Mycobacterial Infection
Tariq Muzzafar, MBBS
Key Facts
Clinical Issues
High index of suspicion essential for diagnosis
Definitive diagnosis by histology and culture of LN
Molecular methods enable quicker identification of organism
FNA is as useful as excisional LN biopsy in HIV(±) patients
Microscopic Pathology
Granulomas, classically with necrotic center (caseation)
Concentric layers of epithelioid cells, Langhans giant cells, lymphocytes, and plasma cells
Fibrosis, hyalinization, calcification present in healing phase
In LN biopsy specimen, AFB identified by Ziehl-Neelsen, Kinyoun, Fite-Faraco stains
Auramine-rhodamine stain with fluorescent microscopy more sensitive for detection
Top Differential Diagnoses
M. avium-intracellulare lymphadenitis
Histoplasma lymphadenitis
Kikuchi-Fujimoto lymphadenitis
Cat scratch lymphadenitis
Sarcoidosis lymphadenopathy
Reporting Considerations
Suspected or confirmed cases of TB should be reported to local public health department
Identify adult source case and contacts for follow-up
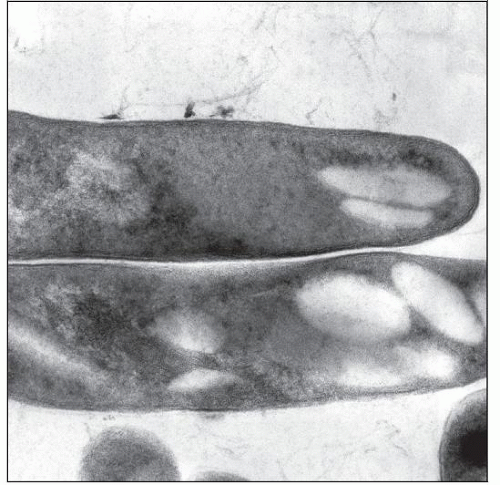
 Scanning electron micrograph demonstrates M. tuberculosis; the bacterium ranges from 2-4 µm long and 0.2-0.5 µm wide. (Courtesy J. Carr, CDC Public Health Image Library, #9997. |
TERMINOLOGY
Abbreviations
Acid-fast bacilli (AFB)
Tuberculosis (TB)
Definitions
Lymphadenitis caused by infection with Mycobacterium tuberculosis
ETIOLOGY/PATHOGENESIS
Infectious Agents
M. tuberculosis
Immunocompetent Patients
Reactivation of disease at site seeded during primary infection by hematogenous route
As compared to adults, young children more commonly have
Disseminated disease
Severe illness even with low bacterial loads
Deficient immune responses implicated
Infection of tonsils, adenoids, and Waldeyer ring can occur
Abdominal involvement may occur via ingestion of milk or sputum infected with M. tuberculosis
Immunocompromised Patients
Reactivation of latent infection
Part of generalized infection, miliary dissemination
Greater mycobacterial load than immunocompetent patients
Laryngeal involvement very infectious: Special precautions needed
CLINICAL ISSUES
Epidemiology
Incidence
Childhood tuberculosis represents
15-40% of all cases in low- and middle-income countries
2-7% of all cases in industrialized countries
Associated with lower socioeconomic status and overcrowding
Represents ˜ 40% of peripheral lymphadenopathy in developing world
Prevalence of TB lymphadenitis in children ≤ 14 years in rural India: 4.4/1,000
In industrialized countries, most cases occur in immigrants and travelers to endemic areas
Immigrant populations mostly originate from Southeast Asia and Africa
Lymphadenitis is most common form of extrapulmonary tuberculosis
Risk of infection higher in following settings
Lower socioeconomic status, overcrowding leading to close contact with index case
Orphanages and refugee camps
Immunosuppression: HIV (most important), malignancies, chemotherapy, corticosteroids
Age
Incidence
Decreases from birth to 8 years of age
Increases again in late adolescence and early adult life
Gender
M:F = 1:2
Ethnicity
Asian Pacific Islanders more susceptible
Presentation
Characteristically, multiple lymph nodes (LNs) involved
Usually unilateral; can be bilateral
Superficial LN involvement
Most common form of extrapulmonary TB in children
Anterior and posterior cervical (most common)
Supraclavicular, submandibular, preauricular, submental also involved
Classified as nonsevere disease if
No spread to or compression of adjacent neural, vascular, lymphatic, or bony tissues
Isolated sinus or fistula formation from node present, and no involvement of other organs
Inguinal, epitrochlear, axillary involvement rare
Isolated intraabdominal LNs can be involved
Periportal, peripancreatic, and mesenteric
Classified as nonsevere if only enlarged abdominal nodes present
Due to hematogenous or retrograde lymphatic spread from lung, or ingestion of sputum or milk infected with M. tuberculosis
Generalized lymphadenopathy and hepatosplenomegaly may occur
Due to lymphohematogenous spread
Typical course
Lymph nodes usually enlarge gradually in the early stages
Systemic signs and symptoms absent
Low-grade fever may be present
Without treatment, caseation necrosis, rupture of capsule, involvement of adjacent LNs and overlying skin, sinus tract
Occasional cases
Lymphadenitis acute with rapid enlargement
High fever, tenderness, fluctuation, overlying cellulitis
Parabronchial and paratracheal involvement can lead to airway compromise
LN on physical examination
Firm, rubbery, discrete, and nontender; may be matted
Nodes may feel fixed to underlying or overlying tissues
May be swollen and tender due to secondary bacterial infection
Laboratory Tests
Tuberculin skin test (TST)
May be negative with culture documented disease in
10% of immunocompetent children; may become positive subsequently
Disseminated disease
HIV-positive patients
Interferon-Y release assays (IGRA)
Measure in vitro T-cell interferon-Y release in response to 2 unique antigens
Sensitivity similar to TST; specificity higher
Negative in prior Bacillus Calmette-Guérin vaccination and in sensitization to nontuberculous mycobacteria
2 widely studied tests
Enzyme-linked immunospot (ELISpot) (T-SPOT.TB; Oxford Immunotec; Oxford, UK)
Enzyme-linked immunosorbent assay (ELISA) (QuantiFERON-TB Gold; Cellestis; Chadstone, VIC; Australia)
TST and IGRA cannot distinguish between infection, active disease, and past disease
IGRA not recommended to replace TST in low- and middle-income countries
Direct staining
Carbolfuchsin stains (Ziehl-Neelsen stain; Kinyoun stain) highlight AFB
AFB are bright red against blue or green background, depending on counterstain
Must be scanned under oil-immersion
Time consuming due to limited size of field viewed at 1 time
< 2% of children below 10 years positive in newly diagnosed TB
Negative smears do not rule out diagnosis
Fluorochrome stain (auramine O, ± rhodamine)
Scanning is quicker since slides can be scanned at 25x objective
Confirmation may require 40x objective
Bacteria bright yellow (auramine) or orange-red (rhodamine) against dark background
Microbiological culture
General comments
Only ˜ 30% of children confirmed bacteriologically
5% of children < 10 years positive in newly diagnosed TB
Löwenstein-Jensen (LJ) medium
Less sensitive
Recommended only for chromogenic studies and biochemical tests
Middlebrook 7H10 and 7H11 agar medium used for isolation and susceptibility testing
Automated radiometric detection systems: BACTEC 460 (BD Diagnostic Systems; Sparks, MD; USA)
Automated nonradiometric detection systems
MGIT 960 (BD Diagnostic Systems)
MB/BacT System (BioMerieux; Durham, NC; USA)
BACTEC MYCO/F lytic blood culture bottle (BD Diagnostic Systems)
ESP Culture System II (TREK Diagnostic Systems, Inc.; Cleveland, OH; USA)
Gas-liquid and high-performance liquid chromatography
Useful in culture confirmation
Molecular diagnosis (nucleic acid amplification)
Quicker and accurate identification compared to traditional methods; specificity > 97%
Negative result does not rule out diagnosis
AFB microscopy negative cases
Real-time polymerase chain reaction assay useful
Xpert-MTB/RIF (Cepheid, Sunnyvale, California, USA) assay recommended by WHO
Detects 81-bp-core region of RNA-polymerase β-subunit gene flanked by M. tuberculosis-specific DNA sequences
Can test for rifampicin resistance simultaneously
Initial diagnostic test in cases with suspected multidrug-resistant (MDR) TB or HIV-associated TB
AFB microscopy positive cases
Molecular line probe assays preferred
GenoType-MTBDRplus (Hain Lifesciences, Nehren, Germany) assay recommended by WHO
Can test for rifampin and isoniazid resistance simultaneously
Treatment
Surgical approaches
Indications: Failure of antimicrobial chemotherapy, pressure effect
Excisional biopsy preferred since incisional biopsy may result in sinus tract formation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree