Kikuchi-Fujimoto Disease
Carlos E. Bueso-Ramos, MD, PhD
Key Facts
Clinical Issues
Self-limited clinical course in most patients
Might represent phenotype of diverse disease entities
Prognosis is different according to underlying cause
Young patients
Acute tender cervical lymphadenopathy
Low-grade fever; systemic symptoms
Systemic survey and follow-up is recommended to rule out systemic lupus erythematosus
Microscopic Pathology
Multiple, pale circumscribed foci are found in paracortical area of lymph node
Lack of extension of process into perinodal tissue
3 phases: Proliferative, necrotizing, xanthomatous
Lesions are composed of mononuclear cells with round to irregular nuclei
Abundant karyorrhectic debris
Plasmacytoid dendritic cells are present
Paracortical areas of coagulative necrosis are seen
Large numbers of histiocytes, including crescentic histiocytes and activated lymphoid cells
Absence of neutrophils
Ancillary Tests
Predominance of CD3(+), CD8(+) T cells
Histiocytes express myeloperoxidase, lysozyme and CD68
↑ plasmacytoid dendritic cells expressing CD68, CD123, CD303
No evidence of monoclonal Ig or TCR rearrangements
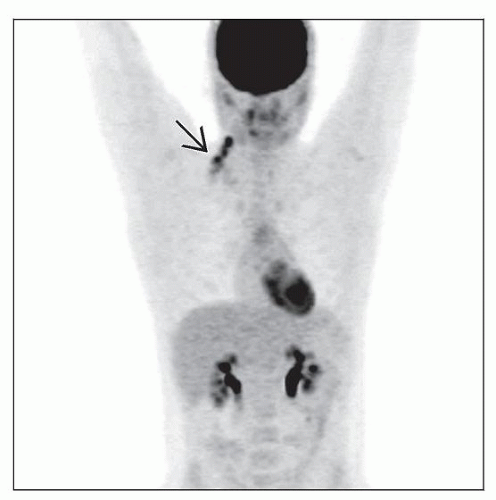
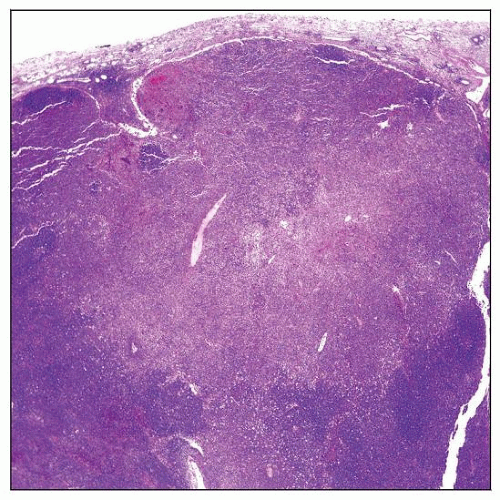 Cervical lymph node involved by Kikuchi-Fujimoto disease. The paracortex shows a circumscribed, wedgeshaped area of necrosis that extends to the capsule. |
TERMINOLOGY
Abbreviations
Kikuchi-Fujimoto disease (KFD)
Synonyms
Necrotizing lymphadenitis without granulocytic infiltration
Histiocytic necrotizing lymphadenitis
Kikuchi-Fujimoto lymphadenopathy
Definitions
Self-limited, benign form of lymphadenopathy characterized by
Proliferation of histiocytes and plasmacytoid monocytes
Apoptosis with abundant karyorrhectic debris
Systemic symptoms and low-grade fever in subset of patients
ETIOLOGY/PATHOGENESIS
Unknown
Viral, infectious, or autoimmune cause has been suggested
Exuberant T-cell-mediated response to variety of stimuli in genetically susceptible people
Cytokine-mediated mechanisms
↑ interleukin-6, interferon-α, FAS ligand
Viruses suggested to be involved in KFD include
Epstein-Barr virus (EBV) and human herpes virus 6 (HHV6)
Identified in small subset of cases; unlikely to be cause
CLINICAL ISSUES
Epidemiology
Age
Usually < 30 years (range: 2-75 years)
Gender
Women are affected more often
Female to male ratio is 4:1
Ethnicity
KFD has been described in a variety of ethnic backgrounds
Asian descent most common
Site
Lymphadenopathy
Cervical lymph nodes most often involved
Presentation
Fever typically lasts for 1 week
Can persist for up to 1 month
Upper respiratory symptoms
Most common initial manifestations are
Tender and painful lymphadenopathy
Lymphadenopathy with fever
Uncommon manifestations
Weight loss, night sweats, nausea, vomiting
Generalized lymphadenopathy
Joint pain
Extranodal involvement by KFD
Splenomegaly, hepatomegaly
Laboratory Tests
Rule out other causes of necrotizing lymphadenopathy
No specific tests are available for detecting KFD
Anemia
Elevated lactate dehydrogenase levels
Granulocytopenia and atypical lymphocytosis in peripheral blood (50%)
Elevated erythrocyte sedimentation rates
Polyclonal hypergammaglobulinemia
Negative serologic studies for
EBV, Cytomegalovirus, influenza, adenovirus
Toxoplasmosis, Mycoplasma, Q fever
Usually negative autoimmune laboratory studies
Antinuclear antibodies, rheumatoid factor, antidouble-strand DNA antibodies
Rare patients with KFD are subsequently diagnosed to have systemic lupus erythematosus
Natural History
Diagnosis is usually established by lymph node biopsy
Excisional biopsy is often required because KFD can be patchy
Assessment of lymph node architecture is very helpful in establishing diagnosis
Spontaneous resolution occurs, usually within 1-4 months
Small (˜ 3%) subset of patients develop relapse
Treatment
No specific therapy required
Anti-inflammatory agents
Prognosis
Excellent
IMAGE FINDINGS
CT Findings
Computed tomography (CT) is preferred modality
Cervical lymph nodes in KFD tend to be located in posterior triangle
Lymph nodes appear as clusters
< 4 cm in greatest dimension
Nonenhancing necrosis
Any lymph node group can be involved in KFD
MACROSCOPIC FEATURES
General Features
Size: 0.5-4.0 cm
MICROSCOPIC PATHOLOGY
Histologic Features
Lymph node
Architecture: Partial or extensive involvement
Often patchy in early stages
KFD begins in paracortex and near capsule
Degree of apoptosis/necrosis varies from one case to another
No granulocytes identified in necrotic areas
Plasma cells usually absent or rare
Process does not extend into perinodal tissues
Immunoblasts are numerous in viable paracortex contiguous with necrosis
No hematoxylin bodies identified
Sinuses are patent or compressed
Can be filled by histiocytes or monocytoid B cells
Hyperplastic lymphoid follicles in uninvolved areas
± thrombosed blood vessels
3 histologic subtypes of KFD have been described
Lymphohistiocytic/proliferative; thought to be early stage
Necrotic
Phagocytic/foamy cell; thought to be late stage
> 1 stage of KFD can be present within lymph node
Lymphohistiocytic/proliferative type
Proliferation of histiocytes (including C-shaped forms)
Increased plasmacytoid dendritic cells
Small lymphocytes and immunoblasts are present
Relatively little apoptosis or necrotic debris
Necrotic type
Abundant apoptosis within distinct foci of necrosis associated with eosinophilic debris
Histiocytes and plasmacytoid dendritic cells undergo apoptosis
Fibrin thrombi may be present in blood vessels
Phagocytic/foamy cell type
Cytologic Features
Diagnosis can be suggested in touch imprints of lymph node
Highlights cytologic characteristics of plasmacytoid dendritic cells (pDC)
Touch imprint often better than fine needle aspiration (FNA) smears
Frequency of CD123(+) pDC is high in KFD
Valuable indicator for diagnosis of KFD
Useful for distinguishing KFD from reactive lymphadenopathy and neoplasms
Skin
Most frequently located on face or upper body
KFD in skin can grossly present as
Erythematous papules
Indurated lesions or plaques
Ulcers
Histologic findings in skin include
Dermal lymphohistiocytic infiltrate; most common
Epidermal changes
Necrotic keratinocytes
Nonneutrophilic karyorrhectic debris
Basal vacuolar change
Edema of papillary dermis
ANCILLARY TESTS
Immunohistochemistry
Histiocytes are CD4(+), CD68(+), lysozyme(+), myeloperoxidase(+, dim)
Plasmacytoid dendritic cells are
CD68(+), CD123(+), CD303(+)
Myeloperoxidase(-), fascin(-)
T cells are predominantly CD8(+)
Immunoblasts are CD30(+) and of CD8(+) T-cell lineage
B cells are rare or absent in areas of necrosis
Flow Cytometry
Predominance of CD8(+) T cells without aberrancies
Rare polytypic B cells
Insufficient to establish diagnosis of KFD
Helpful to exclude non-Hodgkin lymphoma
PCR
No evidence of monoclonal IgH gene rearrangements
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree