Lymph Node Metastases
TERMINOLOGY
Abbreviations
Individual tumor cells or individual tumor cell clusters (ITCs)
ETIOLOGY/PATHOGENESIS
Histogenesis
Majority of breast cancers metastasize via lymphatics and likely also metastasize via blood vessels
A subgroup of cancers metastasize only via blood vessels and do not involve lymph nodes
Spindle cell carcinomas, high-grade phyllodes tumors, and sarcomas typically metastasize without involving regional nodes
Major outflow of lymph from the breast is to 1 or 2 sentinel lymph nodes in the axilla
Negative sentinel node is predictive of absence of metastases in remainder of axillary nodes in ˜ 90% of patients
Nonsentinel node metastases occur in up to 10% of patients with a negative sentinel node
Some cases are due to sentinel node being replaced by tumor, not allowing uptake of radioactive tracer or dye
Some cases may be due to aberrant drainage patterns in a few patients
Some cases are due to failure of mapping technique
Rare cancers metastasize via lymphatics draining to other nodal basins, such as internal mammary nodes
Intramammary nodes may be involved by carcinoma but are rarely, if ever, the sentinel node
CLINICAL IMPLICATIONS
Clinical Significance of Lymph Node Metastases
Macrometastases (≥ 0.2 cm) are prognostically significant for overall and disease-free survival
0.2 cm was originally chosen as size that could be measured with a ruler and did not require special measuring devices
0.2 cm is also size that can be reliably detected by thinly slicing nodes and examining all slices with 1 H&E section
Prognosis is diminished with each additional lymph node metastasis
Difference in survival between 0 positive nodes and 1 positive node is similar to difference for each additional node; there is no sharp drop-off in survival
Total number of involved lymph nodes should be counted and reported
Nodes with ITCs are not included in total node count
Axillary nodes and intramammary nodes are counted together
Number of uninvolved nodes and ratio of positive/negative nodes also has prognostic significance
Very important to always identify as many separate nodes as possible
When 1 sentinel node is involved, number of additional negative nodes may be used to determine need for additional node dissection
Extranodal invasion is an adverse prognostic factor
Not extensively studied due to rarity of this finding
Extensive extranodal invasion correlates with clinical finding of matted axillary nodes
It may be necessary to estimate number of nodes present when extensive
May be used in decisions on benefit of axillary radiation
Smaller metastases (micrometastases and ITCs) have a very small effect on prognosis
Survival is diminished by < 3% at 5-10 years as compared with node-negative women
No practical technique can detect all small metastases; hundreds of slides per lymph node would need to be examined
Clinical impact is too small to uniformly recommend studies to detect a subset of these metastases
No currently used clinically feasible protocols detect all ITCs that may be present in nodes
Effect on prognosis is so small that treatment recommendations should be based on their presence with caution
Cancers associated with small metastases often have other adverse prognostic factors that would be indications for systemic treatment
Rare cancers drain to internal mammary nodes
These nodes lie below ribs and sternum and are difficult to approach surgically
If radiologic findings are inconclusive as to whether these nodes are involved, fine needle aspiration (FNA) to establish positivity may be attempted
Lymph node metastases after neoadjuvant treatment are an adverse prognostic finding
Indication of an incomplete response to therapy
Small residual metastases are as prognostically important as larger metastases
Although ITCs are classified as pN0(i+), this finding is not considered a pathologic complete response (pCR)
Response in nodal metastases has more prognostic significance than the response of cancer in the breast
Degree of response of metastases to treatment should be reported (e.g., presence and extent of fibrosis)
Some metastases can resolve completely after treatment without leaving a fibrous scar
Alternatively, some nodes not involved by metastasis can have small areas of fibrosis
Therefore, if nodes are free of carcinoma after treatment, it cannot be determined with certainty whether or not they were involved prior to treatment
pCR in nodes cannot be determined with certainty unless a metastasis has been documented before treatment by either fine needle aspiration or core needle biopsy
Sentinel node biopsy after neoadjuvant treatment is less accurate than in absence of treatment
Response to treatment is not uniform across all nodes
Metastasis in sentinel node may completely respond to treatment, but this does not ensure that all metastases to nonsentinel nodes will also have undergone a complete response
Documenting metastatic disease to lymph nodes is necessary to accurately classify patients for neoadjuvant trials and to derive the most information about treatment response
Palpable nodes may be sampled by FNA or core needle biopsy
Nonpalpable but enlarged nodes can be identified by ultrasound and sampled by needle biopsy
If no enlarged nodes are identified, sentinel node biopsy can be used to document a negative node; no additional nodal sampling is then necessary after treatment
MACROSCOPIC FINDINGS
General Features
Gross appearance
Large metastases efface surface of lymph node and appear as firm white nodule(s)
Gross size of metastasis should be noted
Sampling may be limited to 1 section most likely to show extranodal invasion
Metastases < 1 cm may not be grossly evident
Number of nodes examined and number of positive nodes must be determined as accurately as possible
Each node should be separately identified
Nodes should be inked with different colors if slices from more than 1 node will be placed in same cassette
Size &/or shape of node is not reliable to identify different nodes when submitted together
If extensive extranodal invasion is present, it may be difficult to determine number of positive nodes
Attempt must be made to identify as many separate nodes as possible
Specimen Handling
Sentinel lymph nodes
Should be identified as “sentinel” by surgeon
May be identified by blue dye, radioactive tracer, or both
Success rate for finding sentinel node is highest when both methods are used
Majority of sentinel nodes will be both blue and hot (i.e., radioactive)
˜ 5% of sentinel nodes are blue but not hot; these are likely true sentinel nodes
˜ 10-40% of nodes may be hot but not blue; these nodes rarely contain metastases and are likely due to tracer being taken up by nonsentinel lymph nodes
Number of sentinel nodes identified may determine need for completion axillary dissection
Therefore, each node must be separately identified and evaluated
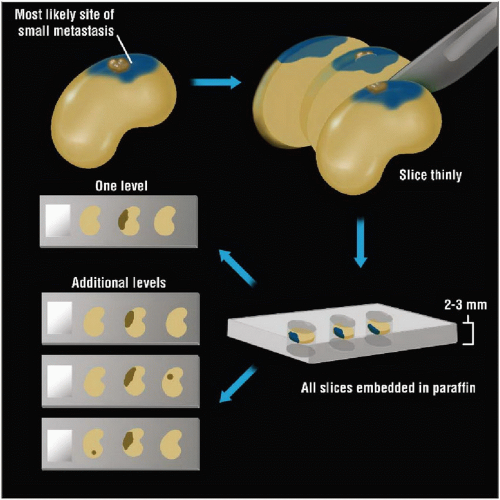
Small metastases are at pole of lymph node identified by dye in > 80% of cases
Metastasis can be missed if a node is bisected and only 1/2 of node examined
20-40% of macrometastases can be missed if only 1/2 of node examined
Examination of entire node histologically is recommended in order to find all macrometastases
Ancillary studies (additional levels, IHC) will detect additional micrometastases and ITCs
Smaller metastases have very minimal impact on survival
Additional studies beyond H&E evaluation are not currently required for AJCC staging
Ancillary studies are not currently recommended by the College of American Pathologists or the Association of Directors of Surgical Pathology
Nonsentinel lymph nodes
Each node should be sliced thinly
All nodal tissue should be examined microscopically
Ancillary studies are not required and are not recommended
Methods of finding nodes
“Squash” method
Fatty tissue is compressed and flattened by firmly pressing with finger or thumb
Lymph nodes are firm nodules that cannot be compressed by firmly pressing on tissue
This method can find nodes as small as 1-2 mm in size
Clearing methods
Special solutions cause adipose tissue to become transparent
Additional very small nodes may be found
Solutions generally contain toxic chemicals and are time-consuming to use
Clinical significance of very small nodes found after using clearing methods and careful gross examination is unclear
Bouin solution
Adipose tissue is dyed yellow, and nodes appear white when sectioned
Bouin adversely affects immunoreactivity for hormone receptors
Bouin fixative should not be used on any tissue for which hormone receptor studies might be required
Bouin also degrades DNA and should not be used for tissue that may be used for FISH or other DNA/RNA studies
After node is identified, it should be dissected out of tissue to avoid counting multiple slices as multiple nodes
If lymph nodes are not found, or very few are found, examination of remaining tissue should be considered
Nodes with extensive fatty replacement may be difficult to see grossly
Small nodes may be found near vessels
REPORTING CRITERIA
AJCC/UICC N Classification
N classification is based solely on axillary lymph nodes in majority of breast cancers
In rare cases in which other nodal groups are involved at presentation (e.g., internal mammary nodes, infraclavicular or level III nodes), additional N categories apply
Intramammary nodes are included in total count with axillary nodes
At least 1 metastasis must be a macrometastasis for classification as pN1a or higher
Nodes with ITCs are not included in total count of positive nodes
pN0: No metastases are detected in nodes
pN0(i+): Isolated tumor cells are present
Largest cohesive cluster measures ≤ 0.02 cm
No more than 200 cells should be present on any single complete cross section of node
pN0 (i-) is undefined term, as no technique completely eliminates possibility of ITCs
pN0(mol+): Molecular test (generally RT-PCR) is positive, but no metastases are seen on H&E
Size of metastasis cannot be determined with certainty
Macrometastases can be missed depending on amount of tissue apportioned for assay
False-positive results occur with RT-PCR in 5% or more of patients
pN1mi: A micrometastasis is present
Defined as > 0.02 cm or more than 200 cells but ≤ 0.2 cm
PN1a: Metastases in 1-3 axillary lymph nodes
PN2a: Metastases in 4-10 axillary lymph nodes
PN3a: Metastases in > 10 axillary lymph nodes
(sn) Modifier
Modifier “(sn)” was introduced in the AJCC 6th edition to indicate cases in which nodal classification was based only on sentinel nodes
In these cases, only 1 or 2 nodes may be examined, and actual nodal classification could be different if all axillary nodes were examined
In some cases, however, several sentinel nodes are removed such that the number is similar to a low axillary dissection
In the 7th edition, modifier (sn) allowed only if ≤ 5 sentinel and nonsentinel nodes are removed
ANCILLARY STUDIES
Use of Ancillary Studies
Ancillary studies for lymph node evaluation are not required or recommended by AJCC, CAP, or ADASP
Lymph nodes can be classified for staging using a representative H&E slide
In selected cases, additional levels or IHC studies can be helpful to identify and classify cells that are not clearly metastatic carcinoma by histologic appearance
Multiple H&E Levels
Recommended that nodes be thinly sliced at 0.2-0.3 cm and that all slices be examined microscopically
This method will detect > 95% of macrometastases (> 0.2 cm)
Additional levels deeper through paraffin block detect micrometastases and ITCs
Routine “levels” are generally only 10-20 microns apart
Levels used to detect additional metastases must be equally spaced in block of tissue and typically must be hundreds of microns apart
Need for widely spaced levels must be specifically communicated to histotechnologist
Number of levels and spacing of levels determine size of metastases that can be detected
1 level: ≥ 0.2 cm metastases
3 equally spaced levels: ≥ 0.1 cm metastases
6 equally spaced levels: ≥ 0.05 cm metastases
Immunohistochemistry (IHC)
IHC for keratin or other epithelial markers can be used to identify cells difficult to classify as epithelial cells on H&E
Cells should have morphology of breast carcinoma before classifying them as cancer cells
Plasma cells may be positive for many IHC markers
Reticulin cells can be positive for keratin CAM5.2
Reticulin cells have spindly processes, encircle germinal centers, and do not have epithelial cell morphology
Keratin positive cells can be artifactually transferred to slides but are usually out of plane of section
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree