Lymphoma
Key Facts
Terminology
Malignancy consisting of clonal population of lymphocytes involving breast
Primary breast lymphoma: Restricted to breast parenchyma and axillary nodes when initially diagnosed
Secondary breast lymphoma: Breast involvement in a patient with systemic disease
Clinical Issues
Lymphomas of the breast are rare; < 0.5% of all breast malignancies
Majority of patients present with palpable breast mass
Unusual presentation mimics inflammatory breast carcinoma due to enlarged axillary lymph nodes
Microscopic Pathology
Majority of breast lymphomas are non-Hodgkin B-cell lymphomas
Hodgkin disease of the breast is very rare
T-cell lymphomas account for < 10%
Top Differential Diagnoses
Inflammatory myofibroblastic tumor (pseudolymphoma, plasma cell granuloma)
Lymphocytic mastopathy (diabetic mastopathy)
Carcinoma
Leukemic breast involvement (granulocytic sarcoma)
Chronic inflammation associated with benign breast conditions
T-cell lymphocytic lobulitis
Intramammary lymph node
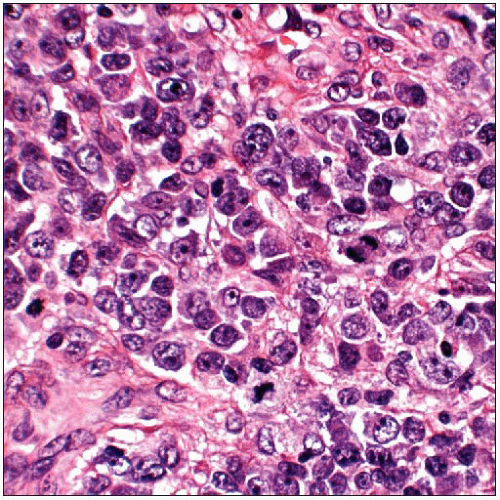
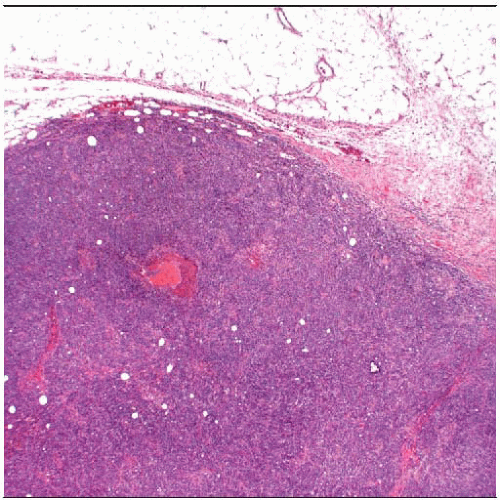 Lymphomas of the breast usually present as circumscribed masses by palpation or by imaging. This lymphoma consists of a solid proliferation of malignant lymphoid cells with a rounded border. |
TERMINOLOGY
Definitions
Clonal population of malignant lymphocytes involving the breast
Primary breast lymphoma: Restricted to breast parenchyma and axillary nodes when initially diagnosed
Should not be prior history of lymphoma with involvement of other sites
Secondary breast lymphoma: Breast involvement in patient with systemic disease
In some cases, intramammary lymph node is involved by the lymphoma
CLINICAL ISSUES
Presentation
Most patients present with palpable breast mass
Rare cases present as mammographic density; associated calcifications may be present in areas of necrosis but are unusual
Borders may be circumscribed or irregular
Lymphomas of breast are rare; < 0.5% of all breast malignancies
Unusual presentation mimics inflammatory breast carcinoma
Breast becomes edematous and enlarged due to lymphatic blockage by involved axillary lymph nodes
Age range is from 12-90 years with bimodal peaks in mid-30s and mid-60s
Treatment
Appropriate treatment is dependent on type of lymphoma
Prognosis
Prognosis is dependent on type of lymphoma
IMAGE FINDINGS
Mammographic Findings
Unusual cases present as mammographic density
Borders may be irregular or circumscribed
No specific imaging findings to identify a mass as lymphoma
Calcifications would be unusual but are rarely associated with foci of necrosis
If patient has systemic lymphoma, bilateral lymph node enlargement may be present
Rare cases present as diffuse breast involvement with trabecular pattern and skin thickening
MACROSCOPIC FEATURES
General Features
Gross mass is usually white to gray with fleshy appearance
Many cases are diagnosed by core needle biopsy
Surgical excision is usually not performed if diagnosis of lymphoma is known
MICROSCOPIC PATHOLOGY
Histologic Features
Majority of breast lymphomas are non-Hodgkin B-cell lymphomas
Hodgkin disease of the breast is very rare and is usually accompanied by nodal involvement
Women who have been treated for Hodgkin disease with mantle radiation are at increased risk for developing breast carcinoma
Majority of breast lymphomas are B-cell lymphomas
Most common type is diffuse large B-cell lymphoma (approximately 60% of cases)
Lymphoplasmacytic lymphoma, extranodal marginal zone B-cell lymphoma, follicle center cell
lymphoma, and lymphoblastic lymphoma have also been reported
Burkitt lymphoma has been reported in young pregnant or lactating women and may be bilateral
These cases occur predominantly in Africa
Only 3 cases of B-cell lymphomas have been reported in association with breast implant
Follicular lymphoma, primary effusion lymphoma, and lymphoplasmacytic lymphoma
T-cell lymphomas are less common (< 10% of all primary breast lymphomas)
ALK1-negative anaplastic large cell lymphoma (ALCL) is rare peripheral T-cell lymphoma
Over 1/2 of cases in the breast have been reported arising adjacent to implant (22 of 30 cases)
Presenting symptom is usually thought to be related to implant, seroma, or infection
Cells are immunoreactive for CD30 (membrane and Golgi) and usually at least 1 T-cell marker
Both silicone and saline implants are associated with cases; used for both cosmetic and reconstructive purposes
Diagnosed 1-23 years after placement of implant
Some cases can be positive for EMA and negative for typical T-cell markers
Molecular studies may be used to demonstrate rearrangement of T-cell receptor gene
Majority of patients undergo chemotherapy, and recurrences are rare
Cutaneous T-cell lymphomas have also been reported in association with breast implants
Presenting symptoms may be exfoliative erythrodermia, erythematous plaques, and skin irritation over implant
DIFFERENTIAL DIAGNOSIS
Inflammatory Myofibroblastic Tumor (IMT)
Synonyms (or closely related lesions) include pseudolymphoma, inflammatory pseudotumor, plasma cell granuloma, xanthomatous pseudotumor, and pseudosarcomatous myofibrohistiocytic proliferation
Consist of infiltrate of mixed inflammatory cells, often with prominent component of plasma cells
Rare cases show preponderance of IgG4 plasma cells and have been termed IgG4-related sclerosing mastitis
Normal germinal centers are often present
Stromal sclerosis with collagen deposition and myofibroblastic proliferation is constant feature
Clonality of stromal cells has been demonstrated in some IMTs
A few cases of IMT have recurred locally
Reports of IMT behaving in malignant fashion may reflect difficulty of distinguishing these lesions from malignant tumors or indicate low probability of progression to malignant neoplasm
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree