Mantle Cell Lymphoma, Blastoid Variant
C. Cameron Yin, MD, PhD
Key Facts
Terminology
Highly aggressive subtype of mantle cell lymphoma composed of cells that resemble lymphoblasts (classic variant) or are large, atypical, and pleomorphic (pleomorphic variant)
Clinically aggressive type of MCL with high-grade cytologic features: 2 major variants
Etiology/Pathogenesis
t(11;14)(q13;q32) juxtaposes CCND1 with IGH and results in Cyclin-D1 overexpression and cell cycle progression
Other molecular genetic abnormalities
P53, P21, P16, MYC
Clinical Issues
Clinical and biological features are comparable to those of typical MCL
Associated with particularly short durations of response after chemotherapy and poorer overall survival
Microscopic Pathology
2 variants are recognized: Classic and pleomorphic
Top Differential Diagnoses
Lymphoblastic lymphoma
Myeloid sarcoma
Diffuse large B-cell lymphoma
Burkitt lymphoma
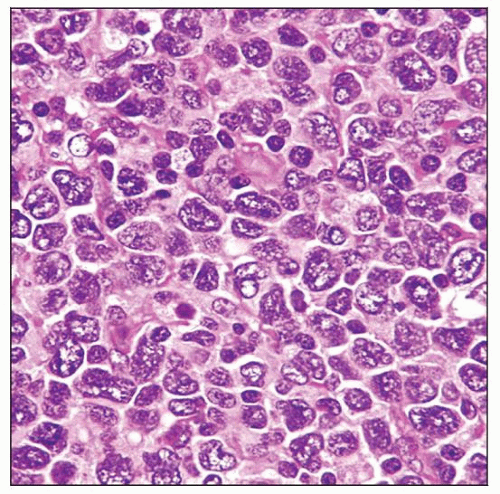
 Lymph node involved by MCL, blastoid variant. In this case, a “starry sky” pattern is present and the neoplastic cells resemble, in part, lymphoblasts. This case carried the t(11;14)(q13;q32). |
TERMINOLOGY
Abbreviations
Mantle cell lymphoma (MCL), blastoid variant (BV)
Synonyms
Mantle cell lymphoma, lymphoblastoid variant
Mantle cell lymphoma, large cell variant
Mantle cell lymphoma, blastic
Definitions
Clinically aggressive type of MCL with high-grade cytologic features: 2 major variants
2 variants of MCL as stated in 2001 WHO classification
Classical and pleomorphic
2 aggressive variants of MCL as stated in 2008 WHO classification
Blastoid and pleomorphic
ETIOLOGY/PATHOGENESIS
t(11;14)(q13;q32)
Virtually all cases of MCL carry t(11;14)(q13;q32)
Juxtaposes CCND1 at 11q13 with IgH at 14q32 and results in Cyclin-D1 overexpression, Rb phosphorylation, and release of E2F
Facilitates cell cycle progression from G1 to S phase
Other Cytogenetic and Molecular Genetic Abnormalities
P53 overexpression and mutations
P16/INK4a deletions and mutations
CLINICAL ISSUES
Epidemiology
Incidence
MCL represents approximately 6% of all non-Hodgkin lymphomas
MCL-BV represents at least 10-15% of all MCL cases
Frequency is probably higher in patients who are followed for long periods of time
Presentation
Median age: 6th to 7th decades
Clinical features of MCL-BV are comparable to those of typical MCL
Male predominance (M:F = 2-3:1)
B symptoms in 30-50%; may be more common in patients with MCL-BV
Lymphadenopathy, generalized
Extranodal involvement is common
Gastrointestinal tract is most common site
Unusual extranodal sites can be involved in patients with MCL-BV
Most patients present with Ann Arbor clinical stage III/IV
MCL International Prognostic Index (MIPI) often high
Based on: Age, ECOG performance status, serum lactate dehydrogenase (LDH), blood leukocyte count
Rare prolymphocytoid variant of MCL is probably a form of MCL-BV
Patients present with high leukocyte count (often > 100 K/uL) and poor prognostic features
Extensive bone marrow involvement
Prominent splenomegaly
Often short survival
Treatment
Aggressive chemotherapy &/or stem cell transplantation
Prognosis
Short durations of clinical response after chemotherapy and poorer overall survival
MCL-BV patients have poor overall survival
Reported to be 14.5 months in 1 study
IMAGE FINDINGS
Radiographic Findings
Widespread lymphadenopathy
MICROSCOPIC PATHOLOGY
Histologic Features
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree