Chapter 33 • The Agency for Healthcare Research and Quality (AHRQ) Guideline on Benign Prostate Hyperplasia: Diagnosis and Treatment was developed in 1994 and continues as the seminal resource in this area. Guideline on the management of benign prostatic hyperplasia (BPH). American Urological Association Education and Research 2010. • The AUA has developed an algorithm for evaluation and treatment of patients with BPH. • α-Blockers and 5α-reductase inhibitors are beneficial. • Surgery: Transurethral microwave thermotherapy and transurethral resection are beneficial. • Herbal treatments: β-Sitosterol plant extract and saw palmetto plant extracts are likely to be beneficial; Pygeum africanum and rye grass pollen extract have unknown effectiveness. • First line: α1A-Selective antagonist for patients without HTN; long-acting α1-antagonist for patients with HTN given to reduce symptoms • 5α-Reductase inhibitor given to shrink the size of the prostate; however, 6 months of therapy is required to achieve maximum benefit. • Combination therapy with α1-antagonist plus a 5α- reductase inhibitor
Male Genitourinary Agents
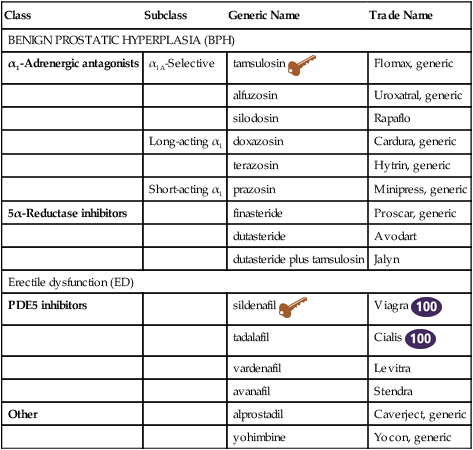
Class
Subclass
Generic Name
Trade Name
BENIGN PROSTATIC HYPERPLASIA (BPH)
α1-Adrenergic antagonists
α1A-Selective
tamsulosin ![]()
Flomax, generic
alfuzosin
Uroxatral, generic
silodosin
Rapaflo
Long-acting α1
doxazosin
Cardura, generic
terazosin
Hytrin, generic
Short-acting α1
prazosin
Minipress, generic
5α-Reductase inhibitors
finasteride
Proscar, generic
dutasteride
Avodart
dutasteride plus tamsulosin
Jalyn
Erectile dysfunction (ED)
PDE5 inhibitors
sildenafil ![]()
Viagra ![]()
tadalafil
Cialis ![]()
vardenafil
Levitra
avanafil
Stendra
Other
alprostadil
Caverject, generic
yohimbine
Yocon, generic
Treatment Principles
Standardized Guidelines
Evidence-Based Recommendations
Cardinal Points of Treatment
Male Genitourinary Agents



