Introduction to Pathophysiology
Lee-Ellen C. Copstead
Key Questions
• How are etiology and pathogenesis used to predict clinical manifestations and response to therapy?
• How are normal and abnormal physiologic parameters defined?
• What general factors affect the expression of disease in a particular person?
![]()
http://evolve.elsevier.com/Copstead/
Pathophysiology derives from the intersection of two older, related disciplines: pathology (from pathos, suffering) and physiology (from physis, nature). Pathology is the study and diagnosis of disease through examination of organs, tissues, cells, and bodily fluids. Physiology is the study of the mechanical, physical, and biochemical functions of living organisms. Together, as pathophysiology, the term refers to the study of abnormalities in physiologic functioning of living beings.
Pathophysiology seeks to reveal physiologic responses of an organism to disruptions in its internal or external environment. Because humans exhibit considerable diversity, healthy structure and function are not precisely the same in any two individuals. However, discovering the common and expected responses to abnormalities in physiologic functioning is useful, and it allows a general prediction of clinical progression, identification of possible causes, and selection of interventions that are most likely to be helpful. Thus, pathophysiology is studied in terms of common or “classic” presentations of disorders.
Historically, descriptions of diseases were based on observations of those individuals who attracted medical attention because they exhibited abnormal signs or complained of symptoms. Over time, cases with similar presentations were noted and treatments that had been successful before were used again. In some cases, similarities among individuals pointed to possible common causes. With the advent of more sophisticated measurements of physiologic and biochemical function, such as blood pressure measurements, blood chemistry values, x-ray images, and DNA analysis, the wide variability in the expression of diseases and disorders in the population became apparent, as did the opportunity to discover diseases at earlier stages, before they were clinically obvious. Screening programs that evaluated large segments of the population revealed the complexity and diversity of disease expression, even in persons with the same genetic defect. Thus, although the study of pathophysiology is necessarily a study of the usual and expected responses of the body to a given disruption, individuals often vary significantly from a classic presentation, making the diagnostic process complex and challenging.
Advances in genomic and epigenomic characterization, innovative technologies, and revolutionary approaches to the analysis of genetic variation and function have made studies and treatments possible that were not even imaginable just a few years ago. As a result, definitions of the living world have been virtually transformed and permeate every branch of biological science. Benefits of this new biology include a deeper understanding of evolution, greater insights into immune mechanisms, and nearly every advance against cancer and acquired immunodeficiency syndrome (AIDS).
Genetic manipulation also raises sensitive and complex ethical and moral questions that did not exist half a century ago. Scientists are able to experiment with genetic manifestations and their mechanisms of action, dramatically altering medical practice, especially the management of inherited diseases. New capabilities have led to experimental treatments such as gene therapy–molecular surgery powerful enough to cure and alter the next generation. The study of pathophysiology assumes even greater significance as genetic research shows fresh insights and hopeful new treatments for human diseases.
Pathophysiology examines disturbances of normal mechanical, physical, and biochemical functions, either caused by a disease or resulting from a disease or abnormal syndrome or condition. For example, the study of a toxin released by a bacterium has evolved from the science of infectious diseases, as well as the harmful effects of that toxin on the body, one possible result being sepsis. Another example is the study of the chemical changes that take place in body tissue as the result of inflammation.
Although individual study of specific diseases undertaken in medical pathology textbooks helps students identify subtle differences between similar diseases, the study of pathophysiology is dynamic and conceptual, seeking to explain processes and relationships common to a number of pathologies. For example, the pathophysiology of inflammation, hypotension, fluid volume deficit, hypoxia, and ischemia is important to the understanding of a large number of different pathologies, but each separate process is not necessarily a specific disease.
Pathophysiology includes four interrelated topics: etiology, pathogenesis, clinical manifestations, and treatment implications—the framework used throughout this textbook. Specific diseases will be used as illustrative examples of conditions in which particular pathophysiologic processes may occur.
Framework for Pathophysiology
Etiology
Etiology, in its most general definition, is the study of the causes or reasons for phenomena.1 A description of etiologic process includes the identification of those causal factors that, acting in concert, provoke a particular disease or injury. When the cause is unknown, a condition is said to be idiopathic. If the cause is the result of an unintended or unwanted medical treatment, the resulting condition is said to be iatrogenic. Most disorders are multifactorial, having several different etiologic factors that contribute to their development. For example, coronary heart disease is a result of the interaction of genetic predisposition, diet, exposure to cigarette smoke, elevated blood pressure, and perhaps numerous other lifestyle and hormonal factors acting in concert. None of these individual factors can be said to cause the disease. When the link between an etiologic factor and development of a disease is less than certain, but the probability is increased when the factor is present, it is termed a risk factor. The identification of risk factors is important for disease prevention and various levels of prevention provide focus for the epidemiology section at the end of this chapter.
Some diseases are closely linked with etiologic factors, such that they are said to be the causative agents in the disease. For example, microbial pathogens are considered to be causative agents for infectious diseases: human immunodeficiency virus causes HIV disease, influenza viruses cause the flu, and Mycobacterium tuberculosis causes pulmonary tuberculosis. These diseases do not occur unless the pathogen is present in the body; however, this does not mean that the infection will have the same consequences in each case, because many host factors affect the clinical course. Even when the link between disease and etiologic agent is strong, only a portion of the population exposed to the factor may develop the disease. For example, in persons who consume large quantities of alcohol and develop liver cirrhosis, it is the alcohol consumption that is considered to be the cause, yet only a portion of persons who drink heavily will develop cirrhosis.2 Thus categorizing the probable etiologies for diseases is a long, difficult research process and, not surprisingly, the exact causes of most disorders remain incompletely understood. Several classification schemes have been proposed to categorize diseases according to etiology. Box 1-1 summarizes an example of an etiologic classification system. No classification system is truly comprehensive and some diseases fall into multiple categories. Some diseases may receive different designations in the future, as further research reveals new data.
Pathogenesis
Pathogenesis refers to the development or evolution of a disease, from the initial stimulus to the ultimate expression of the manifestations of the disease.3 The sequence of physiologic events that occurs in response to an etiologic agent is a dynamic interplay of changes in cell, tissue, organ, and systemic function. As the ways in which intricate intercellular communication networks control physiologic function are discovered, pathogenesis is being increasingly understood on the cellular level. One of the best examples of this communication network is the immune system and its interactions with essentially every other cell in the body. A disruption in the delicate system of checks and balances between immune tolerance of normal cells and immune surveillance for abnormal cells and foreign antigens is at the root of a large number of degenerative and inflammatory diseases.
Pathologic disruptions in cellular behavior lead, in turn, to changes in organ and system function that may be detected by clinical or laboratory examination. Most pathophysiology texts take a systems approach to presenting information. This approach builds on the way in which students learn anatomy and physiology and has its roots in medical specialization. Usually the clinical examination of a patient is also conceptualized by a systems approach. Although the division into systems is useful for dividing the content into conceptual pieces, it is important to remember that the organism functions as an integrated whole and the intercellular communication networks are not confined within single systems. In summary, pathogenesis is a description of how etiologic factors are thought to alter physiologic function and lead to the development of clinical manifestations that are observed in a particular disorder or disease.
Clinical Manifestations
Manifestations of disease that are observed are termed signs of disease. Such objective data may be gathered by clinical examination or by biochemical analysis, diagnostic imaging, and other laboratory tests. The subjective feelings of an abnormality in the body are termed symptoms. By definition, symptoms are subjective and can only be reported by the affected individual to an observer. For example, the feeling of nausea is a symptom, whereas vomiting is objectively observed and is a sign. Some signs and symptoms, such as fever and headache, are nonspecific and, although they designate that something is amiss, they do not indicate a specific cause. In this case further examination and, often, laboratory tests are needed to focus on the possible causes of the signs and symptoms. Many diseases and disorders are characterized by a particular constellation of signs and symptoms, the knowledge of which is essential for accurate detection and diagnosis. When the etiology of a particular set of signs and symptoms has not yet been determined, the disorder may be termed a syndrome. For example, AIDS was originally detected as a set of signs and symptoms related to a deficiency of helper T cells of unknown cause, now known to be a late stage of HIV infection.4
The clinical manifestations of some diseases may change significantly over time, resulting in a completely different clinical presentation at different stages. Knowledge of the possible stages of a disease is helpful in making an appropriate diagnosis and anticipating the clinical course.
Stages and Clinical Course
Early in the development of a disease, the etiologic agent or agents may provoke a number of changes in biological processes that can be detected by laboratory analysis, although no recognition of these changes by the patient has occurred. The interval between exposure of a tissue to an injurious agent and the first appearance of signs and symptoms may be called a latent period or, in the case of infectious diseases, an incubation period. The prodromal period, or prodrome, refers to the appearance of the first signs and symptoms indicating the onset of a disease. Prodromal symptoms often are nonspecific, such as headache, malaise, anorexia, and nausea. During the stage of manifest illness, or the acute phase, the disease reaches its full intensity, and signs and symptoms attain their greatest severity. Sometimes during the course of a disease, the signs and symptoms may become mild or even disappear for a time. This interval may be called a silent period or latent period. For example, in the total-body irradiation syndrome, a latent period may occur between the prodrome and the stage of manifest illness. Another example is syphilis, which may have two latent periods: one occurring between the primary and secondary clinical stages and another occurring between the secondary and tertiary stages.5
A number of diseases have a subclinical stage, during which the patient functions normally, although the disease processes are well established. It is important to understand that the structure and function of many organs provide a large reserve or safety margin, so that functional impairment may become evident only when organ damage has become advanced. For example, chronic renal disease can completely destroy one kidney and partly destroy the other before any symptoms related to a decrease in renal function are perceived.6
The clinical course of a disease is often classified as acute or chronic. An acute condition has relatively severe manifestations but runs a short course measured in hours, days, or a few weeks. A chronic condition lasts for months to years. Sometimes chronic disease processes begin with an acute phase and become prolonged when the body’s defenses are insufficient to overcome the causative agent or stressor. In other cases, chronic conditions develop insidiously and never have an acute phase.
Some diseases (e.g., some types of autoimmune diseases) follow a course of alternating exacerbations and remissions. An exacerbation is a relatively sudden increase in the severity of a disease or any of its signs and symptoms. A remission is an abatement or decline in severity of the signs and symptoms of a disease. If a remission is permanent (sometimes defined as longer than 5 years), the person is said to be cured.
Convalescence is the stage of recovery after a disease, injury, or surgical operation. Occasionally a disease produces a subsequent pathologic condition called a sequela (plural: sequelae). For example, the sequela of an inflammatory process might be scarring. The sequelae of acute rheumatic inflammation of the heart might be scarring and deformation of cardiac valves. In contrast, a complication of a disease is a new or separate process that may arise secondarily because of some change produced by the original problem. For example, bacterial pneumonia may be a complication of viral infection of the respiratory tract.
Treatment Implications
An understanding of the etiology, pathogenesis, and clinical consequences of a particular disorder may suggest, or “imply,” that certain treatments could be helpful. For example, understanding that a person with septic shock has excessive dilation of blood vessels that contributes to hypotension implies that fluid administration would likely be helpful. In contrast, most patients with cardiogenic shock have fluid overload, and hypotension in this case is unlikely to improve with fluid administration. Care must be taken not to rely on theoretical implications when evidence-based treatment recommendations are available. When subjected to evaluation by rigorous randomized clinical trials, many treatments that seem as though they should help based on pathophysiology fail to pass the test of application.
The treatment implications discussed in pathophysiology texts usually are general statements rather than specific prescriptions. For example, the pathophysiology of heart failure is characterized by fluid overload, which implies that diuretic therapy would be useful; however, the exact selection of a drug and the dosing schedule would depend on a number of factors particular to the individual patient. Specific treatment recommendations are beyond the scope of a pathophysiology text and can be found in pharmacology and clinical practice textbooks.
Concepts of Normality in Health and Disease
The ability to measure numerous structural, physiologic, biochemical, and genetic parameters in an individual allows the evaluation of information that is helpful in the diagnosis and monitoring of clinical diseases. Many of these same measures are commonly used to screen for disease or to evaluate the risks of a disease occurring in the future. To determine whether a certain finding is indicative of disease or “abnormal,” it must be compared with what is “normal.” The obviousness of this statement belies the difficulty in determining what is normal and the degree of deviation from normal that would be considered abnormal. Many clinical parameters are evaluated by direct observation by the examiner. Skin color and warmth, quality of pulses, briskness of pupil reactions to light, mental acuity, muscle strength, joint mobility, heart sounds, lung sounds, bowel sounds, balance, psychological affect, and level of consciousness are but a few examples of assessments that are subjectively interpreted based on the examiner’s observations. Deciding whether a clinical finding is normal, a normal variation, or an abnormality indicative of a disorder is essential. Reliability of data obtained from observation is dependent upon the examiner’s skill and experience. Often the clinical examination is not sufficient to determine definitively the underlying pathophysiologic processes, and diagnostic testing is undertaken to provide more information.
Statistical Normality
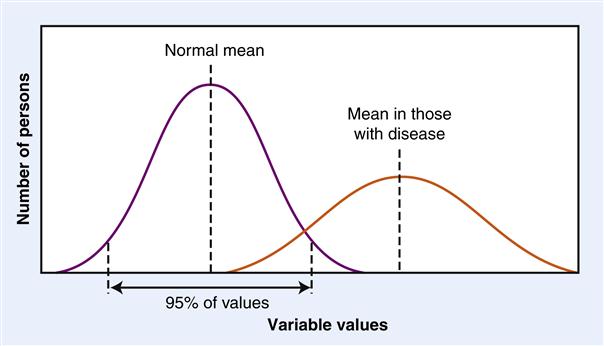
Some of the variables that are measured to diagnose disease are relatively easy to declare as normal or abnormal because they occur in only two states; for example, a bone is either broken or not broken on x-ray examination. However, most diagnostic variables occur in the population according to a “bell curve” or normal distribution.7 This means that a large enough sample taken from the population should give a good estimate of the range of values in the population. Statistics are often used to determine the standard deviation of the variable in question, and then a normal range is suggested as the mean ±2 standard deviations. This means that 95% of the values in the population are expected to fall in the normal range and 5% will be either higher or lower (Figure 1-1). The “population” chosen to serve as the normal reference population must be carefully selected to represent the individual to be tested for disease, because many variables are influenced by age and gender.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree