Male Reproductive System
SEXUAL REPRODUCTION
Sexual reproduction requires two parent organisms, a male and female, each of which contributes half of the nuclear chromosomes needed to form the first cell of an offspring organism. Asexual reproduction, on the other hand, requires only one parent who produces an offspring genetically identical to itself. An advantage of sexual reproduction is that a new mixture of genes in each offspring increases the variety of genetic characteristics in the population. This variety of characteristics makes it more likely that in the case of infectious disease or environmental changes such as natural disaster or shifting climatic conditions, there will be at least some individuals likely to survive and carry on the reproductive line.
Besides producing the cells needed to form the offspring, each reproductive system produces hormones that regulate development of the secondary sex characteristics that promote successful reproduction. For example, hormones create structural and behavioral differences in the sexes that permit adults to recognize and form sexual attractions with the opposite sex. Reproductive hormones and other regulatory mechanisms give us the urge to have sex, which is often reinforced with the pleasant sensations that sexual activity can produce. This sex drive is essential to success in producing offspring.
Sexual maturity and the ability to reproduce occur at puberty. The male reproductive system consists of organs whose functions are to produce, transfer, and ultimately introduce mature sperm into the female reproductive tract, where the nuclear chromosomes from each parent can unite to form a new offspring.
MALE REPRODUCTIVE ORGANS
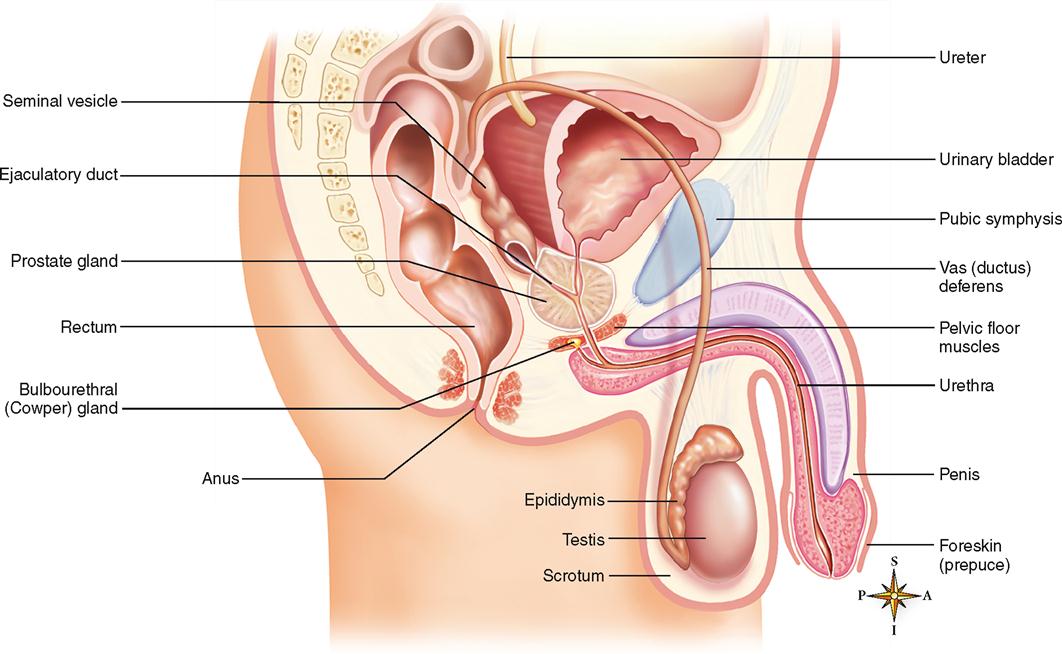
Organs of the reproductive system (Figure 34-1) may be classified as essential organs for the production of gametes (sex cells) or as accessory organs that play some type of supportive role in the reproductive process.
In both sexes the essential organs of reproduction that produce the gametes, or sex cells (sperm or ova), are called gonads. In Chapter 36, we will explore the development of male and female reproductive organs more thoroughly. The gonads of the male are the testes.
The accessory organs of reproduction in the male include genital ducts, glands, and supporting structures.
Reproductive ducts convey sperm to the outside of the body. They are also called genital ducts. The ducts are a pair of epididymides (singular, epididymis), the paired vasa deferentia (singular, vas deferens), a pair of ejaculatory ducts, and the urethra. Accessory glands in the reproductive system produce secretions that serve to nourish, transport, and mature sperm. The glands are a pair of seminal vesicles, one prostate, and a pair of bulbourethral glands. Supporting structures include the scrotum, the penis, and a pair of spermatic cords.
Perineum
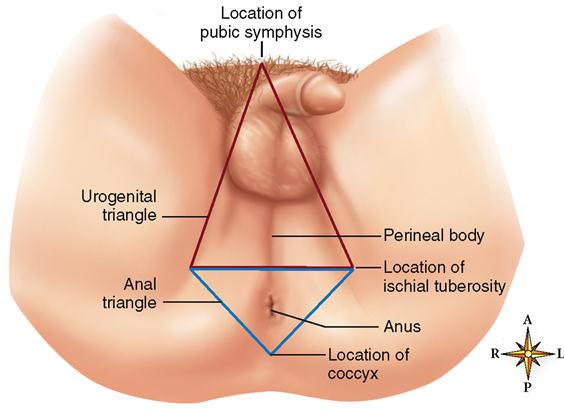
The perineum in the male is an area between the thighs shaped roughly like a diamond (Figure 34-2). It extends from the pubic symphysis anteriorly to the coccyx posteriorly. Its most lateral boundary on either side is the ischial tuberosity. A line drawn between the two ischial tuberosities divides the area into a larger urogenital triangle, which contains the external genitals (penis and scrotum), and the anal triangle, which surrounds the anus.
TESTES
Structure and Location
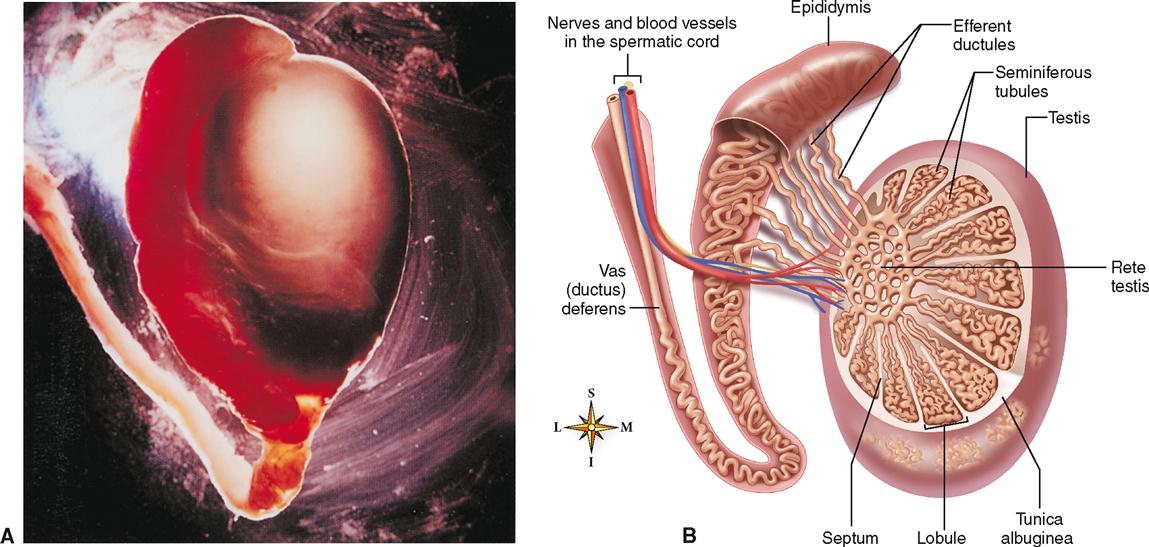
The testes are small, ovoid glands that are somewhat flattened from side to side, measure about 4 or 5 cm in length, and weigh 10 to 15 grams each. They are both located in a supporting sac called the scrotum. The left testis is generally located about 1 cm lower in the scrotal sac than the right. Both testes are suspended in the pouch by attachment to scrotal tissue and by the spermatic cords (Figure 34-3). Note in Figure 34-3, B, that testicular blood vessels reach the testes by passing through the spermatic cord.
A dense, white, fibrous capsule called the tunica albuginea encases each testis and then enters the gland, sending out partitions (septa) that radiate through its interior, dividing it into 200 or more cone-shaped lobules.
Each lobule of the testis contains scattered interstitial cells and one to three tiny, coiled seminiferous tubules, which, if unraveled, would measure about 75 cm (more than 2 feet) in length. The tubules from each lobule come together to form a plexus called the rete testis. A series of sperm ducts called efferent ductules then drain the rete testis and pierce the tunica albuginea to enter the head of the epididymis (see Figure 34-3).
Microscopic Anatomy of the Testis
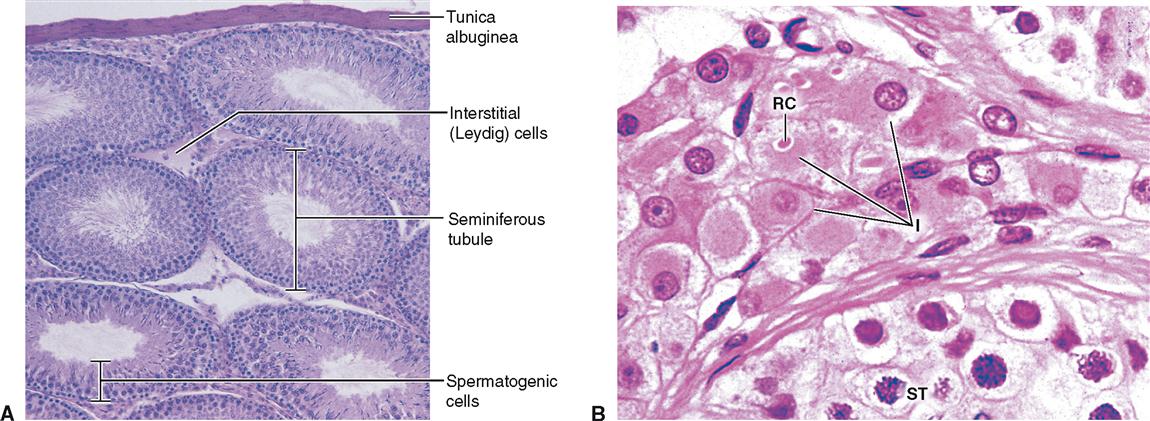
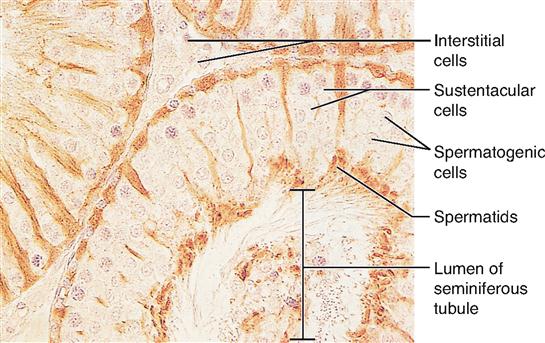
Figure 34-4, A is a low-power (×70) micrograph of testicular tissue showing a number of cut seminiferous tubules and numerous interstitial cells, or Leydig cells, in the surrounding connective tissue septa. In this figure, maturing sperm appear as dense nuclei with their tails projecting into the lumen of the tubule. The wall of each seminiferous tubule may contain five or more layers of cells. At puberty, when sexual maturity begins, spermatogenic cells in diverse stages of development appear, and the hormone-producing interstitial cells become more prominent in the surrounding septa. Figure 34-4, B, is a high-power micrograph showing a group of typically round interstitial cells clustered between seminiferous tubules. A unique cellular feature often visible in interstitial cells is an elongated rectangular-shaped mass called a crystalloid. Also called Reinke crystalloids, these masses are absent before puberty and then increase in number during the reproductive years into old age. The functional significance of these structures remains uncertain.
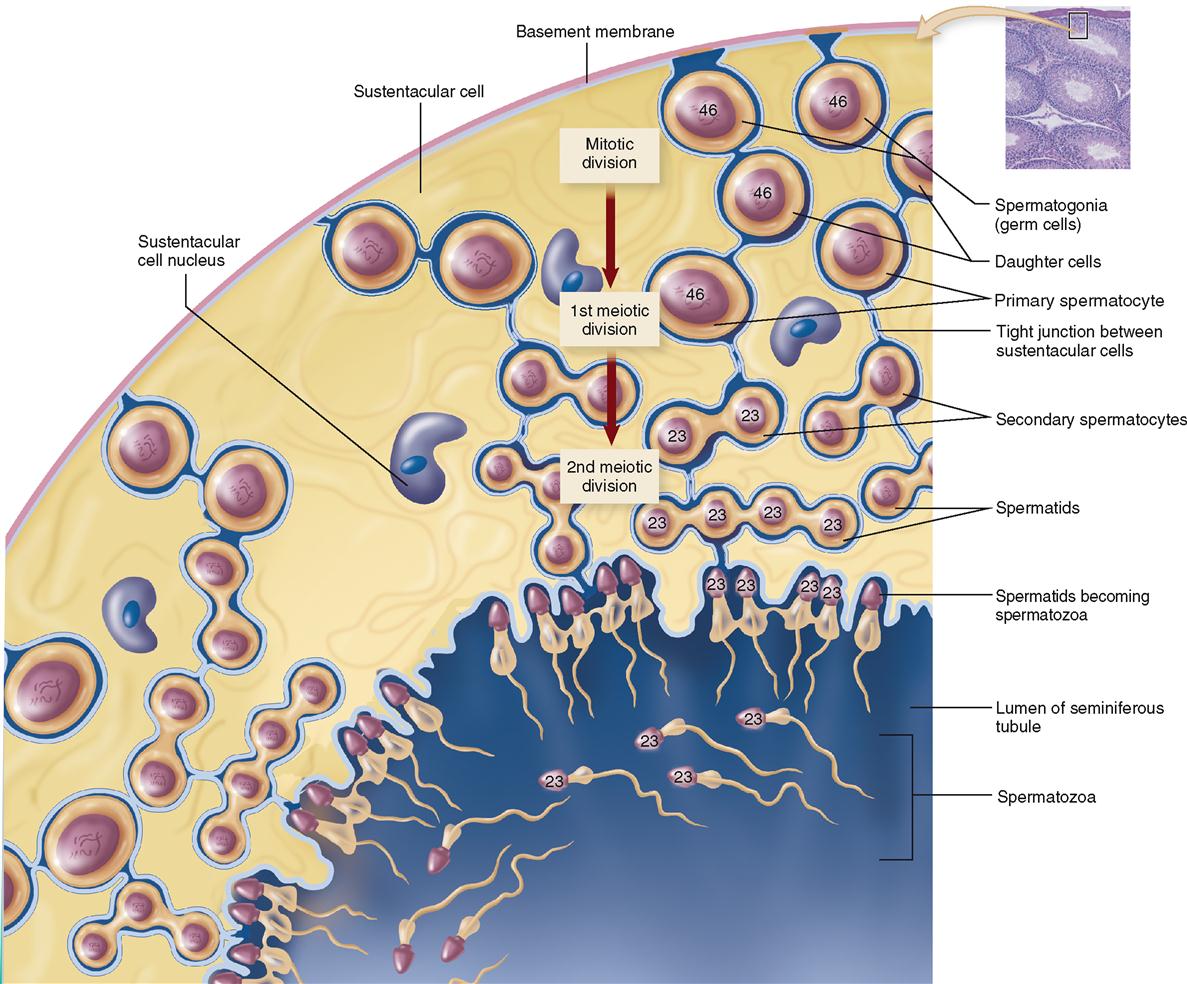
Irregular elongated sustentacular cells have a supportive and regulatory function important for the developing germ cells. Sustentacular cells of the testis are also called nurse cells or Sertoli cells. These cells provide mechanical support and protection for spermatids attached to their luminal surface and are visible in Figure 34-5 within a section of seminiferous epithelium.
Sustentacular cells also secrete the hormone inhibin, which inhibits gonadotropin-releasing hormone (GnRH) in the hypothalamus and follicle-stimulating hormone (FSH) production in the anterior pituitary. A drop in FSH lowers the rate of sperm production. This sets up a negative feedback mechanism in which the supportive sustentacular cells can slow down sperm production to manageable levels if needed.
At sexual maturity, sustentacular cells begin to secrete androgen-binding protein, or ABP, that binds to testosterone, a steroid lipid hormone, to make it more water soluble. This increases the testosterone concentration within the seminiferous tubules. High concentrations of testosterone are required for normal germ cell maturation. Thus sustentacular cells play an important role in spermatogenesis (sperm production).
Sustentacular cells are columnar in shape and extend from the basement membrane to the luminal surface of the seminiferous tubule (Figures 34-5 and 34-6). Tight junctions exist between adjacent sustentacular cells and divide the wall of the tubule into two compartments that house either meiotically active cells near the luminal surface or spermatogonia near the basement membrane.
Tight junctions between sustentacular cells form the blood-testis barrier (BTB). This structure isolates the developing sperm cells, which have active surface antigens different from somatic body cells, from the body immune system. If these antigens were to escape from the tubule epithelium and enter the bloodstream by breaking through the basement membrane, an autoimmune reaction could occur.
Testes Functions
The testes perform two primary functions: spermatogenesis and secretion of hormones.
Spermatogenesis is the production of spermatozoa (sperm), the male gametes, or reproductive cells. The seminiferous tubules produce the sperm. Figure 34-6 shows a cross section of a seminiferous tubule in which two meiotic divisions result in a reduction of chromosomes from 46 in the spermatogonia to 23 in the spermatids and mature sperm. Details of spermatogenesis are discussed in Chapter 36.
Testosterone is the major androgen (masculinizing hormone) produced in humans. Testosterone is a steroid hormone produced by interstitial cells. Another hormone, inhibin, is produced by sustentacular cells of the testis.
Testosterone has several functions. One important group of functions is that it promotes “maleness,” or development and maintenance of male secondary sex characteristics, accessory organs such as the prostate, seminal vesicles, and adult male sexual behavior.
Testosterone also helps regulate metabolism. It is usually classified as an anabolic hormone because it stimulates the protein anabolism. By stimulating protein anabolism, testosterone promotes growth of skeletal muscles (responsible for greater male muscular development and strength). This effect has tempted some athletes to take various synthetic versions of testosterone or testosterone promoters to enhance muscular strength. Testosterone also stimulates bone growth and promotes closure of the epiphyses (see Chapter 8, p. 202). Early sexual maturation leads to early epiphyseal closure. The converse also holds true: late sexual maturation, delayed epiphyseal closure, and tallness tend to go together.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree