Chapter 2 Neurophysiology
I. Overview
B. It consists of several complex components that function in an organized fashion at extremely high speeds.
C. The human brain is a network of more than 100 billion nerve cells that, through specific pathways, communicate with each other and with various motor and sensory systems.
D. Ultimately, these networks allow one to think, move, feel, experience, and manipulate one’s environment.
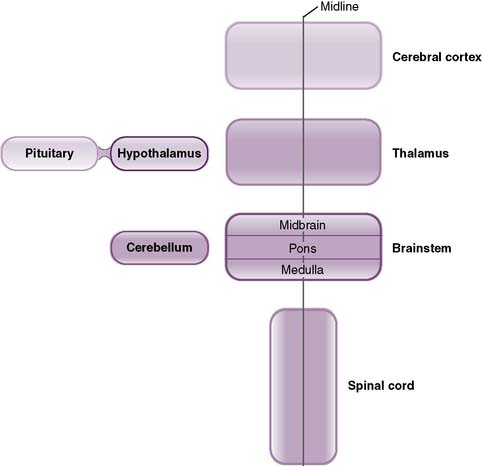
II. Organization and Functional Anatomy of the Nervous System
• The nervous system is anatomically subdivided into the central nervous system (CNS) and peripheral nervous system (PNS).
B. Peripheral nervous system (PNS)
1. Comprises the peripheral nerves originating from the brainstem and spinal cord (cranial and spinal nerves, respectively), as well as specialized clusters of neurons referred to as ganglia
C. The somatic nervous system
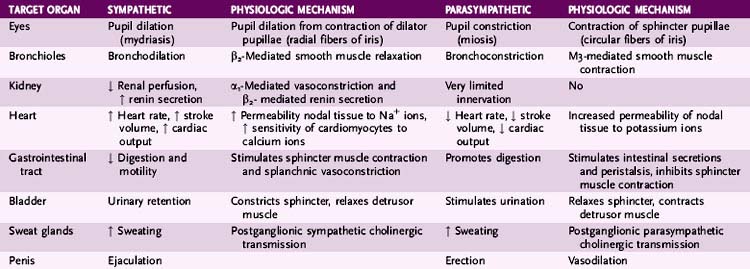
D. The autonomic nervous system (ANS)
1. This controls all involuntary actions (e.g., reflexes, respiration) by regulating functioning of viscera, smooth muscle, and exocrine and endocrine glands.
2. It comprises sensory and motor neurons running between the brain and various internal organs such as the heart, lungs, viscera, and endocrine and exocrine glands.
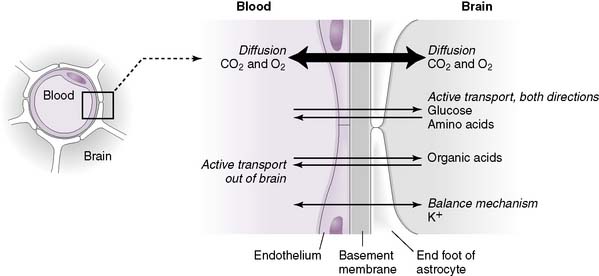
E. Protection of the brain
• This is ensured by two separate systems, the blood-brain and blood-CSF barriers.
1. Blood-brain barrier (BBB) (Fig. 2-2)
• Composed of endothelial cells packed tightly together to form tight junctions that prevent passage of most molecules
• An underlying basement membrane and specialized glial cells (astrocytes), which project processes (pedicels) that attach to the walls of the capillary, reinforce this barrier.
• Very few substances can cross the BBB into brain tissue:
b. Glucose (the primary energy source of the brain) and amino acids require carrier-mediated transport.
c. Nonpolar lipid-soluble substances (e.g., free unconjugated bilirubin) cross more readily than polar water-soluble ones.
2. Blood-CSF barrier
• Cerebrospinal fluid (CSF) is a clear, colorless fluid that normally contains none or few cells, a small amount of protein, and a moderate amount of glucose.
• The blood-CSF barrier is composed of epithelial cells of the highly vascular choroid plexus located within the ventricles. These cells are connected through tight junctions.
• The choroid plexus produces CSF. The tight junctions between the cells serve to selectively allow substances access to the CSF.
III. The Autonomic Nervous System
A. Overview
1. The primary function of the autonomic nervous system (ANS) is to control and regulate the visceral functions of the body (e.g., heart rate, glandular secretions).
B. Organization
3. These entities interpret the signal and reflexively send signals back to the visceral organ to control its activity.
4. The efferent autonomic signals are transmitted to the various organs of the body through two major subdivisions, the sympathetic nervous system and the parasympathetic nervous system.
5. A third subdivision, the enteric nervous system (ENS), controls activity of the gastrointestinal tract; however, activity of the ENS can be greatly influenced by both arms of the autonomic nervous system.
6. An example of a visceral reflex is the response to cold.
• Cold receptors on the skin transmit signals to the hypothalamus, which in turn causes several reflexive adjustments through autonomic efferents, including:
a. Stimulating muscle contraction (shivering), which increases the rate of body heat production, and
a. The sympathetic division: “fight or flight” system
• The sympathetic nervous system is called the fight-or-flight system because it is most active in times of stress, fear, or excitement.
• For example, at the exact moment a sudden fear is made conscious, the sympathetic nervous system takes over.
• Bodily changes include a racing heart, dilated pupils, sweating, and skeletal muscle prepared for running.
• While the body is poising itself for escape, it recruits additional energy from systems that are not vital to surviving the encounter.
• For instance, sympathetic output shuts down gut and genitourinary function, to allow all efforts to be put into the escape (or “fight”).
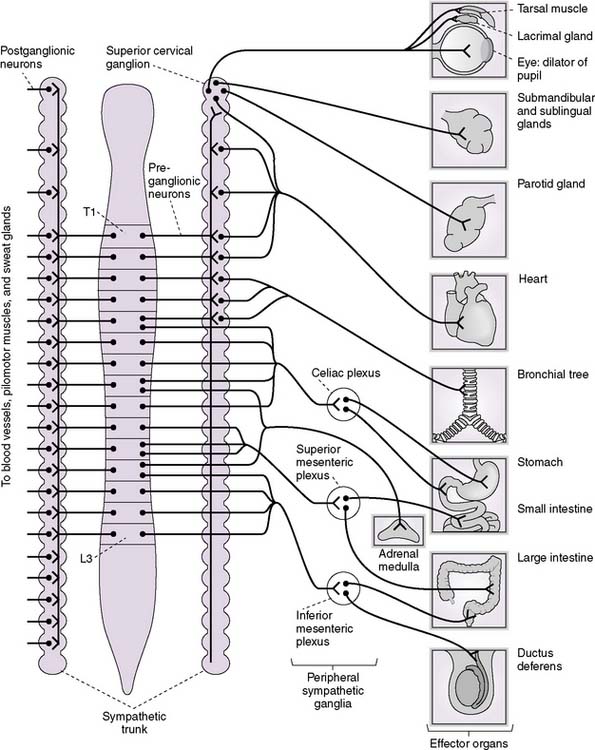
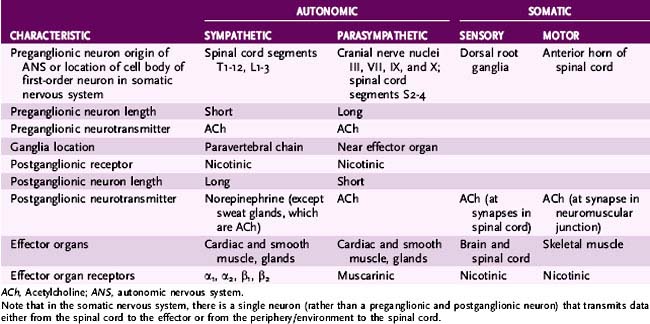
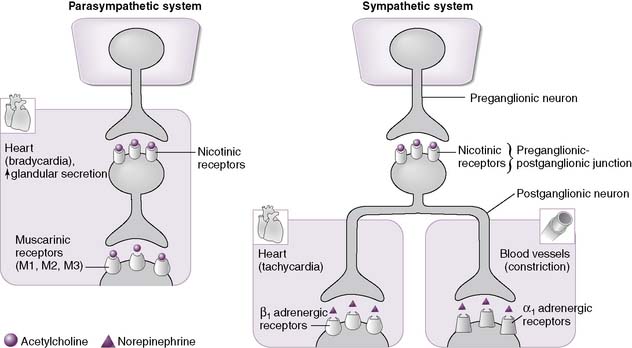
b. Functional anatomy (Fig. 2-3)
• Sympathetic nerves are different from skeletal motor nerves in that each sympathetic pathway is composed of two neurons, a preganglionic neuron and a postganglionic neuron (Table 2-2).
• The preganglionic nerve fibers originate in the intermediolateral horn of the spinal cord between cord segments T1 and L2.
• They pass through the anterior roots of the cord through the white rami and do one of three things:
(1) Synapse in the paravertebral sympathetic chains of ganglia that lie to the two sides of the vertebral column or in the two prevertebral ganglia (the celiac and hypogastric ganglia)
• The adrenal medulla is a specialized ganglion of the sympathetic division that synthesizes and secretes epinephrine and norepinephrine.
• Preganglionic sympathetic fibers pass, without synapsing, from the intermediolateral horn cells of the spinal cord, through the sympathetic chains and the splanchnic nerves, and finally to the adrenal medulla, where they synapse on the chromaffin cells.
• Chromaffin cells are modified neuronal cells that secrete epinephrine (80%) and norepinephrine (20%) into the bloodstream.
c. The parasympathetic division: “rest and digest” system
• The parasympathetic nervous system is called the rest-and-digest system because it is most active in times of rest, relaxation, and rejuvenation.
• Simultaneously, those organs activated in times of stress, such as skeletal and cardiac muscle, are relaxed.
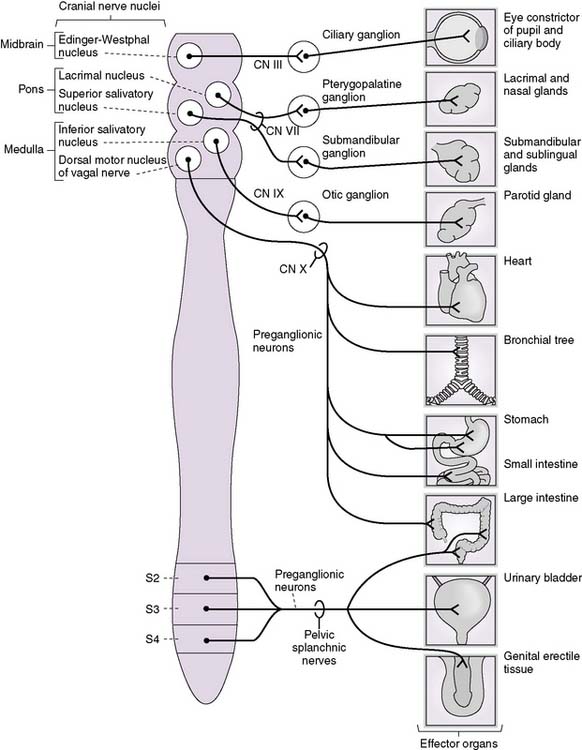
d. Functional anatomy (Fig. 2-4)
• As in the sympathetic nervous system, parasympathetic pathways are composed of preganglionic and postganglionic neurons.
• The preganglionic nerve fibers originate in cranial nerve nuclei in the brainstem and in the intermediolateral horn of the spinal cord between cord segments S2 and S4 (craniosacral origin).
e. The enteric nervous system
• This is contained entirely within the gut wall and is composed of the submucosal (Meissner) plexus and the myenteric (Auerbach) plexus.
• Stimulation of the submucosal plexus promotes digestion, largely by stimulating secretions from the mucosal epithelium.
• Stimulation of the myenteric plexus increases intestinal motility by stimulating peristalsis and inhibiting contraction of sphincter muscles throughout the intestinal tract.
• The ANS can powerfully influence functioning of the enteric nervous system:
(1) The sympathetic nervous system inhibits peristalsis and increases sphincter tone, thereby inhibiting digestion.
C. Neurotransmitters of the ANS
1. Acetylcholine (ACh)
• Neurotransmitter used in the peripheral nervous system, central nervous system, and autonomic nervous system
5. Nitric oxide (NO)
• Released by vascular endothelial cells (endothelium-derived relaxation factor [EDRF]); plays an important role in blood pressure regulation by promoting vascular smooth muscle relaxation
D. Neurotransmitter receptor types
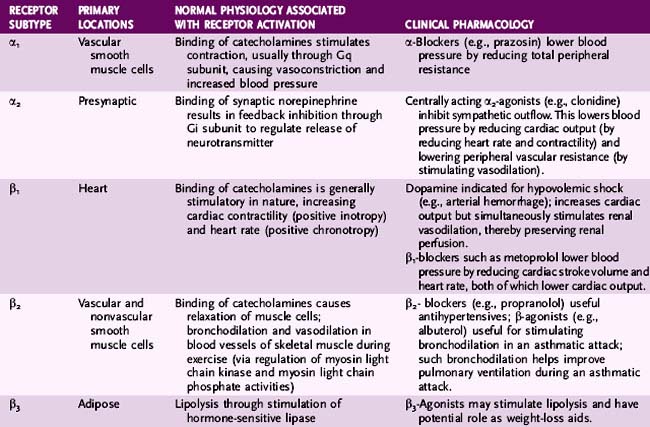
1. Adrenergic receptors (Table 2-3)
• NE released from sympathetic neurons binds to these receptors, as do adrenal catecholamines; this is why the sympathetic nervous system is sometimes referred to as the sympathoadrenal system.
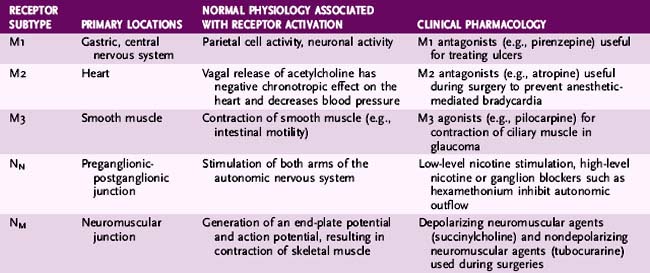
2. Cholinergic receptors (Table 2-4; Fig. 2-5)
• Location
a. Parasympathetic effector organs as well as a few sympathetic effector organs such as sweat glands
IV. Control of Movement
A. Overview
1. The control of movement is complex and involves coordinated functioning of multiple hierarchical structures within the CNS such as the motor cortices, basal ganglia, motor thalamus, cerebellum, upper and lower motor neurons, and the sensory system.
2. Planning, initiation, and modification of movement are dependent on a proper functioning of the complicated interplay between a CNS stimulus, a musculoskeletal effector, and a proprioceptive sensor.
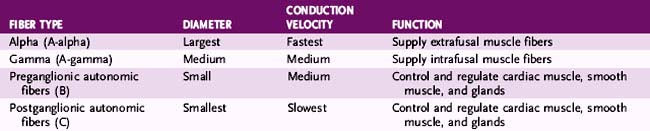
B. Motor neurons
1. Muscles can be supplied by two types of motor neurons: alpha motor neurons and gamma motor neurons.
2. Alpha motor neurons are large, myelinated axons that innervate extrafusal muscle fibers, contraction of which causes movement at a joint.
3. Gamma motor neurons are small, myelinated axons that innervate intrafusal muscle fibers, contraction of which do not result in movement but does play an important role in muscle tone and joint proprioception.
C. Control of voluntary movement
D. Role of the cerebral cortex in movement
1. The motor cortex of the frontal lobe is responsible for formation and execution of motor plans for voluntary movements.
4. Descending corticobulbar and corticospinal fibers travel through the internal capsule en route to their target nuclei in the brainstem and spinal cord, respectively.
5. Stimulation of the primary motor cortex results in discrete movements of contralateral muscles (e.g., moving a finger).
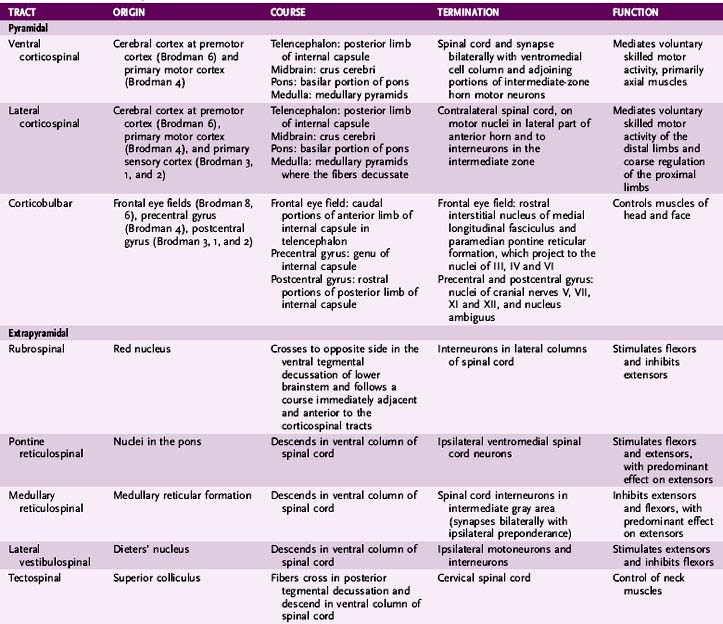
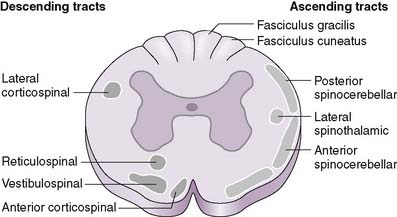
E. Role of spinal cord tracts in movement (Table 2-6)
1. Important in rhythmic movements such as chewing and swallowing, as well as reflexive movements such as withdrawal reflexes
2. Tracts can be divided anatomically into two categories, pyramidal and extrapyramidal.
• The pyramidal tracts originate in the cerebral cortex, decussate in the pyramids of the caudal medulla, and terminate directly on motor neurons in the brainstem and spinal cord.
• The extrapyramidal tracts originate in the brainstem (pons and medulla) and terminate on neurons adjacent to the ventral horn cells of the spinal cord.
a. These tracts indirectly modulate activity of the ventral horn cells of the spinal cord and play an important role in reflexes, postural control, and locomotion.
3. Medial descending system (MDS)
• Overview
a. The tracts of the MDS terminate in the ventromedial portion of the anterior horn (hence their name).
• Vestibulospinal tracts
a. Arise from the vestibular nuclei of the medulla and travel in the anterior funiculus of the spinal cord
c. The lateral vestibulospinal tract stimulates extensor motor neurons supplying muscles of the trunk and legs, thereby stabilizing posture.
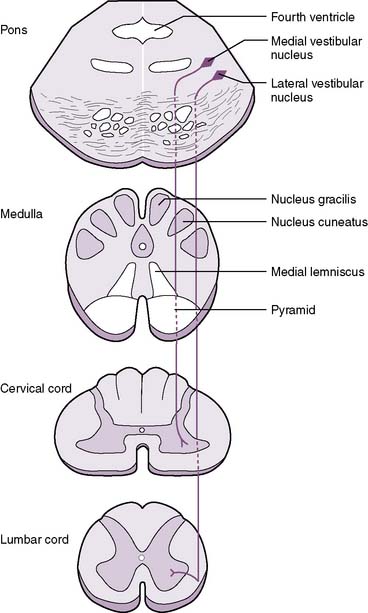
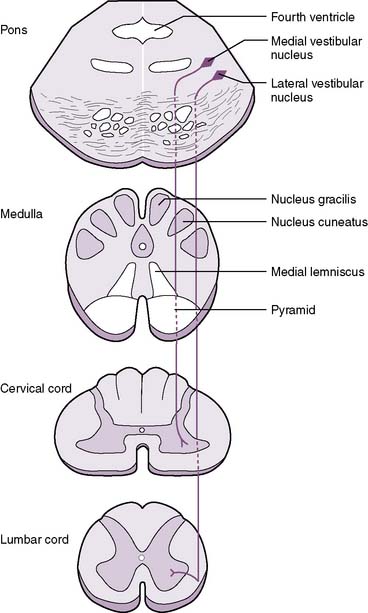
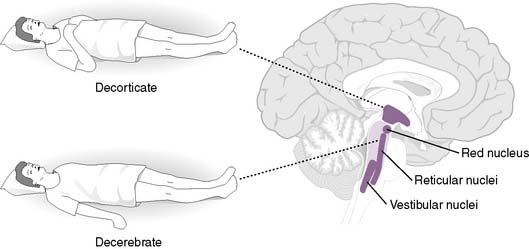
2-7 Pathway of the vestibulospinal tracts.
(From Crossman A, Neary D: Neuroanatomy: An Illustrated Colour Text, 3rd ed. London, Churchill Livingstone, 2006, Fig. 8-20.)
• Reticulospinal tracts
c. The pontine reticulospinal tract descends in the anterior funiculus of the spinal cord and acts in concert with the vestibulospinal tracts, being excitatory to extensor antigravity muscles.
d. The medullary reticulospinal tract descends in the lateral funiculus of the spinal cord and is inhibitory to extensor antigravity muscles.
4. Lateral corticospinal tract
• After decussating in the caudal medulla, these tracts descend in the lateral funiculus of the spinal cord and synapse on alpha motor neurons, controlling distal limb muscles.
5. Relationship of upper and lower motor neurons




• The term upper motor neurons encompasses motor neurons originating (primarily) from the motor cortices that descend to synapse on lower motor neurons located in the brainstem and spinal cord.
• The term lower motor neurons encompasses motor neurons originating in the brainstem and spinal cord and their path from their origin to the muscle they innervate.
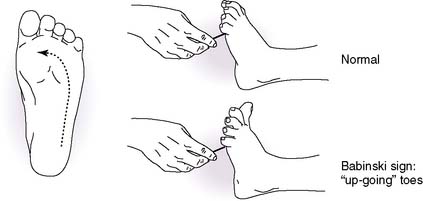
• A lesion therefore causes disinhibition of lower motor neurons, resulting in spasticity and hyperreflexia (Table 2-7).
< div class='tao-gold-member'>
TABLE 2-7 Lesions of Upper and Lower Motor Neurons
| Parameter | Upper Motor Neuron Lesion | Lower Motor Neuron Lesion |
|---|---|---|
| Cause | Lesion of cortex or corticospinal tract | Damage to lower motor neurons |
| Examples | Amyotrophic lateral sclerosis | Poliomyelitis, trauma, Guillain-Barré syndrome |
| Clinical Signs | ||
| Babinski sign | Present | Absent |
| Paralysis | Spastic | Flaccid |
| Muscle wasting | Absent or minimal | Present |
| Fasciculations | Absent | Present |
| Hyperreflexia or hyporeflexia | Hyperreflexia, clonus | Hyporeflexia |
| Deep tendon reflexes | Hyperactive | Absent |
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree