Lymphatic System Disorders
Learning Objectives
After studying this chapter, the student is expected to:
1. Identify the structures that comprise the lymphatic system and their general functions.
4. Describe the pathophysiology, signs and symptoms, and treatment of multiple myeloma.
6. Describe the pathophysiology, signs and symptoms, and treatment of Castleman disease
Key Terms
Ann Arbor staging system
Castleman disease
fascia
filaria
hydrocele
lymph
lymphedema
lymphoma
myeloma
Reed-Sternberg cell
spleen
thymus gland
tonsils
Review of the Lymphatic System
Structures and Function
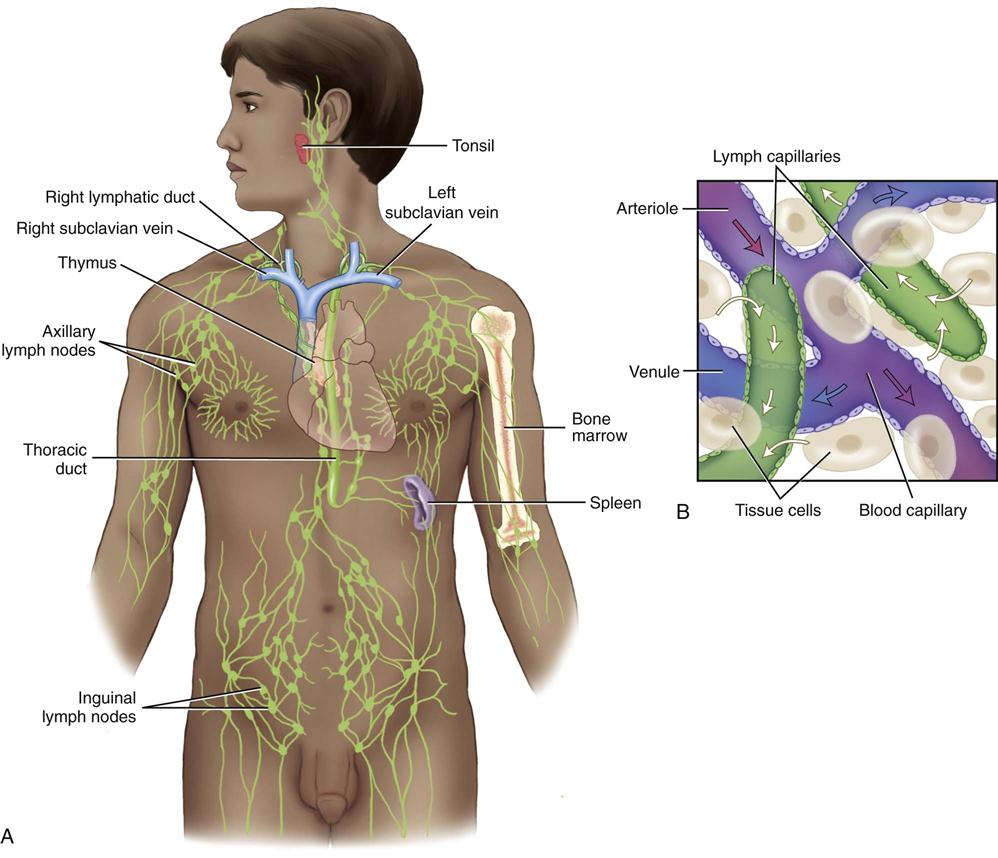
The lymphatic system consists of lymphatic vessels, lymphoid tissue, which includes the palatine and pharyngeal tonsils, lymph nodes the spleen, and the thymus gland (Fig. 11-1). The system functions to return excess interstitial fluid and protein to the blood, to filter and destroy unwanted material from the body fluids, and to initiate an immune response.
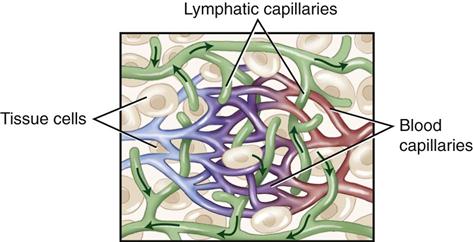
Lymphatic vessels originate as microscopic capillaries that are in direct contact with tissue cells and the interstitial fluid surrounding the cells (Fig. 11-2). These capillaries in turn form branches, then trunks, and finally ducts. These ducts empty into the left and right subclavian veins. Although similar in structure to veins, lymphatic vessels have thinner walls, more valves, and contain nodes at certain intervals. The thinner walls allow an increased degree of permeability allowing large molecules and some particulate matter to be removed from the interstitial spaces. Proteins that eventually accumulate in the interstitial fluids can only be returned to the blood system through the lymphatic vessels. Any condition that might affect normal return from lymphatic vessels to the blood vessels could have a dramatic effect on blood protein concentration and osmotic pressure with serious or fatal results. Lymph capillaries in the villi of the small intestines are called lacteals and have the important function in the absorption of fats and other nutrients that are produced as a result of digestion.
The lymph nodes and lymphoid tissue act as a defense system, removing foreign or unwanted material from the lymph fluid before it enters the general circulation. When infection is present, the regional lymph nodes are often swollen and tender; for example, upper respiratory infection causes enlarged nodes in the neck area. Lymph nodes containing many lymphocytes and macrophages are situated along all lymphatic and blood vessels, ensuring constant filtration and surveillance of body fluids. As well, the lymph nodes are essential to the immune response and the sensitization of B and T lymphocytes (see Chapter 7).
The palatine and pharyngeal tonsils are composed of lymphoid tissue and are located in a ring under the mucous membrane of the mouth and at the back of the throat. These tonsils function as protection against bacterial infection in the area of the openings between the nasal and oral cavities. The tonsils are truly the first line of defense from invasion by external organisms and are therefore often subject to infections such as tonsillitis. Removal of the tonsils when infected has been a controversial topic due to the important immunological role that is played by lymphoid tissue.
The spleen is located on the left side of the abdominopelvic cavity directly below the diaphragm. As with other lymphoid organs, the spleen is surrounded by a fibrous capsule and internally it is divided into compartments (see Fig. 11-2).
The spleen has many functions: defense, hematopoiesis, and red blood cell and platelet destruction, as well as serving as a reservoir for blood.
As part of the body’s defense, the blood passes through the spleen, where macrophages remove microorganisms from the blood and destroy them through phagocytosis.
In the role of hematopoiesis, monocytes and lymphocytes mature and become activated in the spleen and before birth erythrocytes are also formed in the spleen. After birth the spleen is responsible for red blood cell formation only in extreme cases of hemolytic anemia.
The function of red blood cell and platelet destruction is carried out by macrophages that destroy old blood cells and platelets through phagocytosis. These cells also break down the hemoglobin molecules from the destroyed RBCs and salvage the iron and globin portion of the hemoglobin, where they are then returned to the blood circulation for storage in the liver and bone marrow.
Finally, as a blood reservoir the spleen contains a large amount of blood in the pulp and venous sinuses. This blood can be quickly returned to the circulatory system if needed. This large reservoir of blood also damages the spleen, in the form of severe trauma, a serious problem that can result in rapid death; for instance, if a rib punctures the spleen with its significant volume of stored blood.
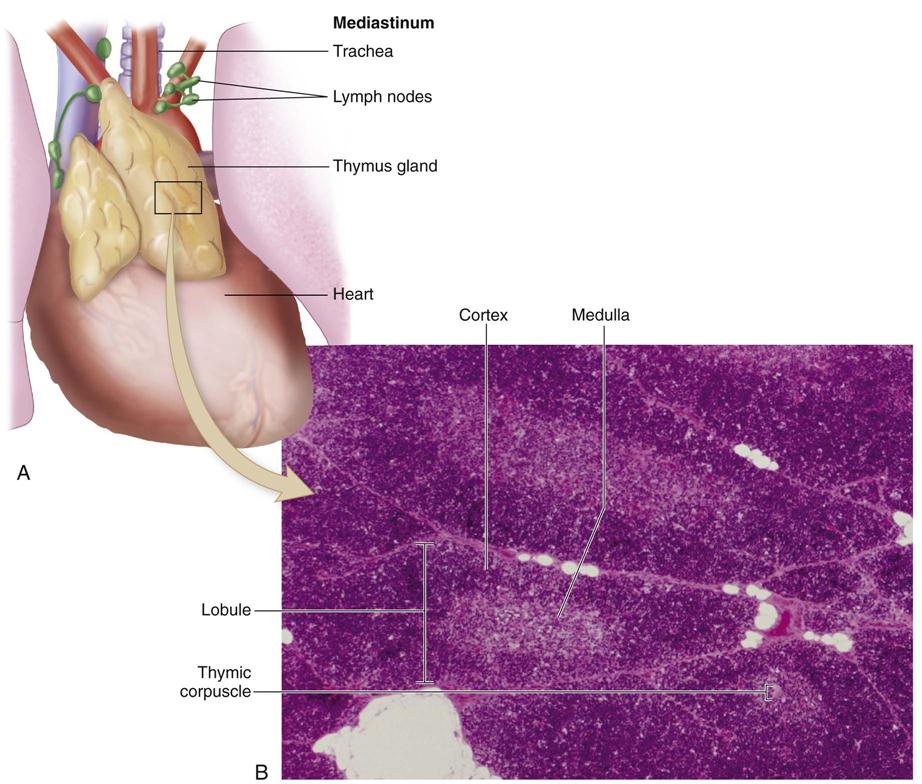
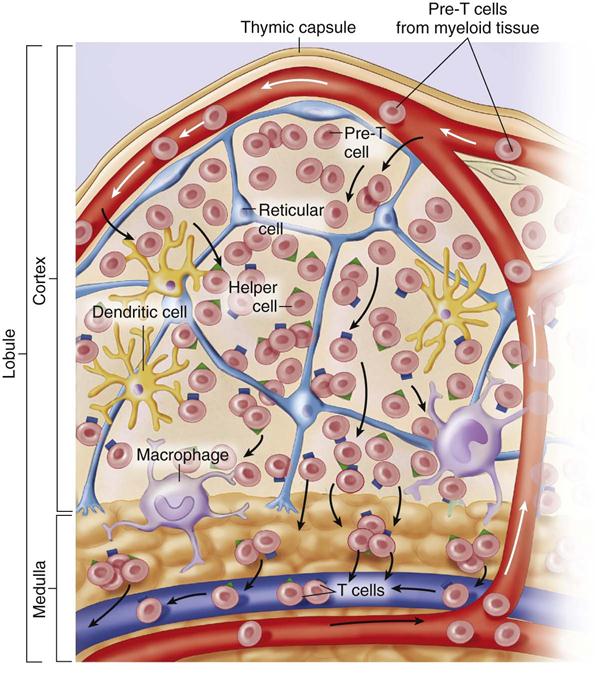
The thymus gland consists of two lobes and is located in the mediastinum, lying in front of the top half of the heart and extending up the neck to the bottom of the thyroid gland. The thymus is covered by a fibrous capsule that extends inward to subdivide the lobes into small lobules (Fig. 11-3).
The thymus plays a critical role as part of the immunity mechanism against infections. In this role it has at least two primary functions: the final site of lymphocyte development before birth and the secretion of hormones after birth, which enable lymphocytes to develop into mature T cells (Fig. 11-4). Because of the T cell’s functions in attacking foreign or abnormal cells and as regulators of immune function, the role of the thymus is extremely important as part of the immune mechanism of the body.
Composition and Production of Lymph
Lymph is the clear, watery, isotonic fluid that is circulated in the lymphatic vessels. Lymph and interstitial fluid (see Chapter 2) are almost chemically identical when taken from the same part of the body. Both also closely resemble blood plasma; however, they usually contain a lower protein percentage than plasma except in the thoracic duct. Here in the thoracic duct, the lymph is protein rich as a result of the outflow into the duct from the liver and small intestine. Interstitial fluid that is not absorbed by the cells or the capillaries tends to accumulate in the interstitial spaces and as this fluid builds it will drain into the lymphatic vessels and become lymph.
Lymphatic Circulation
The lymphatic circulation functions as follows:
1. It begins with blind-ending capillaries containing one-way minivalves at the terminus, into which excess interstitial fluid flows as pressure builds up in the tissues (Fig. 11-5).
2. The lymphatic capillaries join to form larger vessels with valves to ensure a one-way flow of fluid, similar to the network of veins. Flow depends on pressure arising from movement of surrounding skeletal muscle and organs (Fig. 11-6).
6. Lymphatic capillaries in the intestinal villi absorb and transport most lipids as chylomicrons.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree