Metaplastic Carcinoma
Key Facts
Terminology
Metaplastic breast carcinoma (MBC) includes a diverse group of tumors consisting entirely, or in part, of components that do not have the histologic appearance of adenocarcinoma
Major subtypes include
Carcinomas with squamous/spindle cell morphology
Carcinomas with matrix production
Carcinomas with a true malignant mesenchymal component
Clinical Issues
MBCs are uncommon (< 1% of all breast cancers)
Usually presents as large palpable mass
Lymph node metastases are less frequent compared with other carcinomas of similar size
Prognosis is generally poor, except for some subtypes (e.g., low-grade adenosquamous carcinoma)
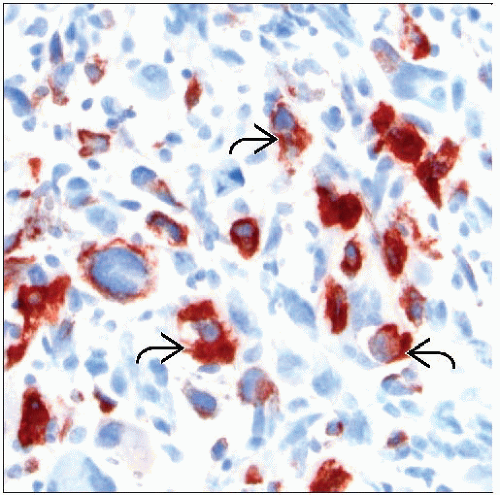
Ancillary Tests
Majority are negative for ER, PR, and HER2
Expression of cytokeratin should be present for diagnosis
Cytokeratin reactivity is often focal, and only basal types (CK14 and CK17) may be present
Top Differential Diagnoses
Squamous cell carcinoma of the skin
Phyllodes tumor
Primary or metastatic sarcoma
Epithelial/myoepithelial tumors (including adenoid cystic carcinoma and pleomorphic adenoma)
TERMINOLOGY
Abbreviations
Metaplastic breast carcinoma (MBC)
Definitions
MBC encompasses a diverse group of carcinomas that consist entirely, or in part, of elements that do not have the histologic appearance of adenocarcinoma
MBC has 3 main categories
Carcinomas with squamous &/or spindle cells
Squamous cell carcinoma
Spindle cell carcinoma
Adenosquamous carcinoma
Low-grade carcinoma with fibromatosis-like stroma
Matrix-producing carcinomas
Carcinomas with a true malignant mesenchymal component (carcinosarcoma)
ETIOLOGY/PATHOGENESIS
Cell of Origin
All MBCs show at least focal evidence of origin as an epithelial malignancy
Cytokeratin expression should be present but may be focal and only for “basal” keratins (14 and 17)
1 study demonstrated that, when 2 components are present, both share the same P53 mutation
Data support concept that biphasic MBC is a monoclonal tumor
Many MBCs have features of myoepithelial differentiation
About 1/3-2/3 express markers typical of myoepithelial cells, including p63, smooth muscle actin, P-cadherin, maspin, or CD10
Myoepithelial cells can produce basement membrane material that may resemble cartilage or bone
Myoepithelial cells can be spindled in shape and closely resemble squamous cells
Squamous metaplasia may occur primarily in myoepithelial cells
Very rarely, MBC is associated with true mesenchymal differentiation
Sarcomatous portion of tumor should show definitive mesenchymal features
Monoclonality of these carcinomas supports that sarcoma component arises from malignant epithelial cells
Gene Expression Profiling
MBC has a distinctive molecular signature, separating it from other molecular classes of breast carcinomas
Majority demonstrate a transcriptional profile similar to, but distinct from, basal-like carcinomas
Profile is most similar to a claudin-low group of carcinomas
Discriminator genes for MBC fall into several groups
Decreased expression of genes related to cell adhesion and increased expression of E-cadherin repressors
These genes are hypothesized to play a role in the epithelial to mesenchymal transition
E-cadherin can be present by IHC in epithelial component and absent in matrix-producing component of MBC
Increased expression of genes involved in extracellular matrix formation
Increased expression of genes thought to be associated with stem cell-like patterns
Expression pattern for MBC is similar to that of residual carcinoma not responding to chemotherapy
May indicate a gene expression pattern associated with chemoresistance
DNA Studies
MBC has pattern of copy number gains and losses distinct from basal-like carcinomas as well as other groups
Gains of 1p/5p and loss of 3q were most common
High frequency of mutation, amplification, and activation of P13K/AKT pathway genes
Changes in this pathway are uncommon in basal-like carcinomas
CLINICAL ISSUES
Epidemiology
Incidence
Rare, < 1% of breast cancers
Presentation
Typically presents as a large palpable mass
May be associated with rapid growth
Prognosis
Limited prognostic data are available due to rarity of MBC
Axillary lymph node metastases are less common in MBC compared with other cancers of similar size
Nodal metastases very uncommon for tumors showing spindle cell and squamous features
Metastatic route may be primarily hematogenous to lung and liver
Prognosis for some types of MBC is significantly worse than for non-MBC in some studies
May be related to higher stage at presentation
Most MBCs are triple negative; thus hormonal or HER2-targeted therapy is not available
MBC may be more resistant to chemotherapy than other types of breast carcinoma
However, some low-grade subtypes of MBC have a favorable prognosis
IMAGE FINDINGS
General Features
Size
Tumors tend to be larger compared with other types of invasive breast cancers
Mean: 2.5-4.5 cm (range: 1 to > 10 cm)
Mammographic Findings
Lobulated or irregular mass
Usually partially circumscribed and partially indistinct
Calcifications
Usually absent or subtle
Rarely, calcification can be prominent when associated with extracellular matrix production or ossification
MICROSCOPIC PATHOLOGY
Histologic Features
MBC comprises a very heterogeneous group of carcinomas
Although there are several main categories of MBC, some carcinomas can be difficult to classify due to unusual histologic patterns
Usually associated with little or no DCIS
When DCIS is present, its presence supports classification as MBC
Squamous Cell Carcinoma (SCC)
SCC is often located centrally in the breast
Typically adjacent to a cystic cavity
May arise in areas of squamous metaplasia secondary to inflammation
Cells that undergo metaplasia may be myoepithelial cells
In situ SCC may be present in a cyst wall or a duct
Squamous component of MBC can range from well to poorly differentiated
May be keratinizing or nonkeratinizing
SCC adjacent to areas of squamous metaplasia in cysts or papillomas can mimic reactive stromal cells
IHC may be necessary to identify spindle cells as carcinoma
Rare acantholytic growth pattern can resemble angiosarcoma
Epithelium degenerates and forms pseudovascular spaces
Lymph node metastases are rare
Prognosis is similar to carcinomas of no special type
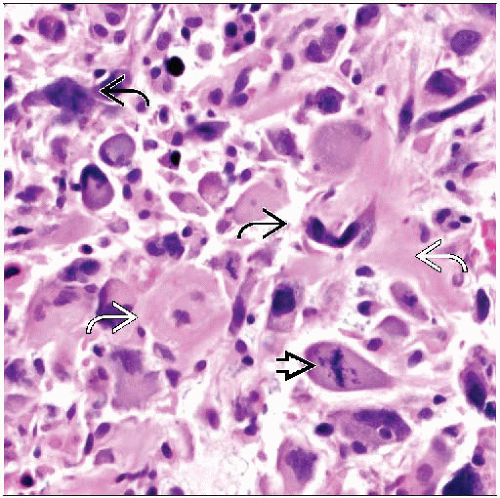
Spindle Cell Carcinoma
May present as pure spindle cells or an admixture of spindle cells with epithelioid and heterologous elements
Appearance of spindle cell component can range from bland low-grade cytology to cells with highly pleomorphic nuclei and frequent mitoses
Lymphocytic infiltrate is commonly present
Frequently expresses myoepithelial markers including p63, smooth muscle actin, and muscle specific actin
May be classified as sarcomatoid carcinoma or myoepithelial carcinoma
Lymph node metastases are rare, but overall prognosis is generally poor
Low-Grade Spindle Cell Carcinoma with Fibromatosis-like Stroma
Spindle cells have very bland small nuclei and resemble fibroblasts
Small areas with epithelioid-appearing cells may be present
Cellularity is low
Stromal collagen may be prominent
Differential diagnosis often includes fibromatosis, nodular fasciitis, or reactive stromal cells
Prognosis is favorable, but occasional distant metastases have been reported
Adenosquamous Carcinoma (ASC)
Carcinomas composed of both adenocarcinoma and SCC
Can vary from low grade to high grade
Very rare carcinomas resemble mucoepidermoid carcinoma of the salivary glands
Low-grade ASC is composed of well-formed glands and squamous nests
Glandular structures are rounded
Squamous nests are usually solid and can be comma-shaped; keratin pearls may be present
Nuclear pleomorphism is minimal, and mitoses are generally absent
Majority of associated spindle cells are usually reactive fibroblasts, but a few may be tumor cells
Usually smaller (˜ 2 cm) than other types of MBC
Resembles syringomatous adenoma of the nipple
Prognosis is generally very favorable
MBC with Matrix Production (Cartilaginous or Chondroid)
Matrix consists of homogeneous, often abundant, extracellular material
Can appear cartilaginous, myxoid, or collagenous
May be basement membrane-type material or (less likely) true cartilage
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree