DRUG CLASSES
Androgens
Estrogens
Progestins
PHARMACOLOGY IN PRACTICE

Janna Wong is at the clinic for a sports physical. After the physical, Janna lingers in the examination room. You knock and ask if everything is okay. She asks you to come in and says she would like to get birth control. After reading the chapter, determine how you would respond to Janna’s request.
Male and female hormones play a vital role in the development and maintenance of secondary sex characteristics; they are necessary for human reproduction. Although hormones are naturally produced by the body, administration of a male or female hormone may be indicated in the treatment of certain disorders, such as an advanced-stage cancer, male hypogonadism, and male or female hormone deficiency. Hormones also are used as contraceptives and for treating the symptoms of menopause (Chapter 47).
MALE HORMONES
Male hormones—testosterone and its derivatives—are collectively called androgens. Androgen secretion is influenced by the anterior pituitary gland. Small amounts of male and female hormones are also produced by the adrenal cortex (see Chapter 43). The anabolic steroids are closely related to the androgen testosterone and have both androgenic and anabolic (stimulate cellular growth and repair) activity. Androgen hormone inhibitors reduce the conversion of testosterone into a potent androgen (Fig. 45.1).
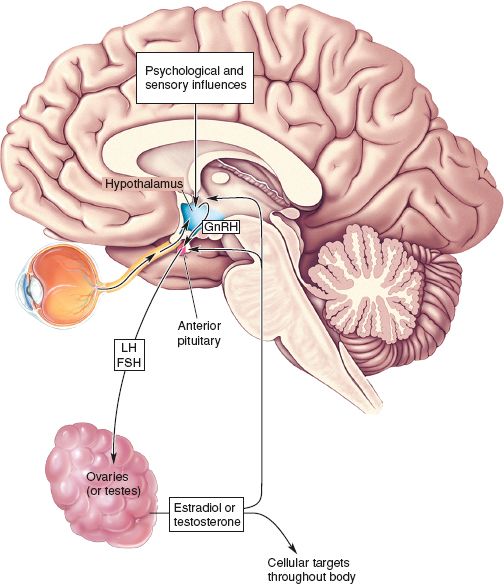
Figure 45.1 The sex hormone relationship to the pituitary and hypothalamus. (From Bear, M. F., Connors, B. W., & Parasido, M. A. [2001]. Neuroscience–exploring the brain [2nd ed.]. Philadelphia: Lippincott Williams & Wilkins.)
Actions
Androgens
The male hormone testosterone and its derivatives cause the reproductive maturation in the adolescent boy. From puberty onward, androgens continue to aid in the development and maintenance of secondary sex characteristics: facial hair, deep voice, body hair, body fat distribution, and muscle development. Testosterone also stimulates the growth in size of the sex organs (penis, testes, vas deferens, prostate) at the time of puberty. The androgens also promote tissue-building processes (anabolism) and reverse tissue-depleting processes (catabolism).
Anabolic Steroids
Anabolic steroids are synthetic drugs chemically related to the androgens. Like the androgens, they promote tissue-building processes. Given in normal doses, they have a minimal effect on the accessory sex organs and secondary sex characteristics.
Uses
Androgen therapy may be given as replacement therapy for the following:
• Testosterone deficiency
• Hypogonadism (failure of the testes to develop)
• Delayed puberty
• Development of testosterone deficiency after puberty
In the female patient, androgen therapy may be used for:
• Postmenopausal, metastatic breast carcinoma
• Premenopausal, hormone-dependent metastatic breast carcinoma
The transdermal testosterone system is used as replacement therapy when endogenous (produced by the body) testosterone is deficient or absent.
Anabolic steroid use includes the following:
• Management of anemia of renal insufficiency
• Control of metastatic breast cancer in women
• Promotion of weight gain in those with weight loss after surgery, trauma, or infections
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Young Males
The use of anabolic steroids to promote an increase in muscle mass and strength has become a serious problem. Anabolic steroids are not intended for this use. Unfortunately, deaths in young, healthy individuals have been directly attributed to the use of these drugs. Young men should be discouraged from the illegal use of anabolic steroids to increase muscle mass.
Adverse Reactions
Androgens
In men, administration of an androgen may result in breast enlargement (gynecomastia), testicular atrophy, inhibition of testicular function, impotence, enlargement of the penis, nausea, vomiting, jaundice, headache, anxiety, male-pattern baldness, acne, and depression. Fluid and electrolyte imbalances, which include sodium, water, chloride, potassium, calcium, and phosphate retention, may also occur.
In women receiving an androgen preparation for breast carcinoma, the most common adverse reactions are amenorrhea, menstrual irregularities, and virilization (acquisition of male sexual characteristics by a woman). Virilization produces facial hair, a deepening of the voice, and enlargement of the clitoris. Male-pattern baldness and acne may also result.
Anabolic Steroids
Virilization in a woman is the most common reaction associated with anabolic steroids, especially when higher doses are used. Acne occurs frequently in all age groups and both sexes. Nausea, vomiting, diarrhea, fluid and electrolyte imbalances (the same as for the androgens, discussed previously), testicular atrophy, jaundice, anorexia, and muscle cramps may also be seen. Blood-filled cysts of the liver and sometimes the spleen, malignant and benign liver tumors, an increased risk of atherosclerosis, and mental changes are the most serious adverse reactions that may occur during prolonged use.
Many serious adverse drug reactions are being reported in healthy individuals using anabolic steroids. There is some indication that prolonged high-dose use has resulted in psychological and possibly physical dependence, and some individuals have required treatment in drug rehab centers. Severe mental changes, such as uncontrolled rage (called “roid rage”), severe depression, and suicidal tendencies; malignant and benign liver tumors; aggressive behavior; increased risk of atherosclerosis; inability to concentrate; and personality changes are not uncommon. In addition, the incidence of the severe adverse reactions cited earlier appears to be increased in those using anabolic steroids for this purpose.
Contraindications and Precautions
The male hormones are contraindicated in patients with known hypersensitivity to the drugs, liver disorders, or serious cardiac disease, and in men with prostate gland disorders (e.g., prostate carcinoma and prostate enlargement). These drugs are classified as pregnancy category X drugs and should not be administered during pregnancy and lactation. Anabolic steroids are contraindicated for use to enhance physical appearance or athletic performance. Anabolic steroids should be used cautiously in older men because of increased risk of prostate enlargement and prostate cancer.
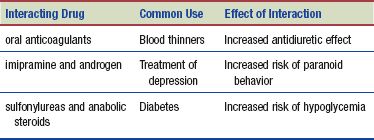
Interactions
The following interactions may occur with the male hormones:
NURSING PROCESS
PATIENT RECEIVING VASOPRESSIN
ASSESSMENT
Preadministration Assessment
Assessment of the patient receiving an androgen or anabolic steroid depends on the drug, the patient, and the reason for administration.
ANDROGENS. In most instances, androgens are administered to the man on an outpatient basis. Before and during therapy, the primary health care provider may order electrolyte studies, because use of these drugs can result in fluid and electrolyte imbalances.
When these drugs are given to the female patient with advanced breast carcinoma, evaluate the patient’s current status (physical, emotional, and nutritional) carefully and record the findings in the patient’s chart. Problem areas such as pain, any limitation of motion, and the ability to participate in the activities of daily living are carefully evaluated and recorded in the patient’s record. You should take and document vital signs and weight. Baseline laboratory tests may include a complete blood count, hepatic function tests, serum electrolytes, and serum and urinary calcium levels. Review these tests and note any abnormalities.
ANABOLIC STEROIDS. Evaluate and document the patient’s physical and nutritional status before starting therapy with anabolic steroids. Note the patient’s weight, blood pressure, pulse, and respiratory rate. Baseline laboratory studies may include a complete blood count, hepatic function tests, and serum electrolytes and serum lipid levels. Review these studies and note any abnormalities.
Ongoing Assessment
The ongoing assessment depends on the reason the drug was prescribed and the condition of the patient. Men receiving an androgen or anabolic steroid are questioned regarding the effectiveness of drug therapy.
Track the weight of the patient with advanced breast carcinoma daily or as ordered by the primary health care provider. Contact the primary health care provider if there is a significant (5-lb) increase or decrease in the weight. Check the lower extremities frequently for signs of edema.
Teach the patient or caregiver to observe for adverse drug reactions, especially signs of fluid and electrolyte imbalance, jaundice (which may indicate hepatotoxicity), and virilization. The primary health care provider must be alerted to any signs of fluid and electrolyte imbalance or jaundice.
When the patient is hospitalized, review vital signs every 4 to 8 hours, depending on the patient’s condition, and then evaluate the patient’s response to drug therapy based on original assessment findings. Possible responses include a decrease in pain, an increase in appetite, and a feeling of well-being.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Chronic Care
When the androgens are administered to a patient with diabetes, blood glucose levels should be measured frequently because glucose tolerance may be altered. Adjustments may need to be made in insulin dosage, oral antidiabetic drugs, or diet.
When anabolic steroids are used for weight gain, the patient is weighed at intervals ranging from daily to weekly. A good dietary regimen is necessary to promote weight gain. Consult the dietitian if the patient eats poorly.
NURSING DIAGNOSES
Drug-specific nursing diagnoses include the following:
 Excess Fluid Volume related to adverse reactions (sodium and water retention)
Excess Fluid Volume related to adverse reactions (sodium and water retention)
 Disturbed Body Image (in the female) related to adverse reactions (virilization)
Disturbed Body Image (in the female) related to adverse reactions (virilization)
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected outcomes of the patient may include an optimal response to therapy, support of patient needs related to the management of adverse reactions, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
If the androgen is to be administered as a buccal tablet, show the patient how to place the tablet and warn the patient not to swallow the tablet but to allow it to dissolve in the mouth. Remind the patient not to smoke or drink water until the tablet is dissolved. Oral and parenteral androgens are often taken or given by injection on an outpatient basis. When given by injection, the injection is administered deep intramuscularly (IM) into the gluteal muscle. Alternatively, a pellet dose is placed under the skin and repeated every 3 to 6 months. Oral testosterone is given with or before meals to decrease gastrointestinal (GI) upset.
Androderm is a transdermal system that is applied nightly to clean, dry skin on the abdomen, thigh, back, or upper arm. This system is not applied to the scrotum. Sites are rotated, with 7 days between applications to any specific site. The system is applied immediately after opening the pouch and removing the protective covering. If the patient has not exhibited a therapeutic response after 8 weeks of therapy, another form of testosterone replacement therapy should be considered. When the system is removed it should be folded in half on itself to prevent accidental dosing if touched.
Testosterone gel (AndroGel) is applied once daily (preferably in the morning) to clean, dry, intact skin of the shoulders and upper arms or abdomen. After the packet is opened, the contents are squeezed into the palm of the hand and immediately applied to the application sites. The application sites are allowed to dry before the patient gets dressed. The gel is not applied to the genitals. Wear gloves if applying to another person; wash hands well with soap and water for self-applications.
Axiron is a liquid preparation that is sprayed into the axillae daily. It is a fast-drying liquid being tested for ease of use.
Monitoring and Managing Patient Needs
Observe the patient receiving an androgen or anabolic steroid for signs of adverse drug reactions.
EXCESS FLUID VOLUME. Sodium and water retention may also occur with androgen or anabolic steroid administration, causing the patient to become edematous. In addition, other electrolyte imbalances, such as hypercalcemia, may occur. Monitor the patient for fluid and electrolyte disturbances.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Older adults with cardiac problems or kidney disease are at increased risk for sodium and water retention when taking androgens or anabolic steroids.
To monitor for fluid retention, make a daily comparison of the patient’s preadministration weight with current weights and make sure to note the appearance of puffy eyelids and dependent swelling of the hands or feet (if the patient is ambulatory) or the sacral area (if the patient is nonambulatory), and report any findings to the primary health care provider. Daily fluid intake and output should be used to calculate fluid balance, too.
DISTURBED BODY IMAGE. With long-term administration of a male hormone, the female patient may experience mild to moderate masculine changes (virilization), namely, facial hair, a deepening of the voice, and enlargement of the clitoris. Male-pattern baldness, patchy hair loss, skin pigmentation, and acne may also result. Although these adverse effects are not life-threatening, they often are distressing and only add to the patient’s discomfort and anxiety. These problems may be easy to identify, but they are not always easy to solve. If hair loss occurs, suggest wearing head coverings such as hats, scarves, or a wig; mild skin pigmentation may be covered with makeup, but severe and widespread pigmented areas and acne are often difficult to conceal. Each patient is different, and the emotional responses to these outward changes may range from severe depression to a positive attitude and acceptance. Work with the patient as an individual, first identifying the problems, and then helping the patient, when possible, to deal with these changes.
Educating the Patient and the Family
Explain the dosage regimen and possible adverse drug reactions to the patient and family and develop a teaching plan to include the following points:
ANDROGENS
 Notify the primary health care provider if any of the following occurs: nausea, vomiting, swelling of the legs, or jaundice. Women should report any signs of virilization to the primary health care provider.
Notify the primary health care provider if any of the following occurs: nausea, vomiting, swelling of the legs, or jaundice. Women should report any signs of virilization to the primary health care provider.
 Oral tablets—Take with food or a snack to avoid GI upset.
Oral tablets—Take with food or a snack to avoid GI upset.
 Buccal tablets—Place the tablet between the cheek and molars and allow it to dissolve in the mouth. Do not smoke or drink water until the tablet is dissolved.
Buccal tablets—Place the tablet between the cheek and molars and allow it to dissolve in the mouth. Do not smoke or drink water until the tablet is dissolved.
 Testosterone transdermal system—Apply according to the directions supplied with the product. Be sure the skin is clean and dry and the placement area is free of hair. Do not store outside the pouch or use damaged systems. Discard systems in household trash in a safe manner to prevent ingestion by children or pets.
Testosterone transdermal system—Apply according to the directions supplied with the product. Be sure the skin is clean and dry and the placement area is free of hair. Do not store outside the pouch or use damaged systems. Discard systems in household trash in a safe manner to prevent ingestion by children or pets.
ANABOLIC STEROIDS
 Anabolic steroids may cause nausea and GI upset. Take this drug with food or meals.
Anabolic steroids may cause nausea and GI upset. Take this drug with food or meals.
 Keep all primary health care provider or clinic visits, because close monitoring of therapy is essential.
Keep all primary health care provider or clinic visits, because close monitoring of therapy is essential.
 Female patients: Notify the primary health care provider if signs of virilization occur.
Female patients: Notify the primary health care provider if signs of virilization occur.
EVALUATION
 Therapeutic response is achieved.
Therapeutic response is achieved.
 Adverse reactions are identified, reported to the primary health care provider, and managed successfully with appropriate nursing interventions:
Adverse reactions are identified, reported to the primary health care provider, and managed successfully with appropriate nursing interventions:
• Adequate fluid volume is maintained.
• Perceptions of body changes are managed successfully.
 Patient and family express confidence and demonstrate an understanding of the drug regimen.
Patient and family express confidence and demonstrate an understanding of the drug regimen.
FEMALE HORMONES
The two endogenous (produced by the body) female hormones are estrogen and progesterone. Like the androgens, their production is under the influence of the anterior pituitary gland. The endogenous estrogens are estradiol, estrone, and estriol. The most potent of these three estrogens is estradiol. Examples of estrogens used as drugs include estropipate (Ortho-Est) and estradiol (Estrace).
There are natural and synthetic progesterones, which are collectively called progestins. Examples of progestins used as drugs include medroxyprogesterone (Provera) and norethindrone (Aygestin).
Actions
Estrogens
Estrogens are secreted by the ovarian follicle and in smaller amounts by the adrenal cortex. Estrogens are important in the development and maintenance of the female reproductive system and the primary and secondary sex characteristics. At puberty, they promote growth and development of the vagina, uterus, fallopian tubes, and breasts. They also affect the release of pituitary gonadotropins (see Chapter 43).
Other actions of estrogen include fluid retention, protein anabolism, thinning of the cervical mucus, and inhibition or facilitation of ovulation. Estrogens contribute to the conservation of calcium and phosphorus, the growth of pubic and axillary hair, and pigmentation of the breast areolae and genitals. Estrogens also stimulate contraction of the fallopian tubes (which promotes movement of the ovum). They modify the physical and chemical properties of the cervical mucus and restore the endometrium after menstruation.
Progestins
Progesterone is secreted by the corpus luteum, placenta, and (in small amounts) adrenal cortex. Progesterone and its derivatives (the progestins) transform the proliferative endometrium into a secretory endometrium. Progestins are necessary for the development of the placenta and inhibit the secretion of pituitary gonadotropins, which in turn prevents maturation of the ovarian follicle and ovulation. The synthetic progestins are usually preferred for medical use because of the decreased effectiveness of progesterone when administered orally.
Uses
Estrogens
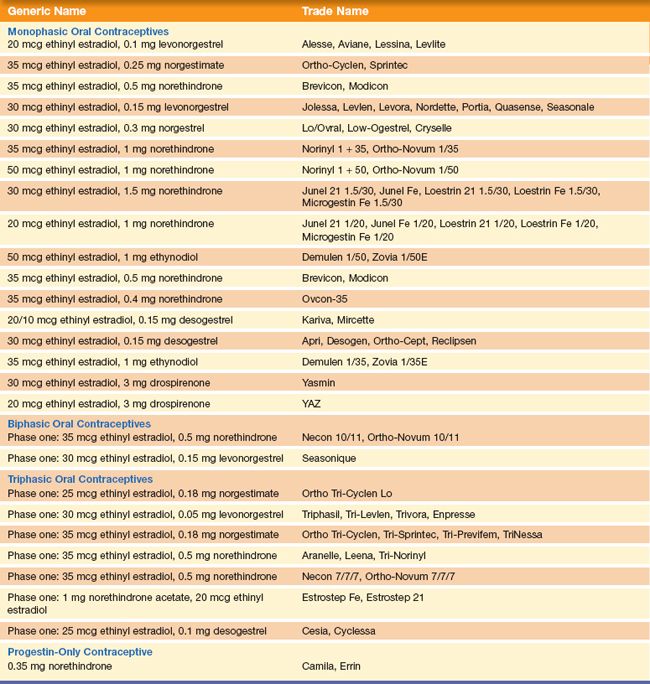
Estrogen is most commonly used in combination with progesterones as a contraceptive agent (Table 45.1) or as estrogen replacement therapy (ERT) in postmenopausal women. ERT and other uses of postmenopausal estrogen are discussed in Chapter 47.
Progestins
Progestins are used in the treatment of amenorrhea, endometriosis, and functional uterine bleeding. Progestins are also used as oral contraceptives, either alone or in combination with an estrogen (see the Summary Drug Table: Male and Female Hormones; see also Table 45.1).
Contraceptive Hormones
Combination estrogens and progestins are used as oral contraceptives. There are three types of estrogen and progestin combination oral contraceptives: monophasic, biphasic, and triphasic. Monophasic oral contraceptives provide a fixed dose of estrogen and progestin throughout the cycle. The biphasic and triphasic oral contraceptives deliver hormones similar to the levels naturally produced by the body (see Table 45.1). Oral contraceptives have changed a great deal since their introduction in the 1960s. Today, lower hormone dosages provide reduced levels of hormones compared with the older formulations, while retaining the same degree of effectiveness (more than 99% when used as prescribed).
Table 45.1 Examples of Oral Contraceptives
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


