Multicentric Castleman Disease
Pei Lin, MD
Key Facts
Terminology
Systemic lymphoproliferative disease occurs in patients with immunodeficiency or immune dysregulation and is usually associated with human herpesvirus type 8 (HHV8) infection
Etiology/Pathogenesis
HHV8 (KSHV) infection important
Virus has pleiotropic effects, including encoding homolog of IL-6
Immunodeficiency (e.g., HIV) plays important role
POEMS syndrome is commonly associated with MCD
Clinical Issues
Lymphadenopathy constant; any lymph node group
B symptoms in over 95% of patients
Splenomegaly in ˜ 75%; hepatomegaly ˜ 50%
Patients with MCD have increased frequency of other neoplasms
Plasmablastic lymphoma, Kaposi sarcoma, primary effusion lymphoma
Microscopic Pathology
Sheets of plasma cells in interfollicular zones
Extensive vascular proliferation
Blurring of boundary between mantle zone and interfollicular area
HHV8(+) cells are usually localized in mantle zones of follicles
Plasmablasts or immunoblasts
Ancillary Tests
LANA1 antibody recognizes HHV8(+) cells
Monoclonal Ig gene rearrangements
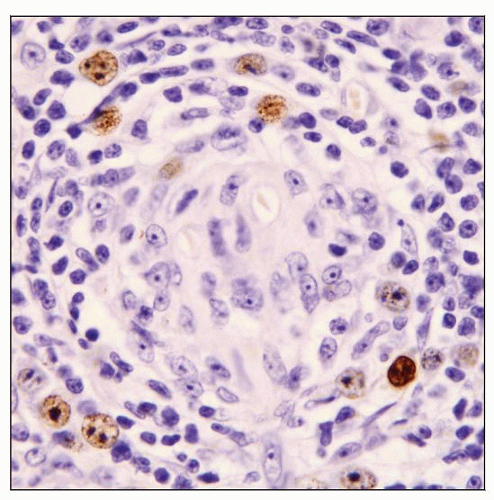
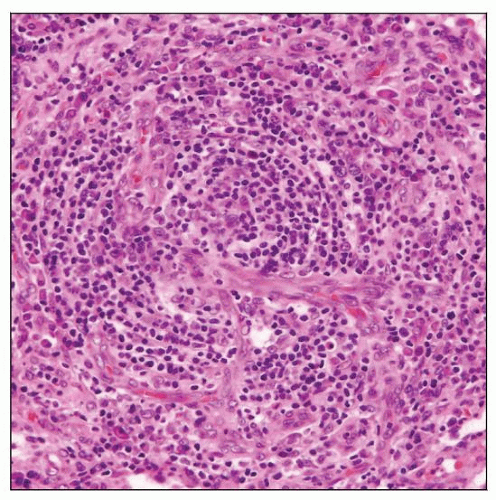 Lymph node involved by multicentric Castleman disease, HHV8(+) in an HIV(+) patient. Scattered hyaline-vascular follicles are present. |
TERMINOLOGY
Abbreviations
Multicentric Castleman disease (MCD)
Synonyms
Angiofollicular lymph node hyperplasia
Angiomatous lymphoid hamartoma
Giant lymph node hyperplasia
Definitions
Systemic lymphoproliferative disease that occurs in patients with immunodeficiency or immune dysregulation
Usually associated with human herpesvirus type 8 (HHV8) infection
ETIOLOGY/PATHOGENESIS
Infectious Agents
HHV8
a.k.a. Kaposi sarcoma herpesvirus (KSHV)
γ-herpesvirus with estimated seroprevalence of 25% in USA
Virus load in peripheral blood mononuclear cells correlates with disease severity
HHV8 encodes for homolog of human interleukin-6 (IL-6)
Viral IL-6 stimulates human IL-6 induced cellular pathways
Human IL-6 is B-cell growth factor that regulates differentiation of B lymphocytes to plasma cells
Regulates T-cell function and induces C-reactive protein (CRP) production by hepatocytes
Endogenous pyrogen
B cells derived form MCD overexpress IL-6 receptor CD126
Cells within lymph nodes express high levels of IL-6
This suggests paracrine and autocrine mechanisms involved in pathophysiology of MCD
Immunodeficiency or immune dysregulation/dysfunction
HIV infection
Most HIV(+) patients with MCD are HHV8(+)
Wiskott-Aldrich syndrome
Autoimmune diseases or phenomena
Associated with autoantibody-induced paraneoplastic pemphigus
Associated with myasthenia gravis
POEMS syndrome
Peripheral neuropathy, organomegaly, endocrinopathy, monoclonal M protein, skin lesions
Serologic evidence of HHV8(+) in many patients
Poorly understood syndrome associated with immune dysregulation
CLINICAL ISSUES
Epidemiology
Incidence
MCD occurs most often in HIV(+) patients with AIDS
Therefore, incidence correlates with that of AIDS
Age
Broad age range
Gender
More often in males (correlates with AIDS)
Presentation
Lymphadenopathy is constant finding; any lymph node group can be involved
Peripheral, abdominal, or mediastinal lymphadenopathy
B-type symptoms in over 95% of patients
Fever, night sweats, weight loss
Splenomegaly in ˜ 75%, hepatomegaly in ˜ 50%
Edema, body cavity effusions, and skin rash in subset of patients
Central nervous system abnormalities in small patient subset
Higher risk for coexistent chronic infections
Epstein-Barr virus, hepatitis C, CMV
Laboratory Tests
Abnormal serum findings
Elevated serum IL-6 levels during symptomatic episodes
Elevated erythrocyte sedimentation rate
Elevated lactate dehydrogenase (LDH) levels
Hypergammaglobulinemia
Hematologic
Cytopenias
Anemia &/or thrombocytopenia
Treatment
Chemotherapy and steroids have been used for patients with MCD
Not very effective for MCD patients who are HIV(+) or have POEMS syndrome
Prognosis
Poor in patients with POEMS syndrome or HIV infection
Patients usually die within a few months of diagnosis
Frequently Associated Neoplasms
Plasmablastic lymphoma (PBL)
HHV8(+) patients; often also EBV(+)
PBL usually involves lymph nodes and spleen; leukemia rare
Can affect HIV(-) patients in HHV8 endemic regions (Africa and Mediterranean countries)
Kaposi sarcoma
More common in HIV(+) patients
Primary effusion lymphoma (PEL)
Occurs in HHV8(+) patients
Usually coinfected with EBV
Glomeruloid hemangioma
Distinctive skin tumor highly suggestive of POEMS syndrome
Increased frequency of classical Hodgkin lymphoma (HL), diffuse large B-cell lymphoma, mantle cell lymphoma, and peripheral T-cell lymphoma
Mixed cellularity is most common type of classical HL
IMAGE FINDINGS
Radiographic Findings
Lymphadenopathy and hepatosplenomegaly
CT scan: Lesions enhance with IV contrast
PET scan: ˜ 50-60% of lesions have increased FDG uptake
Radiographic findings are not specific
Biopsy required for diagnosis
MICROSCOPIC PATHOLOGY
Histologic Features
Lymph nodes
Most MCD cases have features that fit best as plasma cell variant
Hyaline-vascular follicles are also usually present
Others in past have designated these cases as mixed or transitional type of CD
These changes are part of spectrum of plasma cell (PC) variant
Sheets of polytypic plasma cells in interfollicular regions
Extensive vascular proliferation
Some features of HHV8(+) MCD differ from HHV8(-) plasma cell variant
Greater degree of lymphocyte depletion
Particularly in HIV(+) patients
Blurred border between mantle zones and surrounding interfollicular areas
Plasma cells in MCD can be immature and atypical (plasmablasts)
HHV8(+) cells can be small or large with features of immunoblasts or plasmablasts
Usually located in mantle zones
These cells can form small nodules or “microlymphomas”
Observed in subset of cases
During early stage of disease, plasma cells are polytypic or monotypic
During later stage of disease, plasma cells are monotypic
Usually express monotypic Igλ
HHV8(+) cases with distinctive plasmablasts have been called “plasmablastic variant of CD”
Bone marrow involvement by MCD
Bland plasmacytosis is common
Can mimic plasma cell myeloma
HHV8(+) cells can be identified in bone marrow
Cytologic Features
MCD
Touch imprints and smears show plasma cells, plasmablasts, and lymphocytes
MCD with PBL
Monotonous proliferation of plasmablasts
HHV8(+) immunohistochemistry can be performed on smears/imprints
ANCILLARY TESTS
Immunohistochemistry
Can detect HHV8(+) cells using LANA1 antibody
Latency associated nuclear antigen (LANA)
HHV8(+) cells can be small lymphocytes, immunoblasts, or plasmablasts
Plasmablasts are usually polytypic but can be monotypic; IgM(+)
In subset of cases, follicular dendritic cells (FDRCs) are HHV8(+)
Plasma cells are usually polytypic but can be monotypic
Interfollicular areas show T cells without aberrancy
Follicles show B cells and increased CD21(+) FDRCs
Molecular Genetics
Monoclonal Ig gene rearrangements in subset of cases of MCD
Most often in EBV(+) or HIV(+) cases, suggesting HHV8(+) MCD
Prognostic significance is unclear as overall prognosis is poor
Supports concept that HHV8(+) MCD is lymphoproliferative disorder
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree