Invasive Micropapillary Carcinoma
Key Facts
Terminology
Invasive micropapillary carcinoma (IMPC)
Special histologic subtype of infiltrating ductal carcinoma
Clinical Issues
Increased incidence of lymph node metastases and local recurrence
40-50% of patients with IMPC will present with ≥ 4 positive axillary nodes
Microscopic Pathology
Infiltrating clusters of tumor cells surrounded by clear spaces
Micropapillary pattern may predominate or represent minor component of tumor
Tumor likely grows as spherules rather than as micropapillae
Clusters frequently have central hollow space
Immunohistochemistry for EMA or MUC1 can support diagnosis
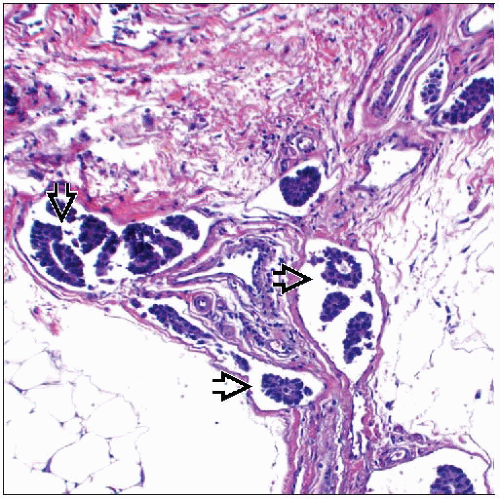
Lymphvascular invasion is commonly seen
Associated with increased nodal metastases
IMPC of breast morphologically similar to micropapillary tumors of bladder, lung, ovary, and salivary glands
Top Differential Diagnoses
Metastatic micropapillary carcinoma
Finding DCIS supports diagnosis of breast primary
Mucinous carcinoma
Invasive ductal carcinoma with tissue retraction artifact
TERMINOLOGY
Abbreviations
Invasive micropapillary carcinoma (IMPC)
Definitions
Type of invasive carcinoma with distinctive pattern of tumor cell clusters growing in individual empty-appearing spaces
Cell clusters often have hollow core with apical aspect of cells facing outward
ETIOLOGY/PATHOGENESIS
Comparative Genomic Hybridization Studies
IMPC exhibits losses involving short arm of chromosome 8 (8p)
88% show chromosomal gains of 8q
Findings suggest that this morphologic phenotype is related to 1 or more genes on chromosome 8
Loss of heterozygosity reported on 17p13.1 in 80% of patients with IMPC
MYC (8q24) amplification significantly associated with IMPC
MUC1 Expression
Apical or secretory pole of cell directed toward outside of cell cluster (“reversed polarity”)
IMPCs show MUC1 expression at periphery/surface of tumor cell clusters
MUC1 has inhibitory effect on epithelial/stroma interaction
MUC1 expression on surface may aid in detachment of tumor cells from stroma and facilitate spread
Gene Expression Profiling
IMPCs cluster together indicating a common pattern of gene expression
Identified as member of luminal A group of cancers
CLINICAL ISSUES
Epidemiology
Incidence
Relatively rare form of infiltrating breast cancer
Only 3.8% of a large breast cancer series
Pure IMPC less frequently seen (˜ 1%)
Mixed lesion with IMPC component more common
Tumors with mixed pattern including IMPC component are important to recognize
Prognostic significance holds true even for minor IMPC component
Age
Broad age range at presentation
Mean: 55 years
Site
Distribution within breast does not differ compared with other forms of carcinoma
More commonly multifocal (approximately 30%) compared to other carcinoma types
May be related to propensity for lymph-vascular invasion resulting in intramammary metastasis
Presentation
Palpable mass; most common presentation
Mammographic density
Calcifications may be associated with carcinoma
Increased incidence of axillary nodal involvement at presentation (70-95%)
Lymph node metastases occur in majority of IMPC < 1 cm in size
Prognosis
IMPC has more aggressive clinical course compared to breast cancers of no special type
Decreased disease-free and overall survival
Increased incidence of local recurrence
Recurs in ˜ 22% of patients compared to ˜ 12% of patients with carcinomas of no special type
Increased incidence of lymph node metastases
40-50% of IMPCs will present with ≥ 4 positive axillary nodes
Lymph node metastases are common even with smaller tumors (< 1 cm)
Therefore, patients with IMPC are more likely to present at higher stages than patients with carcinomas of no special type
When matched by stage, IMPC has similar survival compared to other cancer types
Core Needle Biopsy
Micropapillary pattern on core needle biopsy is predictive of a higher likelihood of lymph node metastasis
IMAGE FINDINGS
Mammographic Findings
Irregular or circumscribed mass
Microcalcifications may be present
MACROSCOPIC FEATURES
General Features
Typically firm solitary mass with ill-defined margins grossly
Cut surface usually solid and white or white-gray
Tumors are multifocal in about 30% of cases
Size
Tumors range in size from 0.7-10 cm
Median: 2.8 cm
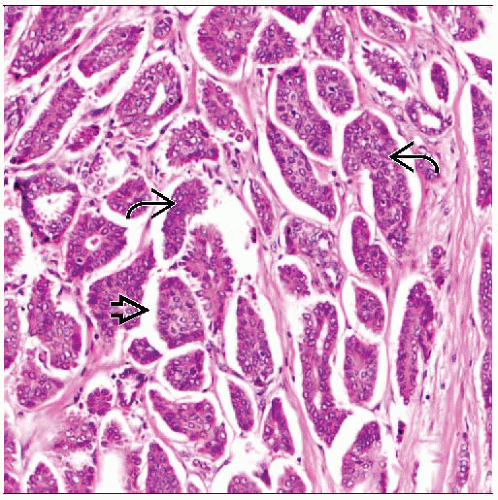
MICROSCOPIC PATHOLOGY
Histologic Features
“Micropapillary” may be a misnomer
Papillae are never seen in cross section
It is likely tumor grows as hollow spherules of cells
Similar to appearance of tumor cells in malignant effusions in cross section
Same pattern is seen in lymphatics and in lymph nodes
Numerous small clusters of tumor cells
Many tumor cell clusters are hollow without fibrovascular cores
Other clusters appear to be solid
Peripherally located nuclei may bulge out with knobby appearance
Apical blebs are found on outer surface of clusters
Clusters of tumor cells are surrounded by clear spaces
Low-power appearance resembles “fallen leaves” or has a spongy look
1 or only a few tumor cell clusters seen per space
Spaces usually clear; however, scant mucin occasionally present
Spaces surrounded by loose fibrocollagenous stroma
May mimic lymph-vascular involvement
Clusters of tumor cells are characterized by reversed polarity
Apical (secretory) pole of cells is directed toward outside of cell groups (not into a lumen or central empty space)
May contribute to ability to invade vascular lymphatic spaces
EMA, E-cadherin, and MUC1 are positive on periphery of tumor cell clusters, highlighting reverse polarity
Neoplastic cells are predominantly polygonal in shape or pleomorphic
Frequently intermediate to high nuclear grade
Nuclear pleomorphism, hyperchromasia, and macronucleoli typical
Abundant finely granular, eosinophilic, or vacuolated cytoplasm
Distinctive cell borders
Micropapillary pattern may predominate (pure IMPC) or represent a minor component
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree