Lymphadenopathy Secondary to Drug-induced Hypersensitivity Syndrome
Tariq Muzzafar, MBBS
Key Facts
Terminology
DIHS is idiosyncratic host reaction to drug involving T-cell/macrophage activation and cytokine release
Criteria for diagnosis of DIHS include
Suspicion of drug reaction
Eosinophilia &/or atypical lymphocytosis
Failure of at least 2 organs (including skin)
Etiology/Pathogenesis
Pathogenesis of DIHS is poorly understood
Possible hapten-like reaction between drug and unknown host antigen
Onset not correlated with drug dose or serum levels
Many drugs have been associated with DIHS
Anti-epileptic drugs and antimicrobial agents are most common
Clinical Issues
Onset usually 1-8 weeks after initiating drug therapy
Fever, rash, lymphadenopathy in up to 75%
Eosinophilia, atypical lymphocytosis
Microscopic Pathology
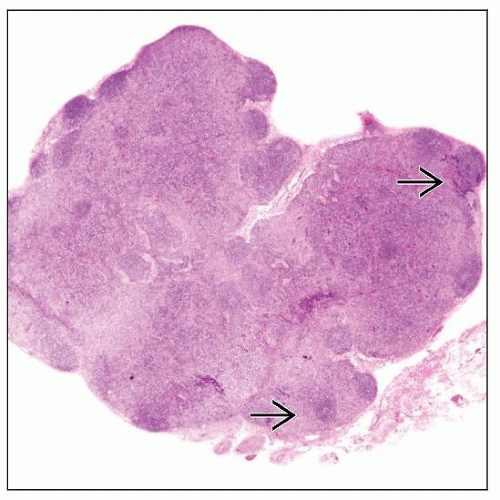
Lymph nodes in patients with acute onset DIHS show
Preserved overall architecture (at least partially)
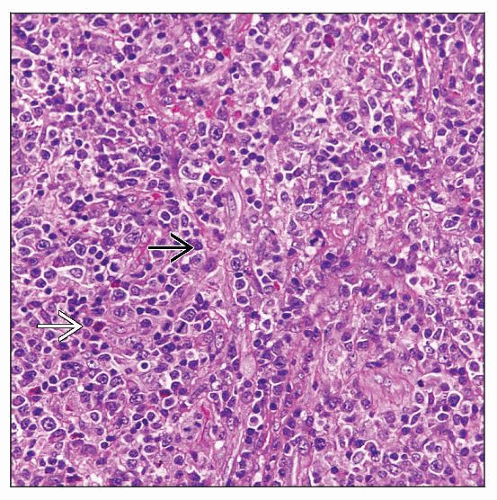
Paracortex expanded by polymorphous infiltrate
Eosinophils(+); immunoblasts can be numerous
± vascular proliferation and necrosis
Follicular hyperplasia is usually present
Diagnostic Checklist
History of drug therapy is required for diagnosis
TERMINOLOGY
Synonyms
Drug-induced hypersensitivity syndrome (DIHS)
Drug reaction with eosinophilia and systemic symptoms (DRESS)
Anticonvulsant hypersensitivity syndrome
Phenytoin or carbamazepine lymphadenopathy
Pseudolymphoma syndrome
Definitions
DIHS is idiosyncratic host reaction to drug therapy involving T-cell and macrophage activation and cytokine release
Criteria for diagnosis of DIHS include
Suspicion of drug reaction
Eosinophilia &/or atypical lymphocytosis
Failure of at least 2 organ systems (including skin)
Organ failure distinguishes DIHS from common drug reactions that usually involve skin
ETIOLOGY/PATHOGENESIS
General Comments
Pathogenesis of DIHS is poorly understood
Possible hapten-like reaction between drug and unknown host antigen
Onset does not correlate with drug dosage or serum levels
Syndrome regresses after drug discontinued
Re-exposure with drug or cross-reacting drug can lead to recurrence
Drug Therapy
Many drugs have been associated with DIHS
Anti-epileptic drugs are most common
Phenytoin, carbamazepine, phenobarbital, primidone, lamotrigine, gabapentin, ethosuximide
Phenytoin and carbamazepine best described and serve as models
Antimicrobial agents also can commonly cause DIHS
Minocycline, β-lactams, sulfonamides, abacavir, nevirapine
Others drugs associated with DIHS include
Allopurinol, dapsone, sulfasalazine, neomercazole, fluindione
For some drugs, their metabolites are direct cause of DIHS
Immunologic Dysregulation
A number of drugs implicated in DIHS have been shown to activate T cells
Most T cells of Th1 type and secrete interferon-γ
Macrophages also appear to be activated in DIHS
Can cause changes similar to low-level hemophagocytic syndrome
High levels of serum ferritin, triglycerides, and lactate dehydrogenase
Elevated levels of C-reactive protein suggest dysregulation of interleukin (IL)-6
IL-18, a proinflammatory cytokine, may be involved in DIHS
IL-18 stimulates T cells, NK cells, and macrophages
Evidence of Impaired Drug Metabolism
Epidermal keratinocytes, mucosal cells, and hepatocytes are
Major sites of oxidative and conjugative processing of xenobiotics, including drugs
Sites of major histocompatibility complex (MHC)-dependent T-cell-mediated immunity for foreign molecules
Aromatic amine drugs
Oxidized by cytochrome P450 isoenzymes into reactive arene oxides
Metabolites further metabolized by epoxide hydrolase
Small subset of DIHS patients may have defective epoxide hydrolase
Loss of detoxification capacity may result in accumulation of reactive epoxide intermediates leading to DIHS
Genetic Factors
DIHS tends to run in families
More common in African-Americans than Caucasians
Predisposing genetic polymorphisms have been reported in patient subsets
May impair metabolism of drugs
May elicit host T-cell or macrophage activation
Possible Role of Immunodeficiency
DIHS is more common in immunocompromised patients
HIV(+) patients have higher frequency of DIHS
Patients with DIHS may have hypogammaglobulinemia and decreased B-cell count
Reactivation of viral infection has been shown
Vitamin D deficiency has been shown in subset of DIHS patients
Vitamin D normally protects against inflammatory and autoimmune conditions
Possible Role of Viruses
Human herpes virus (HHV) 6 reactivation occurs 2-4 weeks after onset of DIHS
May exacerbate symptoms of DIHS
Reactivation of HHV7 has been reported
Viral reactivation is thought to be secondary phenomenon related to immunodeficiency
Delayed Lymphadenopathy
Subset of DIHS patients develop lymphadenopathy after prolonged drug intake
Drug-induced immune dysregulation may allow Bor T-cell clones to emerge
Acute hypersensitivity does not appear to be involved
CLINICAL ISSUES
Epidemiology
Incidence
Risk of DIHS likely depends on specific drug involved
Risk is approximately 1-10 per 10,000 for phenytoin, carbamazepine, phenobarbital
Risk for zonisamide probably similar
Valproic acid rarely implicated
Not reported during monotherapy with topiramate, gabapentin, or levetiracetam
40-70% cross reactivity for 3 aromatic amines: Phenytoin, carbamazepine, and phenobarbital
Age
Wide range; children to elderly
Median age: 4th or 5th decade
Gender
No obvious gender disparity
Slight male predominance in some studies
Site
Peripheral lymph nodes are commonly involved
Cervical and axillary lymph nodes
Other sites: Skin, bone marrow, peripheral blood, liver, heart, kidneys
Presentation
Acute onset is most common form of DIHS
Typically develops 1-8 weeks after initial drug treatment
Rarely onset occurs much later after initiating drug therapy
In previously sensitized patient, onset can occur within 24 hours
Fever occurs in most (if not all) patients at onset
Skin rash is frequent physical finding at onset (˜ 75%)
Initially most skin rashes are patchy and maculopapular
Prurigo is very common
Face, upper trunk, and arms often involved 1st
Periorbital and facial edema are common
Generalized edema can occur
Exfoliative erythroderma also can develop later
Oropharyngeal mucosa is often erythematous
Lymphadenopathy; localized or generalized; in up to 75% of patients
Often tender
Hypotension can develop in ˜ 30-40% of patients
Subset of patients have evidence of cardiac dysfunction
Hepatitis common
May be associated with hepatomegaly and splenomegaly
Severe cases can be fatal
Interstitial pneumonitis, interstitial nephritis, or arthritis in small patient subsets (˜ 20%)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree