Lymphangioma and Lymphangiomatosis
David S. Cassarino, MD, PhD
Key Facts
Terminology
Lymphangioma circumscriptum (superficial lymphangioma) (LAC)
Lymphangiomatosis (systemic angiomatosis) (LAS)
Cystic lymphangioma (cystic hygroma)
Deep lymphangioma (cavernous lymphangioma)
Etiology/Pathogenesis
Most cases considered developmental malformations/hamartomas, not true neoplasms
Associated with trisomies and other genetic syndromes, including Turner (cystic hygroma), Noonan, and Maffucci
Clinical Issues
More common in children (6% of benign childhood tumors); present at birth or within 1st 2 years of life
Typically presents as large, slow-growing, painless mass (deep lymphangioma) or as multiple small, grouped, superficial vesicular lesions (LAC)
Excellent prognosis in most cases, although may be fatal if involving mediastinum or internal organs
Recurrence rate high if removal incomplete
Microscopic Pathology
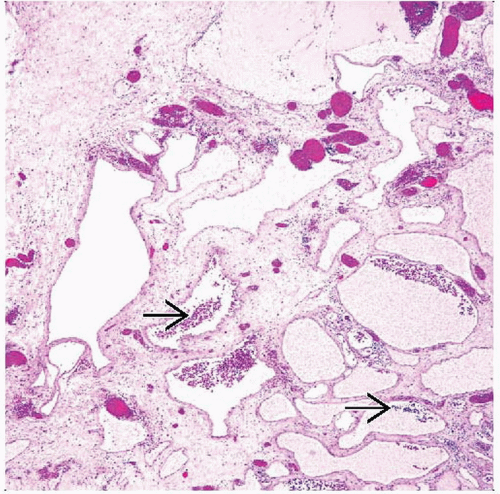
Variably sized anastomosing vascular spaces lined by small, bland endothelial cells
Often contain abundant proteinaceous debris, scattered lymphocytes, and erythrocytes
Walls show stromal fibrosis (older lesions) and may contain smooth muscle
Endothelial cells are small with uniform, bland-appearing, oval to flattened, hyperchromatic nuclei
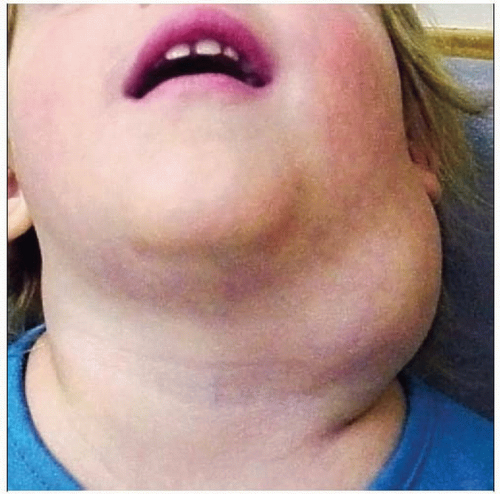 Clinical photograph shows a large deep lymphangioma (cystic hygroma) on the lateral neck of a child. |
TERMINOLOGY
Synonyms
Lymphangioma circumscriptum (superficial cutaneous lymphangioma) (LAC)
Lymphangiomatosis (generalized lymphangioma, systemic angiomatosis) (LAS)
Cystic lymphangioma (cystic hygroma)
Deep lymphangioma (cavernous lymphangioma)
Lymphatic malformation
Definitions
Proliferation of lymphatic vessels; may be
Superficial (lymphangioma circumscription)
Deep (cavernous lymphangioma)
Diffusely involve most organ systems (lymphangiomatosis)
ETIOLOGY/PATHOGENESIS
Developmental Anomaly
Most cases of lymphangioma considered developmental or congenital malformations/hamartomas, not true neoplasms
Maldevelopment of embryonic lymphangiogenesis most likely etiology
Leads to sequestered lymphatics that fail to communicate with normal lymphovascular system
May be due to maternal infections or substance abuse
LAS considered congenital in most cases
Genetics
Associated with genetic syndromes including Turner syndrome (cystic hygroma), Noonan syndrome, Maffucci syndrome, trisomies 13, 18, 21
Mutations in VEGFR-C, VEGFR3, PROX1, FOXC2, and SOX18 genes implicated
Acquired
Rare acquired cases occur in adults
Likely associated with infection or trauma
CLINICAL ISSUES
Epidemiology
Incidence
More common in children: Estimated 6% of benign childhood tumors
Age
Often present at birth or within 1st 2 years of life (approximately 90% of cases)
LAS usually presents within 1st 2 decades of life
Gender
Intraabdominal lymphangiomas have slight male predominance
LAS has no gender predilection
Site
Head and neck most common site for cystic lymphangiomas
Usually posterior triangle but can occur in anterior triangle
Also occur in axillae, abdomen, and internal organs
Cavernous type more frequent in oral cavity, upper trunk, limbs, and abdominal sites
Intraabdominal lymphangiomas occur in mesentery, omentum, and retroperitoneum
LAC: Axillary folds, neck, and trunk are most common sites
LAS: Can affect any organ system, but often involves bones, soft tissues, and skin
Presentation
Cystic mass lesion; may be superfical or deep
Typically presents as large, slow-growing, painless mass (deep lymphangioma) or as multiple small, grouped, superficial vesicular lesions (LAC)
Lymphangiomatosis presents with numerous cystic lesions, both superficial and deep
Soft and fluctuant swellings on palpation
Intraabdominal cases may present with abdominal distension, mass on palpation
May also develop abdominal obstruction, volvulus, and infarction
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree