Mucinous (Colloid) Carcinoma
Key Facts
Terminology
Mucinous carcinoma (MC)
Special histologic type of invasive carcinoma with distinctive features
Characterized by abundant extracellular pools of stromal mucin product
Clinical Issues
Uncommon; accounts for 1-7% of all invasive mammary carcinomas
Higher prevalence in older age (mean age: 65.8 years)
Commonly presents as palpable mass or circumscribed/lobulated mass on mammogram
Pure MC is associated with favorable prognosis
10-year survival in excess of 80%
Pure MCs have better prognosis than mixed tumors (carcinomas with only focal mucin production)
Macroscopic Features
Soft glistening cut surface, gelatinous appearance
Microscopic Pathology
Hallmark of MC is extracellular mucin production
Detached tumor cells floating in pools of mucin
> 90% mucinous histology (frequently, entire tumor is mucinous)
Tumor cells typically show low histologic grade
Ancillary Tests
Most MCs show expression of ER and PR
HER2 and EGFR overexpression is very uncommon
Some MCs can show neuroendocrine differentiation
TERMINOLOGY
Abbreviations
Mucinous carcinoma (MC)
Synonyms
Colloid carcinoma
Older terms: Mucoid or gelatinous carcinoma
Definitions
Special histologic type of invasive carcinoma with distinctive features
Tumors are characterized by abundant extracellular pools of stromal mucin product
Type A MC is paucicellular and type B MC is more cellular
ETIOLOGY/PATHOGENESIS
Mucin Expression in MC: MUC Genes
Among family of MUC genes, MC expresses predominantly MUC2 and MUC6
MUC2 and MUC6, known as gel-forming mucins, are secreted into stroma that surrounds malignant epithelial cells
MUC2 and MUC6 may serve as barrier to spread of tumor cells
May help to explain indolent clinical behavior
Extracellular mucins may also increase cytotoxic T-lymphocyte activity
Gene Expression Profiling
MC and neuroendocrine breast carcinoma (NEBC) are more similar to each other than to carcinoma of no special type
These cancers fall within luminal type A group
Type B MC and NEBC have essentially identical expression profiles
This includes type B MC with and without expression of neuroendocrine markers by IHC
CLINICAL ISSUES
Epidemiology
Incidence
Uncommon tumor that accounts for 1-7% of all invasive mammary carcinomas
Prevalence is age-related : < 1% in women under 35, but 7% in women older than 75
Age
MC tends to show older mean age at diagnosis (65.8 years)
Presentation
Most common presentation is as a palpable mass
Smaller cancers may be identified as circumscribed or lobulated mass lesions on mammography
Prognosis
Pure MC is associated with favorable prognosis
10-year survival in excess of 80%
Patients typically have lower incidence of axillary lymph node metastasis compared with no special type carcinomas (12% of cases)
Axillary nodal involvement is the most important prognostic factor for these patients
Pure MC (> 90% mucinous histology) has better prognosis than mixed tumors (carcinomas with only focal mucin production)
IMAGE FINDINGS
Mammographic Findings
Round, oval, or lobulated density
Portion of margin may be indistinct
Irregular shape and spiculated margin may be seen in mixed tumors
MACROSCOPIC FEATURES
General Features
Pure MC are well circumscribed
Cut surface is soft and typically glistening with gelatinous appearance
Size
Can show wide range of sizes from < 1 cm up to > 10 cm
Median size: 2 cm
MICROSCOPIC PATHOLOGY
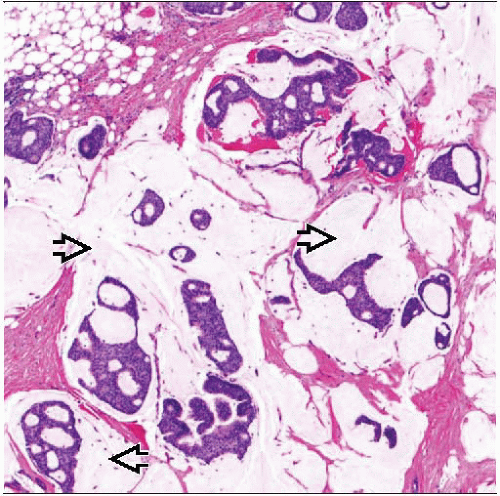
Histologic Features
Pools of extracellular stromal mucin make up at least 1/3 of volume throughout tumor in pure MC
Delicate fibrous septae divide pools or lakes of mucin into compartments
Detached epithelial elements are present floating in pools of mucin
Mucin should surround all tumor cell nests
Pure MC should not contain areas of usual type of invasion of stroma in absence of mucin
If present, tumor should be designated as mixed mucinous/ductal
Pure MC has > 90% mucinous histology (frequently entire tumor is mucinous)
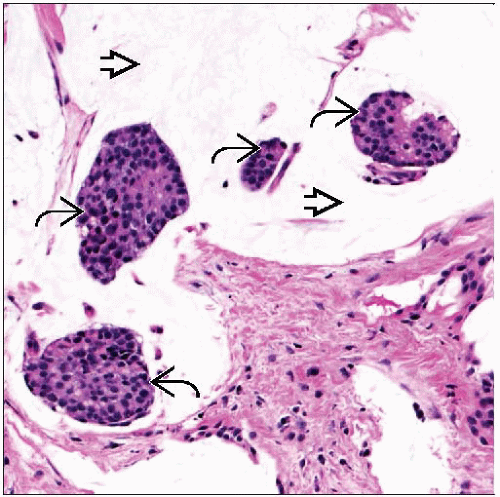
Majority of cases have low-grade nuclei and would be classified as well or moderately differentiated
Rare cases of poorly differentiated MC do occur (10% of total)
Pure MC can be divided into 2 main subtypes based on architectural and cytological features
Mucinous type A carcinomas are paucicellular
Large quantities of extracellular mucin production
Neuroendocrine marker expression is not typical
Mucinous type B carcinomas are more hypercellular
Contain less mucin and more tumor cells
Neuroendocrine markers and argyrophilia are present in 25%
Older patient age
Lower tumor nuclear grade
Lower incidence of axillary node metastasis
MC is often associated with DCIS component
DCIS may show micropapillary, cribriform, or solid patterns
DCIS may also demonstrate prominent mucin production
ANCILLARY TESTS
Immunohistochemistry
Most MC will show expression of ER and PR
Typically tumors express high levels of both receptors
MC more likely to be ER (94%) and PR (81%) positive compared with carcinomas of no special type
HER2 and EGFR overexpression is very uncommon
Some MC can show neuroendocrine differentiation
Tumor cells will show expression of 1 or more neuroendocrine markers
Chromogranin, synaptophysin, CD56
MC expressing neuroendocrine markers are classified as type B by some authors
Tumors that are classified as type A typically do not show neuroendocrine differentiation
Neuroendocrine differentiation associated with better prognosis in some reports
Prognostic significance of neuroendocrine differentiation is not well established
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree