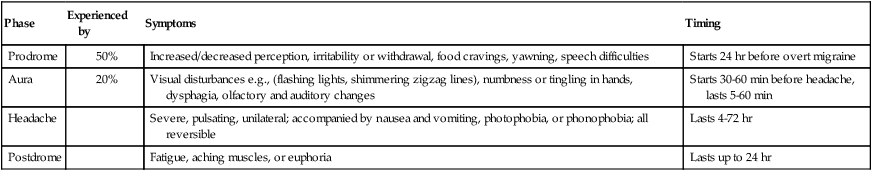
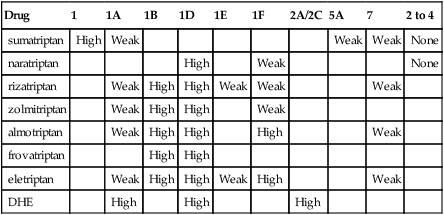
Chapter 44 ∗Some products are off the market now, but available as combination products. Tension headache (THA), the most common type of headache, usually is described as vise-like pressure associated with stress and/or fatigue. The pain of THA usually is generalized but may be worse in the area of the neck and the back of head. These patients are generally treated with analgesics for mild to moderate pain. (See Chapter 43 for more information on pain management.) Migraine symptoms vary. All migraines are paroxysmal in nature—clearly defined attacks separated by symptom-free intervals. Daily or continuous headaches usually are not migraines but are tension or vascular headaches. Migraines are classified as with aura or without aura and are graded as mild, moderate, or severe in intensity. The duration of migraine is an important variable because the clinician must choose medications whose duration of action is adequate. Classic migraines go through specific phases (Table 44-2). TABLE 44-2 Diagnosed migraine must meet specific criteria established by the National Headache Foundation (Box 44-1). A diagnostic workup headache history includes age of onset of headaches; duration of complaint; frequency and duration of each headache; site, quality, and time of onset; associated phenomena; and aggravating and relieving factors. Physical examination, including neurologic examination, is typically normal. Some patients experience substantial burden from their migraines. The Migraine Disability Assessment Scale (MIDAS) is a five-item questionnaire that is used in practice (see Goadsby et al, 2002, for questionnaire uhs.berkeley.edu/home/healthtopics/pdf/assessment.pdf) to help the clinician measure how much intervention is required to improve the patient’s quality of life. Migraine headache often is stimulated by visual, olfactory, or other environmental triggers that may be identified. (See Box 44-3.) The patient must be screened for concurrent illnesses, especially cardiovascular problems such as increased blood pressure and CAD. These concurrent illnesses may affect treatment options. See Table 44-3 for drug effects on serotonin receptors. TABLE 44-3 Drug Effects on Serotonin (5-HT) Receptors From Silberstein SD: Practice parameters: evidence-based guidelines for migraine headache, Neurology 55:754-762, 2000. peripheral and cranial vessels. Ergot drugs also produce an increase in central vasomotor center stimulation. Although dihydroergotamine (DHE) is an ergot, it is also a 5-HT1B/1D receptor agonist that is not as selective as the triptans. DHE binds to norepinephrine (noradrenaline) α1, α2A, and α2B and dopamine D2L and D3 receptors. It is a stronger venoconstrictor and a weaker arterial vasoconstrictor than ergotamine. See Table 44-1 for a list of prophylactic medications. TABLE 44-1 Drugs Commonly Used for Prophylaxis Discussed in Other Chapters
Migraine Medications
Class
Subclass
Generic Name
Trade Name
Abortive agents
Serotonin 5-HT1D receptor agonists
sumatriptan ![]()
Imitrex, generic
frovatriptan
Frova
naratriptan
Amerge, generic
rizatriptan
Maxalt
almotriptan
Axert
zolmitriptan
Zomig
5-HT1B/1D
eletriptan
Relpax
Ergotamine derivatives
ergotamine tartrate ![]()
Cafergot, generic
dihydroergotamine (DHE)
DHE-45, Migranal, generic
isometheptenemucate
Midrin, generic∗
Prophylactic agents
cyproheptadine
Periactin, generic
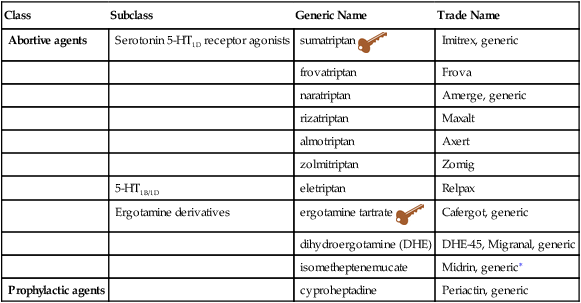
![]() Key drug. Key drugs chosen because they were first in their class and are still used. See Table 44-1 for discussions in other chapters of drugs commonly used for prophylaxis.
Key drug. Key drugs chosen because they were first in their class and are still used. See Table 44-1 for discussions in other chapters of drugs commonly used for prophylaxis.
Therapeutic Overview
Pathophysiology
Disease Process
Phase
Experienced by
Symptoms
Timing
Prodrome
50%
Increased/decreased perception, irritability or withdrawal, food cravings, yawning, speech difficulties
Starts 24 hr before overt migraine
Aura
20%
Visual disturbances e.g., (flashing lights, shimmering zigzag lines), numbness or tingling in hands, dysphagia, olfactory and auditory changes
Starts 30-60 min before headache, lasts 5-60 min
Headache
Severe, pulsating, unilateral; accompanied by nausea and vomiting, photophobia, or phonophobia; all reversible
Lasts 4-72 hr
Postdrome
Fatigue, aching muscles, or euphoria
Lasts up to 24 hr
Assessment
Mechanism of Action
Abortive Agents
Drug
1
1A
1B
1D
1E
1F
2A/2C
5A
7
2 to 4
sumatriptan
High
Weak
Weak
Weak
None
naratriptan
High
Weak
None
rizatriptan
Weak
High
High
Weak
Weak
Weak
zolmitriptan
Weak
High
High
Weak
almotriptan
Weak
High
High
High
Weak
frovatriptan
High
High
eletriptan
Weak
High
High
Weak
High
Weak
DHE
High
High
High
Prophylactic Agents
Class
Generic Name
Trade Name
Dosage 24 Hours
Chapter
β-Blockers
atenolol
Tenormin
25-200 mg
20
metoprolol
Toprol XL, Lopressor
50-200 mg
nadolol
Corgard
20-120 mg
propranolol
Inderal
20-160 mg
Calcium channel blockers
verapamil
Calan, Isoptin, Verelan
120-480 mg
21
Antidepressants
fluoxetine
Prozac
10-80 mg
47
amitriptyline
Elavil
10-150 mg
Anticonvulsants
divalproex
Depakote
125-200 mg
45
topiramate
Topamax
50-150 mg
gabapentin
Neurontin
300-2400 mg
NSAIDs
Analgesics
aspirin
1300 mg/day
35, 36
Ibuprofen
acetaminophen
Tylenol
800 mg/day
Combinations of above with caffeine
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Migraine Medications
Only gold members can continue reading. Log In or Register to continue
