INTRODUCTION
LEARNING OBJECTIVES
After studying this chapter you should know:
The components of the blood.
The methods used to assess these components.
The identity and function of the major hematopoietic and lymphoid tissues: the bone marrow, spleen, thymus, and lymph nodes.
Regardless of what kind of doctor a student decides to become, a well-grounded understanding of disorders of the blood and the hematopoietic tissues is essential. Primary hematologic disorders are commonly encountered in community and hospital-based clinical practices, and a wide variety of other diseases come to attention by producing secondary abnormalities of the blood. Beyond their everyday clinical importance, studies of hematologic diseases have yielded seminal insights into the molecular pathogenesis of cancer and basic aspects of stem cell biology. These lessons have had far-reaching influences on biomedical research and are beginning to shape the practice of molecular medicine.
The goal of this book is to provide students with a foundation in the area of blood disorders that they can build on as they train to become physicians and/or research scientists. In this chapter, we will commence with a description of the cast of characters—the blood, the primary blood-forming (hematopoietic) tissues, and the secondary hematopoietic tissues that support the maturation and function of some of the elements of the blood—accompanied by a brief description of commonly used laboratory tests. In Chapter 2, the origins of blood cells and the regulation of blood cell production will be discussed in detail. The remainder of the text will then be devoted to specific hematologic disorders.
BLOOD
Normal adult men have about five liters of blood, whereas women average closer to four. The blood has two main components—the blood cells (or formed elements)—and the plasma, the fluid phase of the blood. These two components can be separated from one another by centrifugation at low speed. Red cells are dense and collect in the bottom of the tube, whereas white cells and platelets are of intermediate density and tend to collect at the interface between the red cells and the plasma in a thin gray-white layer referred to as the buffy coat.
Most formed elements can be recognized by their morphologic appearance in smears of whole blood, which can be prepared, stained, and visualized under the light microscope in just a few minutes’ time. In days past, clinicians skilled in the art of morphology could sometimes confirm a suspected diagnosis based on a patient’s history and physical findings through the inspection of blood smears prepared at the bedside. In the modern era, the evaluation of blood is usually left to laboratory technicians and pathologists, but to fully understand blood disorders, students must have a working knowledge of the morphology of the formed elements and their precursors.
The formed elements of the blood are of three major types—red cells (erythrocytes), white cells (leukocytes), and platelets (thrombocytes). The normal values for these cells are listed in Table 1-1.
| Cell Type | No. of Cells (per μL) |
|---|---|
| Red cells | 4.5-6.4 × 106 |
| White cells | 4-10 × 103 |
| Neutrophils | 1.9-7.6 × 103 (48%-76%)† |
| Eosinophils | 0.0-0.5 × 103 (<5%)† |
| Basophils | 0.0-0.2 × 103 (<1.5%)† |
| Monocytes | 0.1-0.8 × 103 (2.5%-8.5%)† |
| Lymphocytes | 0.8-4.1 × 103 (18%-41%)† |
| Platelets | 150-450 × 103 |
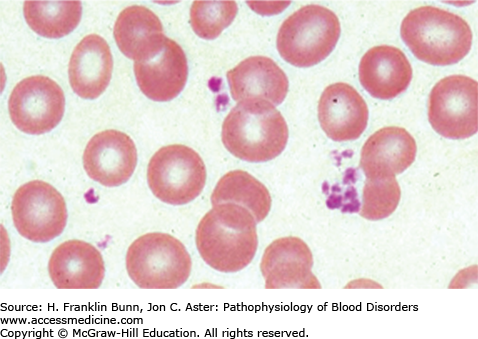
Red cells are the most numerous of the formed elements. In humans they lack nuclei, appearing in smears prepared from peripheral blood as biconcave disks filled with cytoplasm rich in the oxygen-carrying protein hemoglobin (Fig. 1-1). Although simple in appearance and structure, red cells are elegantly designed to fulfill their major functions—the delivery of oxygen from the lungs to the peripheral tissues and the transport of carbon dioxide from peripheral tissues to the lungs for elimination via respiration. Normal red cells have a life span of about 120 days.
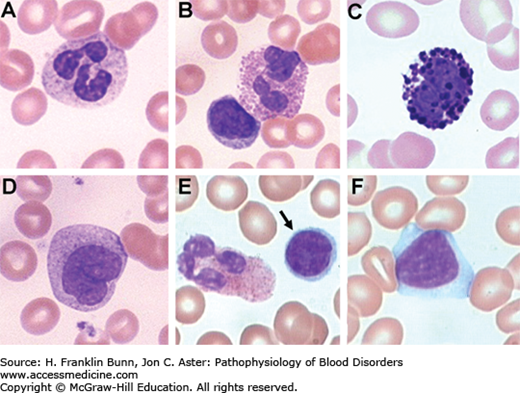
White cells are of several different types (Fig. 1-2). Granulocytes are short-lived, marrow-derived cells that can be distinguished by their appearance in peripheral smears. The most numerous kind is the neutrophil (or polymorphonuclear leukocyte), which has three to five nuclear lobes and moderately abundant cytoplasm containing pale, lilac-colored granules. Neutrophils are phagocytes that provide protection against certain types of acute infections, particularly those caused by bacteria and fungi. They are very short-lived, persisting in the circulation for only a few hours. Eosinophils are cells with two nuclear lobes and abundant red cytoplasmic granules (as befits cells named for Eos, the goddess of dawn). They have an important role in certain chronic immune responses, particularly those associated with helminthic worm infections, asthma, and certain types of allergic reactions. Basophils, the least common granulocyte, have abundant dark blue cytoplasmic granules that obscure their nuclei. Basophils may be slightly increased in number in many of the same conditions that are associated with elevated eosinophil counts. The other types of white cells are so-called mononuclear cells lacking the nuclear segmentation that is characteristic of granulocytes. Monocytes are the largest white blood cell, being 12 to 20 μm in diameter. They are characterized by folded or kidney-shaped nuclei and abundant light blue cytoplasm containing a few small granules. Like neutrophils, monocytes are highly phagocytic, but these cells differ from neutrophils in other important ways. Most notably, upon emigration into tissues, monocytes differentiate into relatively long-lived macrophages, which serve as sentinels capable of detecting “danger” signals produced by infection or tissue injury. Lymphocytes are the key components of the adaptive immune system. They vary widely in size; resting lymphocytes are about the size of normal red blood cells (7-9μm in diameter) and have round, condensed nuclei and scant cytoplasm, whereas activated lymphocytes can be up to 20 μm in size and have enlarged nuclei and abundant cytoplasm, which may contain a few granules. Circulating lymphocytes may be B cells, T cells, or natural killer cells, which can be distinguished from one another reliably only by testing for the presence of certain lineage-specific markers. Some B and T cells (so-called memory cells) may live for years; this longevity is the basis for the immune system’s ability to “remember” exposures to pathogens that occurred many years in the past.
Platelets (thrombocytes) are small, anucleate cell fragments replete with purplish granules that are shed from megakaryocytes in the bone marrow (Fig. 1-1). Together with clotting factors present in the plasma, platelets play a critical role in the regulation of hemostasis. Platelets have a life span of 7 to 10 days. The structure and function of normal platelets are covered in Chapter 14.
As will be discussed in Chapter 2, red cells, platelets, granulocytes, and monocytes originate from a common precursor in the marrow and are referred to as myeloid cells, whereas various kinds of lymphocytes arise from a different common precursor and are referred to as lymphoid cells.
In addition to macrophages, there are a number of other types of bone marrow–derived white cells that exist mainly in tissues. These include osteoclasts, monocyte-derived multinucleated cells that line and resorb bone; plasma cells, terminally differentiated B cells that secrete antibodies and are found mainly in the bone marrow, spleen, lymph nodes, and gut; dendritic cells, specialized antigen-presenting cells; mast cells, tissue cells with dark blue, metachromatic granules that are important in certain types of immune responses, particularly those involving hypersensitivity; and stem cells and progenitor cells, which are the precursors of the formed elements.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree