Leydig Cell Tumors
Steven S. Shen, MD, PhD
Mahul B. Amin, MD
Jae Y. Ro, MD, PhD
Key Facts
Terminology
Pure testicular stromal tumor composed of cells that recapitulate normal interstitial Leydig cells
Clinical Issues
Most common type of sex cord stromal tumor (1-3% of testicular neoplasms)
Majority have benign behavior; 10% malignant
Macroscopic Features
Well-circumscribed, intraparenchymal nodule with golden-brown to yellow, or gray-white homogeneous cut surface
Microscopic Pathology
Growth patterns: Solid (most common), insular, tubular, ribbon-like, and pseudofollicular
Large, round or polygonal cells with well-defined cell borders, eosinophilic or vacuolated cytoplasm
Relatively uniform round or ovoid nuclei, prominent nucleoli; focal nuclear pleomorphism, binucleated or multinucleated cells may be seen
Cytoplasmic vacuoles or foamy cytoplasm (lipid content), lipofuscin (15%), and Reinke crystals (30-40%) may be seen
Other uncommon features: Fatty metaplasia; spindle, clear cell, or microcystic changes; myxoid degeneration; calcification or ossification; and rhabdoid features
Ancillary Tests
Positive for inhibin-α, calretinin, Melan-A(MART-1), and vimentin (strong and diffuse)
TERMINOLOGY
Abbreviations
Leydig cell tumor (LCT)
Synonyms
Interstitial cell tumor
Definitions
Pure testicular stromal tumor composed of cells that recapitulate normal interstitial Leydig cells
CLINICAL ISSUES
Epidemiology
Incidence
Most common type of sex cord stromal tumor (1-3% of testicular neoplasms)
Age
Occurs in any age with 2 peaks: 5-10 & 30-35 years
Presentation
Testicular enlargement, usually painless, decreased libido (20%), gynecomastia (15%), undescended testis (10%), or precocious puberty
May produce testosterone, androstenedione, and dehydroepiandrosterone
May be associated with cryptorchidism, testicular atrophy, infertility
Bilaterality in 3% of cases
Treatment
Surgical approaches
Orchiectomy is curative in majority of tumors; baseline staging work-up is required
Retroperitoneal lymph node dissection may be required in older patients and those with tumors with unfavorable histology
Testis-sparing surgery possible for young men
Prognosis
Majority have benign behavior
Approximately 10% malignant and may metastasize
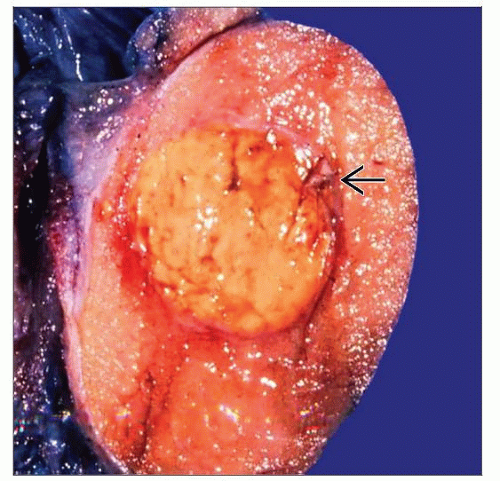
MACROSCOPIC FEATURES
General Features
Well-circumscribed, intraparenchymal mass with golden-brown to yellow, or gray-white homogeneous cut surface
Focal hemorrhage or necrosis may be seen (25%)
Most confined within testis; extratesticular extension possible (10%)
Size
Range: 1-10 cm (average: 3 cm)
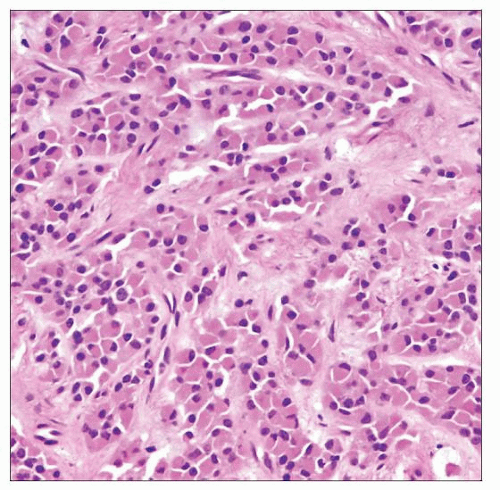
MICROSCOPIC PATHOLOGY
Histologic Features
Growth patterns: Solid (most common), insular, tubular, ribbon-like, and pseudofollicular
Large, round or polygonal cells with well-defined cell borders, eosinophilic or vacuolated cytoplasm
Relatively uniform round or ovoid nuclei, prominent nucleoli; focal nuclear pleomorphism (including endocrine-type), binucleated, or multinucleated cells may be seen
Cytoplasmic vacuoles or foamy cytoplasm (lipid content), lipofuscin (15%), and Reinke crystals (30-40%) may be seen
Frequent fibrous, hyalinized, edematous or myxoid stroma
Other uncommon features: Fatty metaplasia; spindle, clear cell, or microcystic changes; myxoid degeneration; calcification or ossification; and rhabdoid features
Features that tend to be seen more often in malignant tumors: Large tumor size (> 5 cm), infiltrative margins, vascular invasion, nuclear atypia, necrosis, high mitotic rate (> 3/10 high-power fields)
Cytologic Features
Large, round or polygonal cells with prominent nucleoli, abundant eosinophilic cytoplasm, and well-defined cell borders
Predominant Pattern/Injury Type
Diffuse and solid neoplastic growth
Predominant Cell/Compartment Type
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree