Lymph-Vascular Invasion
TERMINOLOGY
Abbreviations
Lymph-vascular invasion (LVI)
Synonyms
Lymphatic/vascular invasion
Lymphovascular invasion
Vascular invasion
Definitions
Tumor emboli within peritumoral vascular channels (lymphatics and capillaries)
EPIDEMIOLOGY
Incidence
Reported to be present in 10-90% of invasive breast carcinomas
Incidence varies with patient population and diagnostic criteria
CLINICAL IMPLICATIONS
Clinical Risk Factors
Pathologic factors and risk
Breast carcinomas metastasize via both lymphatics and blood vessels
Lymphatic channels are main route for metastasis (in approximately 2/3 of cancers)
LVI is associated with the presence of lymph node metastases
In a subset of breast carcinomas, metastasis is via blood vessels
Not associated with lymph node metastasis
Fewer vessels are involved, and tumor emboli are smaller than those in lymphatics
Approximately 20-30% of node-negative patients develop distant metastases, presumably due to blood vessel invasion
Spindle cell carcinomas, phyllodes tumors, and angiosarcomas are examples of tumors that rarely involve lymph nodes
May be specific molecular signatures associated with pattern of metastasis
Difficult to distinguish lymphatics from small capillaries
Immunoperoxidase markers cannot always identify type of vessel with confidence
Many patients have both lymphatic and blood vessel involvement
For practical purposes, no need to distinguish lymphatic from capillary to diagnose LVI
Peritumoral LVI has independent prognostic significance
Associated with increased risk of axillary lymph node metastasis as well as local and distant recurrence
Intratumoral LVI likely has little or no prognostic significance
Difficult to distinguish LVI within confines of invasive carcinoma from retraction artifact
Tumor in vascular channels that has not traveled beyond the tumor is less likely to be prognostically significant
Not associated with lymph node metastasis
Recommended that intratumoral LVI alone not be reported
LVI is more frequently associated with breast cancers demonstrating other aggressive features
High Ki-67 score
High histologic grade
Absence of hormone receptor expression
Prognostic factors and risk
LVI is associated with significantly increased risk for tumor recurrence or death independent of axillary node status
Recurrence for stage I (node-negative) invasive breast cancer increases from 22% without LVI to 38% with LVI
Presence of LVI increases risk for metastases in additional nodes if sentinel node is positive
LVI may be associated with resistance to chemotherapy
Therapeutic Implications
LVI is useful in therapeutic decision making, particularly for node-negative patients with small cancers
MICROSCOPIC FINDINGS
General Features
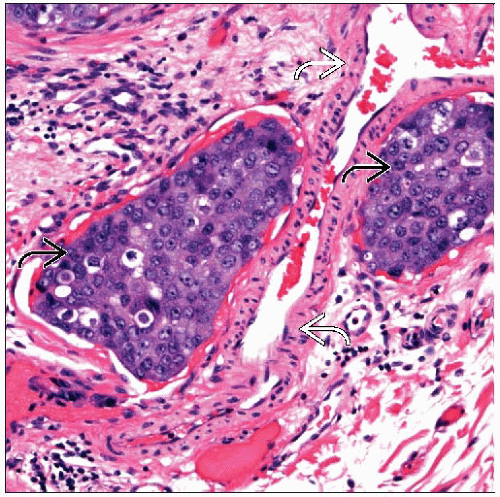
Strict criteria for LVI aid in making correct diagnosis
LVI should be assessed at periphery, beyond advancing border of invasive carcinoma
Majority of LVI will be within 1-2 mm of edge of invasive carcinoma
If foci are only seen at greater distance, they are more likely to be artifactual
Tumor emboli should be within vascular channels lined by a single layer of endothelial cells
Nuclei of endothelial cells are not always apparent in all spaces
Lymphatics and small capillaries are not surrounded by muscular layer or elastica
Red blood cells may be present in either structure
Large arteries or veins with muscular walls are rarely involved
Larger vessels can be identified with elastic stains
Elastin fibers are also present surrounding ducts and should not be mistaken for blood vessels
IHC for smooth muscle markers is also helpful for identifying larger vessels
Tumor emboli usually do not completely conform to shape of space
If space is completely filled by tumor cells, it is difficult to recognize as LVI
Tumor cells within a larger space of different shape favors LVI
In retraction artifact, shape of tumor and space are usually identical
Spaces may be elongated and sinusoidal as lymphatic passes in and out of plane of section
Branch points (Y-shaped focus) are more likely to be due to LVI than invasive carcinoma
Recognizing anatomic distribution of lymphatics aids in their identification
Lymphatics and small blood vessels usually run together between lobules
Lymphatics are often seen adjacent to small arteriole and vein
Lymphatics may cup around arteriole
Immunohistochemistry
Can be used to identify endothelial cells
Clinical significance of LVI detected only by IHC and not seen after careful review of H&E sections remains unclear
CD31 and CD34 are positive in endothelial cells
CD31 is predominantly positive in blood vessels
CD34 is positive in blood vessels and also in some lymphatics
CD34 is also positive in stromal cells, which limits its usefulness for distinguishing LVI from retraction artifact
Podoplanin is a mucin-type transmembrane glycoprotein 1st described in lymphatic endothelial cells
Monoclonal antibody D2-40 (against podoplanin) selectively detects lymphatic vessels
Most sensitive and specific marker for lymphatic endothelial cells
Pattern should be strong and linear
Endothelial cells of arteries, veins, and capillaries should not be positive
Myoepithelial cells can be positive for D2-40; therefore, not very useful to distinguish DCIS from LVI
Pattern in myoepithelial cells is often weak, granular, and membranous
Use of D2-40 can increase number of foci of LVI detected by 20% over H&E sections alone
D2-40 may also be positive in basal-like carcinomas, squamous cell carcinomas, and angiosarcomas
Use of this marker to evaluate LVI in these tumor types may be more difficult
Positive Lymph Node in Absence of LVI
Usually occurs when there is 1 or only a few positive lymph nodes
Frequently occurs with discohesive (e.g., lobular) carcinomas
Cohesive carcinomas grow as contiguous plugs of tumor within lymphatics with adhesion to vessel wall
Discohesive carcinomas are present as dispersed cells, not adherent to wall, and may only be present transiently
In some cases, extensive LVI can be mistaken for DCIS
Diagnosis of LVI should not be made based only on presence of lymph node metastases
Negative Lymph Nodes in Presence of LVI
LVI may be present although no metastases are present in lymph nodes
Reported in 5-10% of node-negative carcinomas
Lymphatic drainage may be toward internal mammary nodes, particularly for medially located carcinomas
Metastatic foci may not have reached axillary nodes or may not be able to establish viable growth in nodes
DIFFERENTIAL DIAGNOSIS
DCIS
Both LIV and DCIS appear as circumscribed nests of tumor cells
Stromal reaction is usually absent surrounding LVI and may be absent or minimal surrounding DCIS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree