DRUG CLASSES
ronchodilators
• Short-acting beta-2 (β2) (adrenergic) agonists (SABAs)
• Long-acting beta-2 (β2) (adrenergic) agonists (LABAs)
• Xanthine derivative
• Cholinergic blocking (anticholinergic)
Antiasthma
• Inhaled corticosteroids (ICSs)
• Mast cell stabilizer
• Leukotriene modifier and immunomodulator
The term chronic obstructive pulmonary disease (COPD) includes the disorders of asthma, chronic bronchitis, chronic obstructive bronchitis, and emphysema, or a combination of these conditions. The patient with COPD experiences dyspnea (difficulty breathing) with physical exertion, has difficulty inhaling and exhaling, and may have a chronic cough. All of these disorders interfere with the exchange of gases in the lung alveoli.
More than 22 million Americans have asthma, which is a chronic inflammatory disease causing spasmodic constriction of the bronchi. It is one of the most common chronic diseases of childhood, affecting an estimated 6 million children.
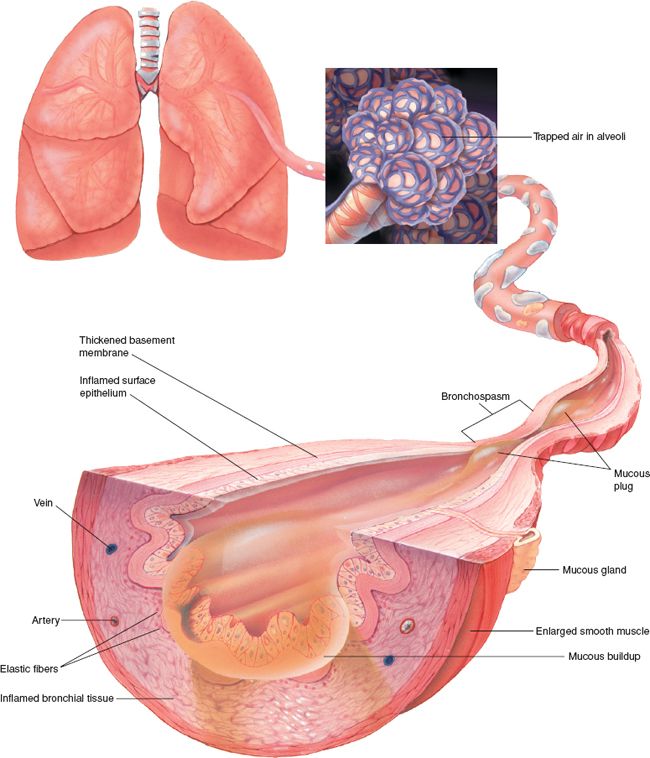
During the inflammatory process, a large amount of histamine is released from the mast cells of the respiratory tract. The lung bronchi constrict, becoming hyperresponsive to the bronchoconstriction, and edema occurs. With asthma, the airways become narrow, the muscles around the airways tighten, the inner lining of the bronchi swell, and extra mucus clogs the smaller airways (Fig. 32.1). Characterized by recurrent attacks of dyspnea and wheezing, this breathlessness causes the patient to experience anxiety.
Patients with asthma may experience periods of exacerbation of symptoms alternating with periods of normal respiratory function. The period of exacerbation may begin abruptly, often triggered by exercise or cold air, but usually is preceded by increasing symptoms over the previous several days:
PHARMACOLOGY IN PRACTICE

Lillian Chase, a 36-year-old woman who had a breathing problem over the weekend, was seen in the emergency department of the local hospital. You are seeing her in the clinic for her follow-up visit. At the end of the chapter, review the medication order and compare it with the established guidelines for her self-management of asthma.
Figure 32.1 Bronchus airflow obstruction in asthma. (Courtesy of Anatomical Chart Co.)
• Cough (worse at night or early morning)
• Generalized wheezing (a whistle or squeaking sound on inspiration or expiration)
• Generalized chest tightness (may feel like someone is sitting on the chest)
• Dyspnea (shortness of breath or feeling of breathlessness)
• Tachypnea (rapid breathing)
These symptoms indicate that inflammation is occurring in the lungs. Stimulation of the sympathetic nervous system, the fight-or-flight response (as described in Chapter 24), is the body’s reaction to the inflammation.
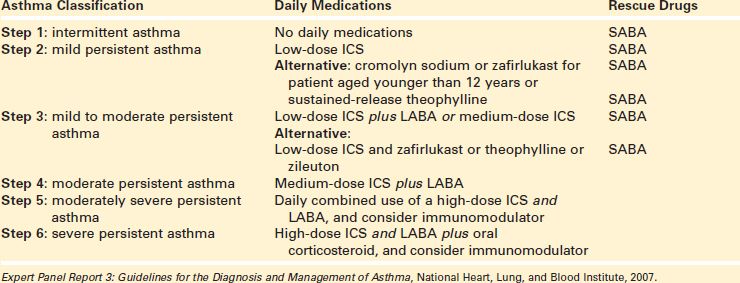
Asthma medications are categorized into two major groups: (1) long-term control medications and (2) quick-relief medications used to treat acute air flow obstruction. The long-term management of asthma uses a stepwise approach (Display 32.1), meaning that medications and their frequency of administration are adjusted according to the severity of the patient’s asthma. The most effective long-term control medications are those that reduce inflammation, with inhaled corticosteroids (ICSs) being the first-line intervention. Quick-relief medications include inhaled short-acting beta-2 (β2) (adrenergic) agonists (SABAs) and oral steroids.
Bronchodilators are the mainstay of treatment for many chronic pulmonary disorders. SABA bronchodilators are drugs used to relieve bronchospasm associated with respiratory disorders, such as bronchial asthma, chronic bronchitis, and emphysema. These conditions are progressive disorders characterized by a decrease in the inspiratory and expiratory capacity of the lung. Examples of β2 agonist bronchodilators include albuterol (Ventolin), epinephrine (Adrenalin), salmeterol (Serevent), and terbutaline. Along with the bronchodilators, several types of drugs are effective in treating asthma. These include ICSs, mast cell stabilizers, leukotriene formation inhibitors, leukotriene receptor agonists, and immunomodulators.
The two major types of bronchodilators are the β2-adrenergic agonists (or sympathomimetics) and the xanthine derivatives. The cholinergic blocking drug ipratropium bromide (Atrovent) is used for bronchospasm associated with COPD, chronic bronchitis, and emphysema in emergent situations. Ipratropium is featured in the Summary Drug Table: Lower Respiratory System Drugs. Chapter 27 provides specific information concerning the cholinergic blocking (anticholinergic) drugs.
Adrenergic Bronchodilators
When alpha (α)-adrenergic receptors (the sympathetic system) in the lungs are stimulated, bronchoconstriction results. The opposite, bronchodilation, occurs when β-adrenergic receptors are stimulated. Some theories propose that asthma is a lack of β-adrenergic stimulation. Many of the adrenergics used as bronchodilators have the subclassification of β2 receptor agonists, which are either short acting (e.g., albuterol and terbutaline) or long acting (e.g., salmeterol). Additional information concerning the various adrenergic drugs is given in the Summary Drug Table: Lower Respiratory System Drugs.
Display 32.1 Step Care Approach for Managing Asthma in Adults and Youth 12 Years and Older
Actions
When bronchospasm occurs, there is a decrease in the lumen (or inside diameter) of the bronchi, which decreases the amount of air taken into the lungs with each breath. A decrease in the amount of air taken into the lungs results in respiratory distress. Use of a bronchodilating drug opens the bronchi by relaxing the smooth muscles and allows more air to enter the lungs, which, in turn, completely or partially relieves respiratory distress.
Uses
The β2-adrenergic drugs (which mimic the sympathetic nervous system) are used in the treatment of chronic respiratory problems due to bronchoconstriction, such as:
• Bronchospasm associated with acute and chronic bronchial asthma
• Exercise-induced bronchospasm (EIB)
• Bronchitis
• Emphysema
• Bronchiectasis (chronic dilation of the bronchi and bronchioles)
• Other obstructive pulmonary diseases
Adverse Reactions
Cardiovascular System Reactions
• Tachycardia, palpitations, or cardiac arrhythmias
• Hypertension
Other Reactions
• Nervousness, anxiety
• Insomnia
When these drugs are taken by inhalation, excessive use (e.g., more than the recommended dose times) may result in paradoxical bronchospasm.
 NURSING ALERT
NURSING ALERT
Long-acting β2 (adrenergic) agonists (LABAs; e.g., salmeterol) may increase the risk of asthma-related death. ICSs should be considered first for long-term control of asthma.
Contraindications
The adrenergic bronchodilators are contraindicated in patients with known hypersensitivity to the drug, cardiac arrhythmias associated with tachycardia, organic brain damage, cerebral arteriosclerosis, and narrow-angle glaucoma. Salmeterol is contraindicated during acute bronchospasm.
Precautions
The adrenergics are used cautiously in patients with hypertension, cardiac dysfunction, hyperthyroidism, glaucoma, diabetes, prostatic hypertrophy, and a history of seizures. The adrenergic drugs are also used cautiously during pregnancy and lactation (all are in pregnancy category C, except terbutaline, which is a pregnancy category B drug).
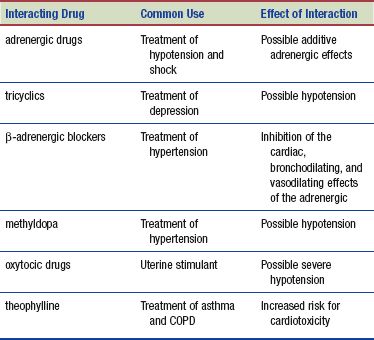
Interactions
The following interactions may occur when an adrenergic drug is used concurrently with another agent:
Xanthine Derivative Bronchodilators
Xanthine derivatives (also called methylxanthines) are a different class of drugs from the adrenergics and also have bronchodilating activity. Examples are theophylline and aminophylline. Additional information concerning the xanthine derivatives is found in the Summary Drug Table: Lower Respiratory System Drugs.
Actions
The xanthine derivatives are drugs that stimulate the central nervous system (CNS) to promote bronchodilation. They cause direct relaxation of the smooth muscles of the bronchi.
Uses
The xanthine derivatives are used for the following:
• Symptomatic relief or prevention of bronchial asthma
• Treatment of reversible bronchospasm associated with chronic bronchitis and emphysema
Adverse Reactions
Central Nervous System Reactions
• Restlessness, irritability, headache
• Nervousness, tremors
Cardiac and Respiratory System Reactions
• Tachycardia
• Palpitations
• Electrocardiographic changes
• Increased respirations
Other Reactions
• Nausea, vomiting, fever
• Hyperglycemia, flushing, alopecia
Contraindications
The xanthine derivatives are contraindicated in those with known hypersensitivity to the drugs, peptic ulcers, seizure disorders (unless well controlled with appropriate anticonvulsant medication), and serious uncontrolled arrhythmias.
Precautions
The xanthine derivatives are used cautiously in patients with cardiac disease, hypoxemia, hypertension, congestive heart failure, and liver disease. They are also used cautiously in older adult patients and those who use alcohol habitually. Aminophylline, dyphylline, oxtriphylline, and theophylline are pregnancy category C drugs and are used cautiously during pregnancy and lactation.
Interactions
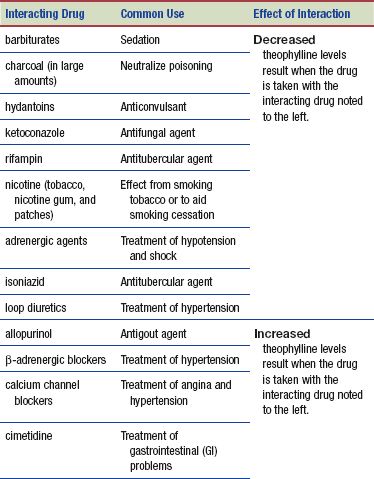
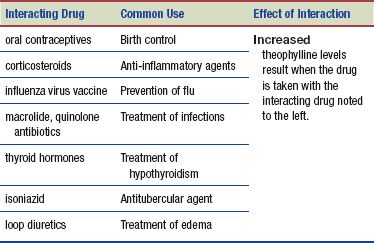
When taken with theophylline, the following agents have an effect on theophylline levels:
Long-term control medications are used daily to achieve and maintain control of persistent asthma. The most effective are those that reduce the underlying inflammation of asthma.
Inhaled Corticosteroids
ICSs are the most consistently effective long-term control medication at all steps of care for persistent asthma. ICS and LABA drugs may be combined to ease administration of the medications and produce positive outcomes in the management of asthma; these ICS/LABA combinations can be found in the Summary Drug Table: Lower Respiratory System Drugs.
Actions
ICSs are anti-inflammatory medications that reduce airway hyperresponsiveness, reduce the number of mast cells in the airway, and block reaction to allergens. ICSs, such as beclomethasone (QVAR) or flunisolide (AeroBid), are given by inhalation and decrease the inflammatory process directly in the airways. In addition, the corticosteroids increase the sensitivity of the β2 receptors, which in turn increases the effectiveness of the β2 receptor agonist drugs.
Uses
The ICSs are used in the management and prophylactic treatment of the inflammation associated with chronic asthma. A number of these preparations may be used intranasally for the treatment of nasal polyps and rhinitis (see Chapter 31).
Adverse Reactions
When used to manage chronic asthma, the corticosteroids are most often given by inhalation. Adverse reactions to the corticosteroids are less likely to occur when the drugs are given by inhalation rather than taken orally. Occasionally, patients may experience reactions.
Respiratory System Reactions
• Throat irritation
• Hoarseness
• Upper respiratory tract infection
• Fungal infection of the mouth and throat
See Chapter 43 for adverse reactions after oral administration of the corticosteroids. A more complete listing of the adverse reactions associated with the ICSs is found in the Summary Drug Table: Lower Respiratory System Drugs.
Contraindications
The ICSs are contraindicated in patients with hypersensitivity to the corticosteroids, acute bronchospasm, status asthmaticus, or other acute episodes of asthma. Beclomethasone is contraindicated for the relief of symptoms that can be controlled by a bronchodilator and other nonsteroidal medications and in the treatment of nonasthmatic bronchitis.
Precautions
The ICSs are used cautiously in patients with compromised immune systems, glaucoma, kidney disease, liver disease, convulsive disorders, and diabetes. Combining ICSs with systemic corticosteroids can increase the risk of hypothalamic-pituitary-adrenal (HPA) suppression, resulting in adrenal insufficiency. These drugs are also used with caution during pregnancy (pregnancy category C) and lactation (pregnancy category B—budesonide).
 NURSING ALERT
NURSING ALERT
During periods of stress or a severe asthmatic attack, patients who have been withdrawn from systemic corticosteroids should be instructed to resume systemic steroids immediately and to contact the primary health care provider. Patient deaths can result from adrenal insufficiency that may occur during and after transfer from systemic corticosteroids to inhaled corticosteroids.
Interactions
Ketoconazole may increase plasma levels of budesonide and fluticasone.
Mast Cell Stabilizer
Cromolyn (Intal) is a mast cell stabilizer.
Actions
Although its action is not fully understood, this drug is thought to stabilize the mast cell membrane, possibly by preventing calcium ions from entering mast cells, thus preventing the release of inflammatory mediators such as histamine and leukotrienes.
Uses
The mast cell stabilizer is used in combination with other drugs in the treatment of asthma and allergic disorders, including allergic rhinitis (nasal solution). It is also used to prevent EIB. They are typically used in Step 2 care for chronic asthma (see Display 32.1).
Adverse Reactions
Respiratory System Reactions
• Throat irritation and dryness
• Unpleasant taste sensation
• Cough or wheeze
This drug may cause a nauseated feeling. A more complete listing of the adverse reactions associated with the mast cell stabilizer is found in the Summary Drug Table: Lower Respiratory System Drugs.
Contraindications and Precautions
The mast cell stabilizer is contraindicated in patients with known hypersensitivity to the drugs and during attacks of acute asthma, because they may worsen bronchospasm during the acute asthma attack.
A mast cell stabilizer is used cautiously during pregnancy (pregnancy category B) and lactation and in patients with impaired renal or hepatic function.
Interactions
No significant drug interactions have been reported.
Leukotriene Modifiers and Immunomodulators
Leukotriene receptor antagonists include montelukast (Singulair) and zafirlukast (Accolate). Zileuton (Zyflo) is classified as a leukotriene formation inhibitor. Omalizumab (Xolair) is a monoclonal antibody used in the treatment of asthma. Additional information concerning these drugs is found in the Summary Drug Table: Lower Respiratory System Drugs.
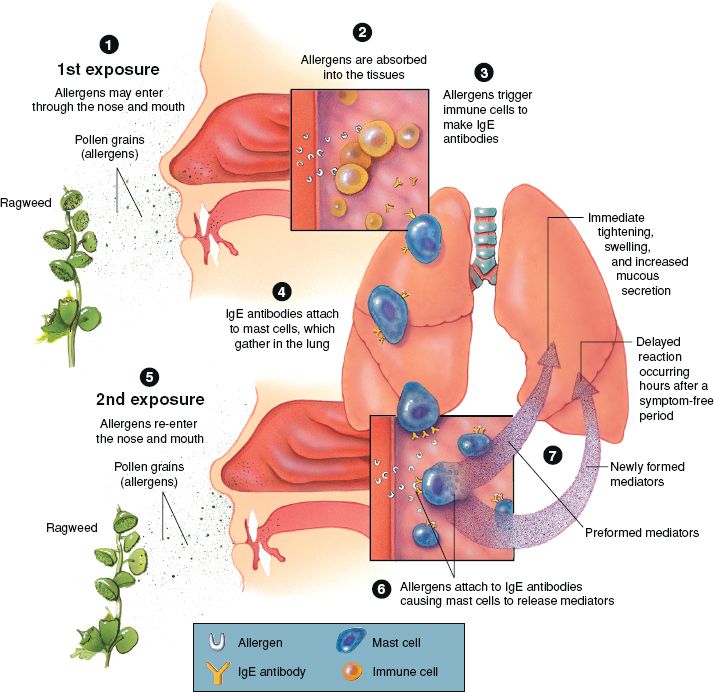
Actions
Asthma attacks are often triggered by allergens or exercise. Inflammatory substances called leukotrienes are one of several substances that are released by mast cells during an asthma attack. Leukotrienes are primarily responsible for bronchoconstriction. When leukotriene production is inhibited, bronchodilation is facilitated. Zileuton (an inhibitor) acts by decreasing the formation of leukotrienes. Although the result is the same, montelukast and zafirlukast work in a manner slightly different from that of zileuton. Montelukast and zafirlukast are considered leukotriene receptor antagonists because they inhibit leukotriene receptor sites in the respiratory tract, preventing airway edema and facilitating bronchodilation. Omalizumab modulates the immune response by preventing the binding of immunoglobulin to the receptors on basophils and mast cells, thereby limiting the allergic reaction. The action of these drugs is illustrated in Figure 32.2, which shows how exposure to an allergen triggers the antibody response in the respiratory system.
Figure 32.2 Exposure to allergen and immune response.
Uses
Leukotriene modifiers are used in the prophylaxis and treatment of chronic asthma in adults and children older than 12 years. Omalizumab is used as adjunctive therapy for patients 12 years of age and older who are sensitive to allergens (e.g., dust mites, cockroaches, cat or dog dander) and who require Step 5 or 6 care (see Display 32.1).
Adverse Reactions
• CNS reaction includes headache.
• Generalized body system reactions include flu-like symptoms.
• Immunomodulators may cause anaphylactic reactions.
• Emergency equipment should be available when administering this medication.
Contraindications and Precautions
These drugs are contraindicated in patients with known hypersensitivity, bronchospasm in acute asthma attacks, or liver disease (zileuton). They should be used cautiously in pregnancy and not at all during lactation (zafirlukast, montelukast, and omalizumab are pregnancy category B drugs and zileuton is a pregnancy category C drug).
Interactions
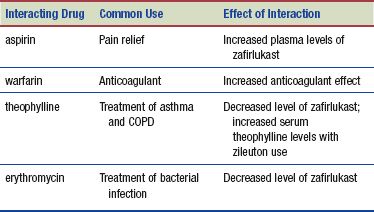
The following interactions may occur when a leukotriene modifier is administered with another agent:
NURSING PROCESS
PATIENT RECEIVING A LOWER RESPIRATORY SYSTEM DRUG
ASSESSMENT
Preadministration Assessment
Because the bronchodilators or antiasthma drugs may be given for asthma, emphysema, or chronic bronchitis, the preadministration assessment of the patient requires careful observation and documentation. Many respiratory problems are chronic conditions with acute exacerbations. Quick recognition and immediate action are essential in treating acute breathing problems. Long-term control of respiratory conditions consists of assessment and monitoring, patient education, environmental control, and medication management. Patients are encouraged to use asthma action plans for daily self-management and for acute respiratory exacerbations (see Fig. 32.4).
In situations of acute breathing distress, take the blood pressure, pulse, and respiratory rate before therapy with a bronchodilator or antiasthma drug. Respiratory rates below 12 breaths/min or above 24 breaths/min are considered abnormal. It is important to assess the lung fields and carefully document the sounds heard before therapy is begun. Note any dyspnea, cough, wheezing, “noisy” respirations, or use of accessory muscles when breathing. If the patient is raising sputum, document a description of the sputum. It is also important to record nonrespiratory signs of hypoxia, such as mental confusion, restlessness, anxiety, and cyanosis (bluish discoloration of the skin and mucous membranes). In some instances, the primary health care provider may order arterial blood gas analysis or pulmonary function tests.
If the patient is able to talk comfortably, ask about possible triggers of the asthma attack causing the inability to breathe. Figure 32.3 illustrates common triggers of asthma. Has the patient been around different environmental items, such as a new pet or changes in environmental temperature? Has the patient been under undue stress either physically or emotionally? Has the patient been monitoring lung function with a peak flow meter, and has a change been noted?
Ongoing Assessment
During an acute attack, assess the respiratory status about 30 minutes after a drug is administered or every 4 hours as the patient returns to a normal breathing pattern (or more often if needed). Note the respiratory rate, lung sounds, and use of accessory muscles in breathing. Additionally, keep a careful record of the intake and output and report any imbalance, which may indicate a fluid overload or excessive diuresis.
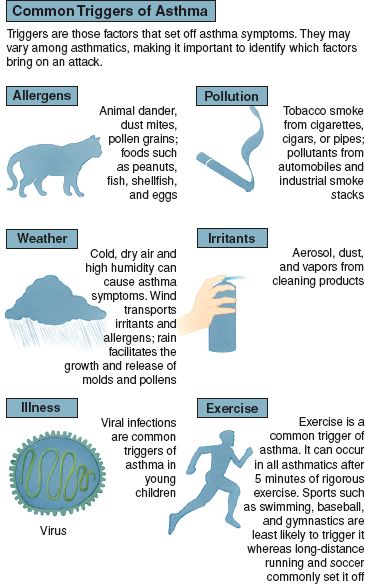
Figure 32.3 Common triggers of asthma. (Courtesy of Anatomical Chart Co.)
During stable chronic phases the patient assumes responsibility to monitor for changes. When an asthma action plan is used, the primary health care provider prescribes daily medications for the patient as well as quick-relief medications. The patient in turn monitors for symptoms such as wheezing and coughing, peak flow meter changes, and triggers that might be making the asthma worsen. During follow-up sessions ask the patient about changes seen on the asthma action plan.
Action plans use a “traffic signal” approach to monitoring breathing status (Fig. 32.4). Has the patient’s condition stayed within the parameters of the green zone or has the patient’s status moved to the yellow or red zones? It is important to monitor any patient with a history of cardiovascular problems for chest pain and changes in the electrocardiogram. The primary health care provider may order periodic pulmonary function tests, particularly for patients with emphysema or bronchitis, to help monitor respiratory status.
NURSING DIAGNOSES
Drug-specific nursing diagnoses include the following:
 Anxiety related to feelings of breathlessness
Anxiety related to feelings of breathlessness
 Ineffective Airway Clearance related to bronchospasm
Ineffective Airway Clearance related to bronchospasm
 Impaired Oral Mucous Membranes related to dryness or irritation
Impaired Oral Mucous Membranes related to dryness or irritation
 Imbalanced Nutrition: Less Than Body Requirements related to decreased appetite caused by nausea, heartburn, or unpleasant taste
Imbalanced Nutrition: Less Than Body Requirements related to decreased appetite caused by nausea, heartburn, or unpleasant taste
Nursing diagnoses related to drug administrations are discussed in Chapter 4.
PLANNING
The expected outcomes for the patient depend on the specific reason for administering the drug but may include an optimal response to therapy, support of patient needs related to managing adverse reactions, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
Nursing care of the patient receiving a bronchodilating drug or an antiasthma drug requires careful monitoring of the patient and instruction for proper administration of the various drugs. These drugs may be given orally, parenterally, or topically by inhalation or nebulization. Dosages are individualized for each patient, which allows the smallest effective dose to be given.
ACUTE SYMPTOM INTERVENTIONS. SABA bronchodilators are used to treat acute respiratory symptoms. Instruct the patient to administer 2 to 4 puffs of the inhaled medication when acute distress occurs. Depending on the severity of the exacerbation, up to three treatments at 20-minute intervals may be administered. A nebulizer may be ordered to deliver the medication rather than an inhaler device. These treatments are given less frequently.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Older adults taking the adrenergic bronchodilators are at increased risk for adverse reactions related to both the cardiovascular system (tachycardia, arrhythmias, palpitations, and hypertension) and the CNS (restlessness, agitation, and insomnia).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree