DRUG CLASSES
Female hormones
• Estrogens
• Progestins
Antispasmodics
Benign prostatic Hyperplasia (BPH) Agents
• α-adrenergic blockers
• Androgen hormone Inhibitors
• Impotence agents
Hormonal cancer agents
In both men and women, aging reproductive system changes are closely related to changes in the urinary system. Menopause makes changes for women very pronounced because fertility stops. For men change is not as overt. Hormonal and urinary changes may be more subtle and are referred to as andropause. Changes to a woman’s reproductive system, the shared changes to the genitourinary system, and changes to the male are described in this chapter. The goal of drug treatment is to reduce symptoms related to the changes of aging reproductive and urinary systems.
PHARMACOLOGY IN PRACTICE

Mr. Phillip, a 72-year-old widower who lives alone, was diagnosed with a UTI 8 weeks ago. Having failed to come in for a follow-up urine sample 2 weeks after completing the course of drug therapy, he is at the clinic to see a primary health care provider because the UTI symptoms are now worse.
Menopause
The female fertility cycle, which is under the influence of estrogen and progesterone, is described in Chapter 45. As women age there is a complex change in these and other hormones. Estrogen diminishes and the menstrual cycle can become irregular until it stops altogether. As the hormonal influence lessens women are said to be in the female climacteric or menopause.
The purpose of this section is to provide you with information to support the woman who has opted for hormone replacement therapy (HRT). Estrogen replacement therapy has been studied extensively. When a woman is premenopausal, this is a good time to discuss options with her primary health care provider. She should discuss the benefit of relief of symptoms (e.g., hot flashes) with negative impact on her body (e.g., blood pressure and lipid changes). Many of the physical changes throughout the body associated with loss of estrogen are illustrated in Figure 47.1. Information about medications used to deal with heart disease or bone changes of older women are discussed in Unit VIII and Chapter 30, respectively.
Aging of the female genitourinary system includes fat atrophy and hormonal changes, which are responsible for the following:
• Vaginal walls become thinner, shorten, and lose some of their elasticity.
• The vagina produces less lubrication and at a slower rate during sexual arousal.
• The pH environment changes, making the vagina more susceptible to yeast infections.
• Pelvic floor muscles weaken and lead to stress incontinence.
Symptoms related to these changes can be reduced by replacing the lost hormones.
ESTROGENS
Actions and Uses
In addition to contraception, estrogen is most commonly used in HRT (or estrogen replacement therapy [ERT]) in postmenopausal women. Changes to aging tissues can be lessened when estrogens are used for the following:
• Relief of moderate to severe vasomotor symptoms of menopause (flushing, sweating)
• Treatment of atrophic vaginitis
• Treatment of osteoporosis in women past menopause
• Palliative treatment of advanced prostatic carcinoma (in men)
• Selected cases of advanced breast carcinoma
The estradiol transdermal system is also used after removal of the ovaries in premenopausal women (female castration) and primary ovarian failure. Estrogen is given intramuscularly (IM) or intravenously (IV) to treat uterine bleeding caused by hormonal imbalance. When estrogen is used to treat menopausal symptoms in a woman with an intact uterus, concurrent use of progestin is recommended to decrease the risk of endometrial cancer. After a hysterectomy, estrogen alone may be used for ERT.
Adverse Reactions
Administration of estrogens by any route may result in many adverse reactions, although the incidence and intensity of these reactions vary. Some of the adverse reactions seen with the administration of estrogens are as follows.
Central Nervous System Reactions
• Headache, migraine
• Dizziness, mental depression
Dermatologic Reactions
• Dermatitis, pruritus
• Chloasma (pigmentation of the skin) or melasma (discoloration of the skin), which may continue when use of the drug is discontinued
Gastrointestinal Reactions
• Nausea, vomiting
• Abdominal bloating and cramps
Genitourinary Reactions
• Breakthrough bleeding, withdrawal bleeding, spotting, changes in menstrual flow
• Dysmenorrhea, premenstrual-like syndrome, amenorrhea
• Vaginal candidiasis, cervical erosion, vaginitis
Local Reactions
• Pain at injection site or sterile abscess with parenteral form of the drug
• Redness and irritation at the application site with transdermal system
Ophthalmic Reactions
• Steepening of corneal curvature
• Intolerance to contact lenses
Miscellaneous Reactions
• Edema, rhinitis, changes in libido
• Breast pain, enlargement, and tenderness
• Reduced carbohydrate tolerance
• Venous thromboembolism, pulmonary embolism
• Weight gain or loss
• Generalized and skeletal pain
Warnings associated with the administration of estrogen include an increased risk of endometrial cancer, gallbladder disease, hypertension, hepatic adenoma (a benign tumor of the liver), cardiovascular disease, and thromboembolic disease, and hypercalcemia in those with breast cancer and bone metastases.
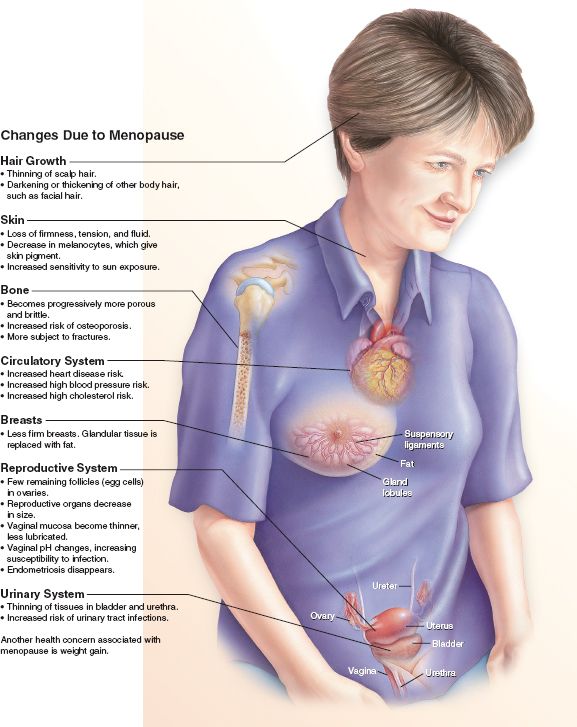
Figure 47.1 Menopausal changes in the female body.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Menopausal Women
Controversy persists over the increased risk for chronic heart disease and female cancers with the use of estrogen. Using the lower-dose agents before the age of 60 may be beneficial. Alternative delivery systems are being explored to reduce the use of oral estradiol products.
Contraindications and Precautions
Estrogen and progestin therapy is contraindicated in patients with known hypersensitivity to the drugs, breast cancer (except for metastatic disease), estrogen-dependent neoplasms, undiagnosed abnormal genital bleeding, and thromboembolic disorders. The progestins also are contraindicated in patients with cerebral hemorrhage or impaired liver function. Both the estrogens and progestins are classified as pregnancy category X drugs and are contraindicated during pregnancy.
Estrogens are used cautiously in patients with gallbladder disease, hypercalcemia (may lead to severe hypercalcemia in patients with breast cancer and bone metastasis), cardiovascular disease, and liver impairment. Cardiovascular complications are greater in women who smoke and use estrogen. Progestins are used cautiously in patients with a history of migraine headaches, epilepsy, asthma, and cardiac or renal impairment.
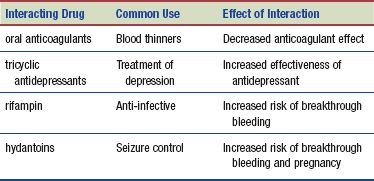
Interactions
The following interactions may occur with female hormones:
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Black cohosh, an herb reported to be beneficial in managing symptoms of menopause, is generally regarded as safe when used as directed. Black cohosh is a member of the buttercup family. Black cohosh tea is not considered as effective as other forms. Boiling the root releases only a portion of the therapeutic constituents. The benefits of black cohosh (not to be confused with blue cohosh) include:
• Reduction in physical symptoms of menopause: hot flashes, night sweats, headaches, heart palpitations, dizziness, vaginal atrophy, and tinnitus (ringing in the ears)
• Decrease in psychological symptoms of menopause: insomnia, nervousness, irritability, and depression
• Improvement in menstrual cycle regularity by balancing the hormones and reducing uterine spasms
Adverse reactions are rare; the most common adverse reaction is nausea. Black cohosh is contraindicated during pregnancy. Toxic effects include dizziness, headache, nausea, impaired vision, and vomiting. This herb is purported to be an alternative to HRT. In addition to its popularity as an herb for women’s hormonal balance, black cohosh has been used for muscular and arthritic pain, headache, and eyestrain (DerMarderosian, 2003). Other herbs used to relieve menopausal symptoms include sage, dandelion, and calendula.
Urinary Aging
As a person’s age increases, so do the number of urinary system disorders. All parts of the urinary system are affected by aging. Changes in kidney size and blood flow to the kidney reduce renal function by almost 50% in older individuals. These changes decrease the filtration and the urine becomes more dilute. Diuretics (Chapter 33) are used to maintain function in the kidney as well as to reduce fluid in the body for hypertension control.
The urinary bladder diminishes in strength, flexibility, and capacity resulting in frequent urination, especially at night (nocturia). The urethra shortens and its lining becomes thinner, increasing susceptibility to infection. In addition to the effects of childbirth and loss of muscle tone in pelvic structures, the urinary sphincter becomes less flexible and is less able to close tightly, resulting in urine leakage (stress incontinence). This type of incontinence is typically treated with surgical or behavior interventions.
Another continence issue can occur when the sensation of having to urinate is not as strong and may not be felt until the bladder is completely full. Then the need to void is sudden and urgent and there may be a loss of urine (urge incontinence). This type of incontinence can be treated with drugs called antispasmodics. Overactive bladder syndrome (OBS, or involuntary contractions of the detrusor or bladder muscle) also presents with urinary urgency. OBS is estimated to affect more than 16 million individuals in the United States. This problem sometimes results from such disorders as cystitis or prostatitis or from abnormalities related to affected structures, such as the kidney or the urethra. Symptoms of an overactive bladder include urinary urgency (a strong and sudden desire to urinate), frequent urination throughout the day and night, and urge incontinence. Another urinary issue in men involves an enlarged prostate, which can eventually interfere with urination. The enlarged prostate compresses the urethra, reducing the flow of urine from the bladder. This also makes men more susceptible to urinary tract infections.
ANTISPASMODICS
Actions and Uses
Antispasmodics are cholinergic blocking drugs that inhibit bladder contractions and delay the urge to void. These drugs counteract the smooth muscle spasm of the urinary tract by relaxing the detrusor and other muscles through action at the parasympathetic nerve receptors (see Chapter 27). Flavoxate (Urispas) is used to relieve symptoms of dysuria (painful or difficult urination), urinary urgency, nocturia (excessive urination during the night), suprapubic pain and frequency, and urge incontinence. The other antispasmodic drugs are also used to treat bladder instability (i.e., urgency, frequency, leakage, incontinence, and painful or difficult urination) caused by a neurogenic bladder (impaired bladder function caused by a nervous system abnormality, typically an injury to the spinal cord).
Adverse Reactions
Adverse reactions to these drugs are similar to those with other cholinergic blocking drugs. They include the following:
• Dry mouth, drowsiness, constipation or diarrhea, decreased production of tears, decreased sweating, gastrointestinal (GI) disturbances, dim vision, and urinary hesitancy
• Nausea and vomiting, nervousness, vertigo, headache, rash, and mental confusion (particularly in older adults)
Patients should be told that antispasmodic drugs can discolor the urine (dark orange to brown) and stain undergarments that come in contact with the urine.
Contraindications and Precautions
Antispasmodic drugs are contraindicated in those patients with known hypersensitivity to the drugs or with glaucoma. Other patients for whom antispasmodics are contraindicated are those with intestinal or gastric blockage, abdominal bleeding, myasthenia gravis, or urinary tract blockage.
These drugs should be used with caution in patients with GI infections, benign prostatic hypertrophy, urinary retention, hyperthyroidism, hepatic or renal disease, and hypertension. Antispasmodic drugs are classified as pregnancy category C drugs and are used only when the benefit to the woman outweighs the risk to the fetus.
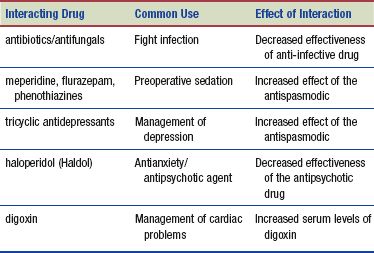
Interactions
The following interactions may occur when an antispasmodic drug is administered with another agent:
Andropause
Unlike women, men do not go through a major change in fertility like women experience (menopause). Instead, changes occur gradually and are called andropause or the male climacteric. Aging changes in the male reproductive system occur primarily in the testes. Like the ovary, testicular tissue diminishes; what is different is that the male sex hormone levels (of testosterone) remain relatively constant.
The change men often notice is prostate enlargement. The prostate gland is about the size of a walnut, sits below the bladder, and wraps around the urethra. Scar tissue replaces prostate cells and causes the enlargement. Fifty percent of men will experience benign prostatic hypertrophy (BPH) as they age (Fig. 47.2). BPH may cause difficulty in urination, retention of urine, and incontinence. Prostate gland infections or inflammation (prostatitis) may also occur. The risk of prostate cancer is no greater in men with BPH, although symptoms may be similar, prostate cancer is due to a change in the prostate cells (see Chapter 50). Treatment for BPH is aimed at relieving symptoms and improving urinary flow.
 NURSING ALERT
NURSING ALERT
Early-stage prostate cancer may not have signs or symptoms. When men present with issues such as difficulty with urination, reduced flow, or blood in the urine, prostate cancer should always be ruled out before treatment is started for BPH.
DRUGS TO TREAT BENIGN PROSTATIC HYPERTROPHY
Treatment for BPH includes monitoring, medications, or invasive procedures. Drugs are used for mild to moderate symptoms of BPH (e.g., frequency, reduced flow, nocturia, and dysuria) and include androgen inhibitors and adrenergic blockers.
Actions and Uses
The most widely used drugs to treat BPH are the alpha (α)-adrenergic blockers. As discussed in Chapter 25, adrenergic blockers prevent the neurotransmission of norepinephrine. The drugs used for BPH are peripherally acting, α1a-adrenergic blockers that exert their action primarily on the smooth muscle of the prostate and the bladder neck. By blocking norepinephrine, the muscles relax and this allows urine to flow from the bladder. Adrenergic blockers can be uroselective; therefore, the α1a-adrenergic blockers exert their action on the bladder with minimal action on the vascular system.
Androgen hormone inhibitors (AHIs) have been used for many years to deal with symptoms of BPH. The biggest drawback has been the adverse effects of erectile dysfunction (ED) and decreased libido. The androgen hormone inhibitors prevent the conversion of testosterone into the androgen 5-α-dihydrotestosterone (DHT). The growth of the prostate gland depends on DHT. The lowering of serum levels of DHT reduces the effect of this hormone on the prostate gland, resulting in a decrease in the size of the gland and the symptoms associated with prostatic gland enlargement.
Currently the use of both types of drugs is being studied (Dhingra, 2011) and is proving successful based on the different sites of action of the drugs. There is one drug on the market that combines an α1a-adrenergic blocker with an AHI—Jalyn, a combination of dutasteride and tamsulosin.
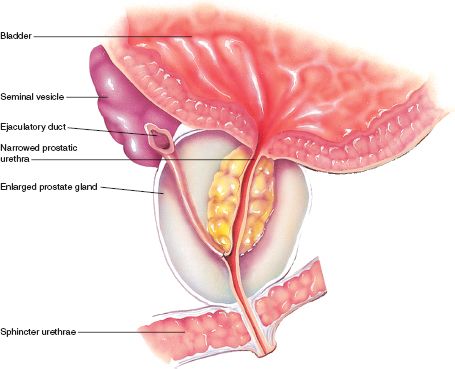
Figure 47.2 Enlarged prostate and narrowing of urethra results in reduced urinary flow. (Asset provided by Anatomical Chart Co.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


