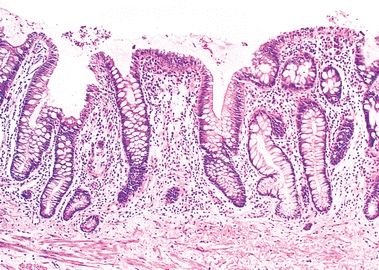
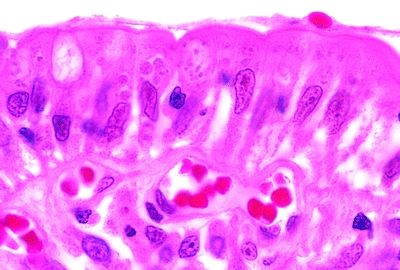
10. A colonic biopsy shows the histologic changes highlighted in this picture, which is from a patient suspected to have inflammatory bowel disease. Does this finding favor a diagnosis of CD?
QUESTION 33.10
A. Yes
B. No
A. Campylobacter species
B. Chlamydia trachomatis
C. Clostridium difficile
D. Yersinia enterocolitica
E. Yersinia pseudotuberculosis
12. A 59-year-old woman presents with intractable watery diarrhea of unknown etiology. All of the clinical and radiologic investigations reveal no abnormalities. Endoscopically, the colonic mucosa appears unremarkable. A colon biopsy shows increased inflammatory cells in the lamina propria and a thick hyaline membrane underneath the epithelial layer. Which of the following is the most likely diagnosis?
A. Bacterial colitis
B. Collagenous colitis
C. Eosinophilic colitis
D. Lymphocytic colitis
E. Pseudomembranous colitis
13. A 32-year-old male presents with constipation and rectal bleeding. Clinical differential diagnosis includes Crohn disease, villous adenoma, and adenocarcinoma. Rectal biopsies reveal replacement of the lamina propria with fibrosis and smooth muscle, as shown in this picture. These features are most consistent with:
QUESTION 33.13
A. Colorectal mucosal prolapse
B. Mucinous adenocarcinoma
C. Pneumatosis cystoides intestinalis
D. Ulcerative colitis
E. Villous adenoma
14. A patient with AIDS develops intractable watery diarrhea. A jejunal biopsy shows round faintly basophilic 3-μm bodies attached to the luminal surface, as illustrated by this high-power picture. Which of the following mucosal changes would be expected?
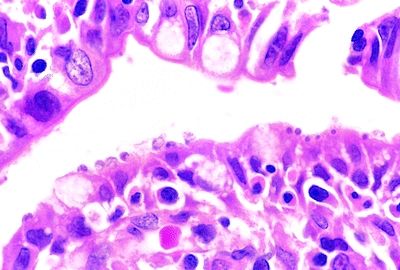
QUESTION 33.14
A. Crypt abscesses
B. Eosinophilic infiltration
C. Extensive lymphocytic infiltration
D. Granulomas
E. Minimal nonspecific changes
15. An AIDS patient with intractable diarrhea undergoes a GI biopsy. Clusters of small dotlike structures are seen in a paranuclear location within epithelial cells of intestinal villi, as shown in this picture. These are gram positive but AFB negative. The most likely pathogen is:
QUESTION 33.15
A. Cryptosporidia
B. Cytomegalovirus
C. Giardia lamblia
D. Microsporidia
E. Spirochetes
16. Indeterminate colitis refers to a form of colitis that:
A. Follows a chronic indolent course
B. Has histologic features inconclusive for UC or CD
C. Is synonymous of colonic inflammatory bowel disease, unclassified
D. Represents approximately 50% of all cases
E. All of the above
17. A colonic biopsy from an area of stricture located in the splenic flexure is examined histologically. Which of the following microscopic changes favors a diagnosis of ischemic bowel disease over inflammatory bowel disease?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree